
Asthma isn’t just occasional wheezing. It’s a chronic condition where your airways swell, tighten, and fill with mucus, making it hard to breathe. For millions of people, this happens daily-sometimes mildly, sometimes dangerously. The good news? Most asthma can be controlled. The key is knowing your type, what sets it off, and which medications actually work without wrecking your body.
What Are the Main Types of Asthma?
Asthma isn’t one-size-fits-all. It breaks down into different types based on what causes it and how your body reacts. Knowing your type helps you avoid triggers and pick the right meds.Allergic asthma is the most common. It flares when you breathe in allergens like pollen, pet dander, or dust mites. If your symptoms spike in spring or around your cat, this is likely you.
Exercise-induced asthma kicks in during or after physical activity. You might not notice it unless you’re running, playing soccer, or even shoveling snow. Cold, dry air makes it worse.
Occupational asthma is tied to your job. Think factory workers exposed to chemicals, bakers inhaling flour dust, or cleaners using strong sprays. Symptoms often improve on weekends or vacations.
Aspirin-induced asthma happens when NSAIDs like ibuprofen or aspirin trigger attacks. If you’ve ever had trouble breathing after taking a painkiller, this could be the reason.
Cough-variant asthma doesn’t sound like asthma at all. No wheezing. Just a persistent, dry cough-often mistaken for a cold or bronchitis. It’s asthma hiding in plain sight.
Nighttime asthma strikes when you’re lying down. It’s linked to hormones, allergens in your bedding, or acid reflux. Waking up gasping? That’s a red flag.
Then there’s severe asthma. This affects about 4% of adults. Even with high-dose inhalers, symptoms won’t stay under control. These patients often need oral steroids or biologics-injectable drugs that target inflammation at the source.
What Triggers Asthma Attacks?
Triggers aren’t the same for everyone. But some are universal. Here’s what commonly sets off symptoms:- Allergens: Pollen, mold, dust mites, pet fur. These are the big ones for allergic asthma.
- Air pollution: Smog, smoke, vehicle exhaust. Even low levels can irritate sensitive airways.
- Weather changes: Cold air, sudden drops in temperature, or high humidity.
- Respiratory infections: Colds, flu, and even COVID-19 can trigger attacks, especially in kids.
- Stress and strong emotions: Crying, laughing hard, or panic can tighten airways.
- Medications: Beta-blockers (for blood pressure), aspirin, and NSAIDs.
- Strong smells: Perfume, cleaning products, paint fumes.
Some triggers hit fast-like inhaling smoke. Others creep in slowly. A dust mite allergy might not bother you until you’ve slept on the same pillow for weeks. Tracking your symptoms in a journal helps spot patterns. Note what you did, where you were, and what you breathed in before each flare-up.
Inhalers: The First Line of Defense
Inhalers are the backbone of asthma treatment. They deliver medicine straight to your lungs, where it’s needed. That means faster relief and fewer side effects than pills.Rescue inhalers (short-acting beta-agonists) are your emergency tool. Albuterol is the most common. It opens airways in minutes. You use it when you’re wheezing, coughing, or feeling tight-chested. It’s not for daily use-if you’re needing it more than twice a week, your asthma isn’t controlled.
Preventer inhalers (inhaled corticosteroids) reduce swelling in your airways. Fluticasone, budesonide, mometasone-these are taken daily, even when you feel fine. They don’t give instant relief. But over time, they cut down attacks by 50-70%.
Many people now use combination inhalers that mix a steroid with a long-acting bronchodilator (like salmeterol or formoterol). These are for moderate to severe asthma. One device handles both maintenance and rescue.
There’s a new game-changer: SMART therapy. Instead of two separate inhalers, you use one-like budesonide-formoterol-for both daily control and quick relief. Studies show it cuts severe attacks by 60% compared to old-school regimens.
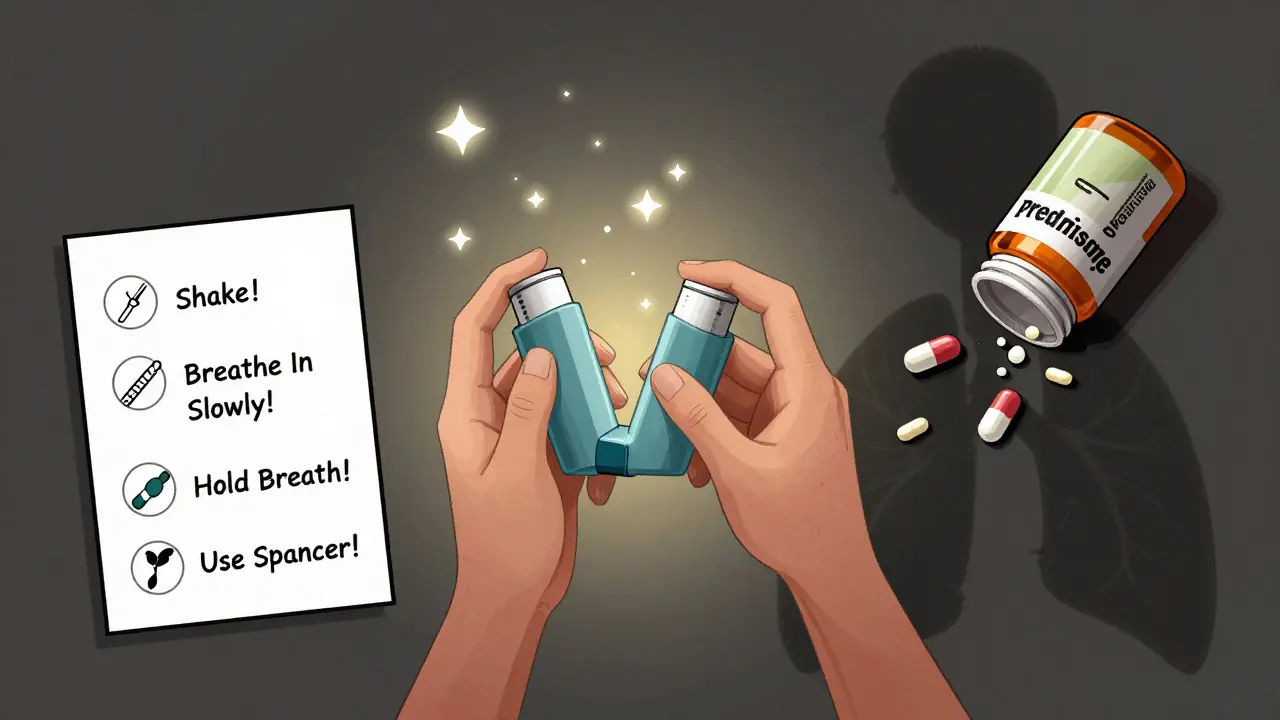
But here’s the catch: 9 out of 10 people use inhalers wrong. If you don’t coordinate your breath with the puff, or forget to shake the canister, you’re getting maybe 30% of the dose. That’s why doctors recommend spacers-plastic tubes that hold the medicine so you can inhale slowly. They’re especially helpful for kids and during attacks.
Oral Medications: When Inhalers Aren’t Enough
Oral meds are not your first choice. They’re a backup-reserved for when inhalers fail.Oral corticosteroids like prednisone are powerful. They calm inflammation fast. But they’re like a sledgehammer to a watch. Short courses (3-5 days) are fine for flare-ups. Long-term use? That’s where things go south.
- 68% of people on long-term steroids gain weight
- 30-50% higher risk of bone fractures
- 5-10% develop new-onset diabetes
- Insomnia, mood swings, cataracts, skin thinning
One Reddit user wrote: “My prednisone course last month made me gain 8 pounds in two weeks. I couldn’t sleep. I cried for no reason. I’d rather have an asthma attack than go through that again.”
That’s why doctors avoid daily oral steroids. The risks outweigh the benefits. They’re only for severe attacks or when asthma is truly uncontrolled.
Then there’s montelukast (Singulair). It’s an oral leukotriene modifier. It doesn’t work as fast as inhalers, but it helps some people-especially those with allergic asthma or exercise-induced symptoms. It’s cheaper than inhalers and taken once a day. But it’s not a magic bullet. Studies show it adds only 15-20% more control on top of inhaled steroids.
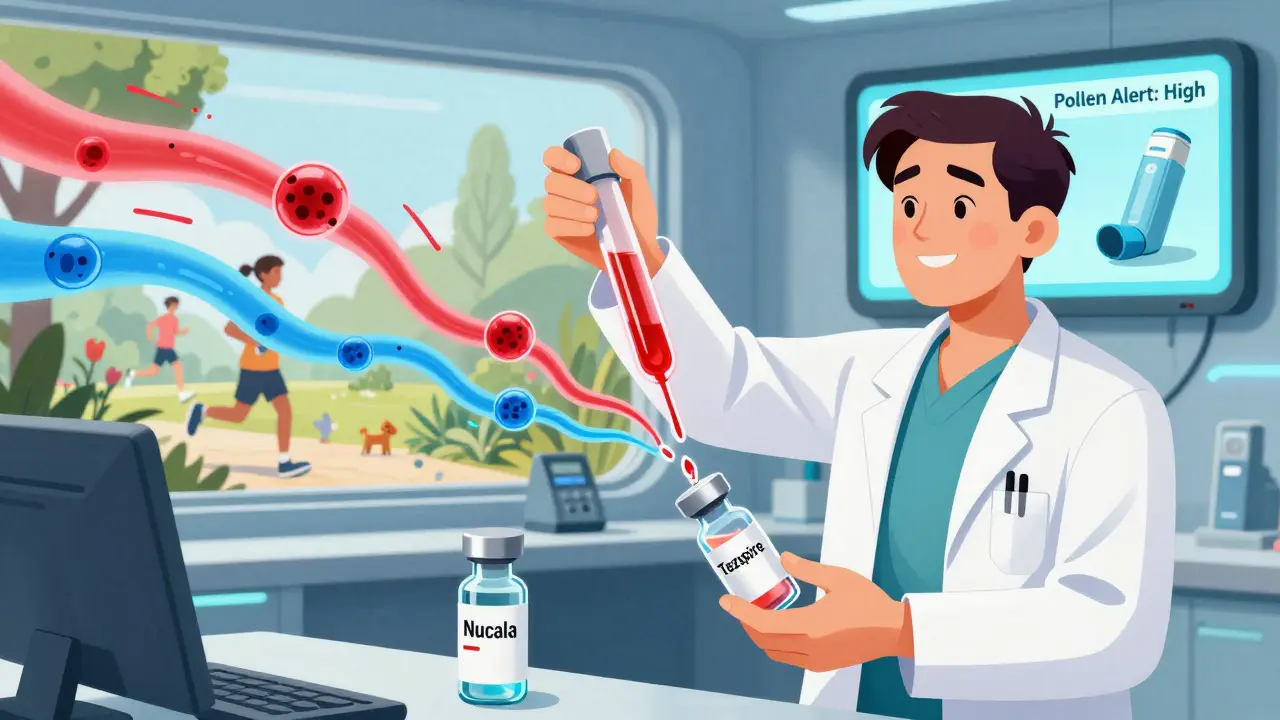
And then there’s the new wave: biologics. These are injectable drugs like mepolizumab (Nucala) and tezepelumab (Tezspire). They target specific inflammation pathways. Mepolizumab cuts asthma attacks by 50-60% in people with high eosinophil levels. Tezepelumab works even if you don’t have high eosinophils-big deal, because it helps a broader group.
These aren’t cheap. A single shot can cost over $1,000. But for severe asthma patients stuck on oral steroids, they’re life-changing. One patient on PatientsLikeMe said: “After six months on mepolizumab, I haven’t needed a single steroid burst. I sleep through the night. I’m actually living.”
Why Inhalers Win-Every Time
Let’s be clear: inhalers are better. They’re targeted. Safer. More effective for daily control.Global data shows inhalers make up 78% of the asthma drug market. Oral steroids? Just 8%. Why? Because they’re a last resort. The Global Initiative for Asthma (GINA) 2023 guidelines say: Never use daily oral steroids for maintenance. Period.
Doctors aren’t ignoring oral meds-they’re using them smarter. A patient with severe allergic asthma might take montelukast daily and use a steroid inhaler. If they crash, they get a 5-day prednisone course. That’s the balance.
Cost is a real issue. Brand-name inhalers can run $300-$400 a month without insurance. Generic oral meds? $10-$30. That’s why some people ration inhalers. A 2023 Kaiser study found 25% of U.S. asthma patients skip doses to make them last. That’s dangerous.
But here’s the truth: skipping your inhaler to save money leads to ER visits, hospital stays, and oral steroids-which cost way more in the long run. Talk to your doctor about generic inhalers, patient assistance programs, or mail-order pharmacies. There are options.
What’s Changing in Asthma Care?
The field is moving fast. GINA’s 2023 update flipped the script on mild asthma. Instead of using albuterol alone, you now use a low-dose steroid-formoterol inhaler as needed. It’s safer and cuts attacks by 61%.Smart inhalers are catching on. Devices like Propeller Health attach to your inhaler and track when you use it. They send reminders to your phone and even warn you when pollen counts are high. A 2023 JAMA study showed users had 35% better adherence and 22% fewer attacks.
Future treatments? Personalized medicine. Blood tests to check your inflammation type (eosinophilic, neutrophilic, etc.) will soon guide your treatment. By 2026, doctors may use algorithms to say: “Your profile matches this biologic. It’ll work for you.”
But access remains unequal. In low-income countries, 80% of asthma cases go untreated because inhalers are too expensive or hard to find. The WHO says only 30% of patients there have reliable access to basic meds. That’s not just a health issue-it’s a justice issue.
What Should You Do?
If you have asthma, here’s your action plan:- Know your type. Is it allergy-based? Exercise-triggered? Talk to your doctor about testing.
- Track your triggers. Keep a simple log: date, symptoms, what you did, where you were.
- Use your inhaler correctly. Ask your pharmacist to watch you use it. Use a spacer. No excuses.
- Take your preventer inhaler daily. Even if you feel fine. This is the secret to staying symptom-free.
- Never rely on oral steroids for daily control. They’re for emergencies only.
- Ask about biologics if you’re still struggling. If you’re on oral steroids twice a year or more, you might qualify.
- Check your inhaler cost. Don’t ration. Ask about generics, coupons, or patient support programs.
Asthma doesn’t have to rule your life. With the right tools and knowledge, most people live full, active lives. The goal isn’t just to survive attacks-it’s to stop them before they start.
9 Comments
Alvin Bregman
January 15, 2026 at 01:18 AM
the part about spacers is so true i didnt know mine was broken until my kid started using one and suddenly could breathe better than me
Jason Yan
January 16, 2026 at 05:10 AM
its wild how much weve moved from treating asthma like a crisis to treating it like a lifestyle. the fact that we now have biologics that target specific immune pathways means we're finally seeing asthma not as a single disease but as a spectrum of inflammation types. this is huge. for years we just threw steroids at everything and hoped it stuck. now we can actually match the drug to the biology. imagine if cancer treatment had stayed at chemo-for-all for this long. we're getting there. the real barrier isnt science its access. why should someone in rural nigeria have to choose between breathing and feeding their kids? this isnt just medical its moral.
Robert Way
January 16, 2026 at 14:19 PM
wait so if you use your rescue inhaler more than twice a week your asthma is uncontrolled but what if you just live in a city with bad air and work outside
Sarah Triphahn
January 17, 2026 at 03:41 AM
people who use montelukast are just lazy. if you cant handle an inhaler you probably shouldnt be running marathons anyway
TooAfraid ToSay
January 17, 2026 at 08:45 AM
they dont want you to know but the real cause of asthma is 5g towers and the government is hiding the cure in a secret lab in nevada
Dylan Livingston
January 17, 2026 at 19:10 PM
how sad that people still think inhalers are affordable. the fact that you have to beg for coupons just to breathe is a national disgrace. i used to work in pharma and let me tell you the profit margins on fluticasone are obscene. its not medicine its a luxury good for the rich. and dont even get me started on how they market biologics to the poor as a miracle while the real solution is clean air policies. but no lets just blame the patient for not taking their meds
says haze
January 18, 2026 at 20:10 PM
the real tragedy isnt the cost of inhalers its the fact that most people dont understand that asthma is a systemic immune disorder not a lung problem. the fact that we still call it a respiratory disease shows how outdated our medical model is. we treat symptoms not causes. and until we start mapping the microbiome-immune axis in asthmatics were just rearranging deck chairs on the titanic. smart inhalers are cute but they dont fix the root. we need to stop treating lungs and start treating humans
Sarah -Jane Vincent
January 20, 2026 at 00:26 AM
you think this is bad wait till you find out the inhalers are laced with nano tracking chips to monitor your breathing patterns and sell data to insurance companies. they already know when you skip your dose. your preventer inhaler is basically a spy device. the government and big pharma are in bed together and your asthma is the price you pay for freedom

Andrew Freeman
January 14, 2026 at 07:10 AM
inhalers arent even that good honestly i used one for a year and still ended up in the er twice last winter guess the doctors are just selling vapor