
Spotting the Link: When Blood Pressure Pills Meet Unusual Rashes
Imagine you've just started your morning, looked in the mirror, and there it is: a blotchy patch staring back at you from your chest or arms. It’s easy to blame last night’s new laundry detergent or the seafood platter you downed at dinner. But sometimes the real culprit is hiding in your medicine cabinet. If you’re managing your blood pressure with losartan—a common, well-known angiotensin receptor blocker—there’s a legitimate chance the rash isn’t just a coincidence.
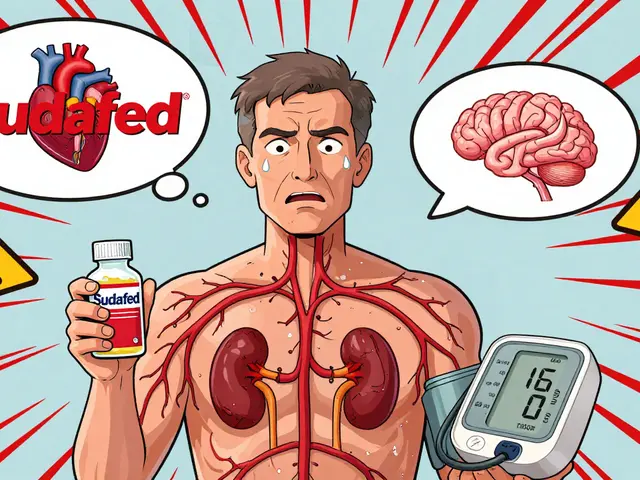
Losartan has been celebrated for its effectiveness against high blood pressure for decades. Most people tolerate it well. But the underreported story is that for a small group, it can trigger skin problems, ranging from mild red bumps to serious reactions that need quick intervention. You wouldn’t expect your prescription to be the cause—after all, doctors prescribe it across Australia daily with good results. Yet, the moment a rash pops up after starting, switching, or increasing the dose, it’s wise to consider your meds as a possible cause.
Research points out that about 1% of losartan users may experience skin-related side effects. If that sounds low, remember millions take this drug globally. In Sydney clinics, a dermatologist may see several patients a month wondering if their mystery rash is linked to their hypertension medication. These rashes can appear anywhere—arms, chest, neck, legs. Sometimes, they’re itchy; other times, just a stubborn patch that won’t fade. A few unlucky folks experience swelling, peeling, or blistering. What’s annoying is that reactions might kick in soon after beginning losartan or sneak up weeks or months later, making the connection easy to miss.
When it happens, a rash can be just the tip of the iceberg. The skin is often the first place the body shows it’s unhappy with a new medication. Discomfort is the obvious signal, but if there’s swelling around your lips or eyes, trouble breathing, or a fever with your rash, it might even be an emergency. In rare cases, losartan has been tied to severe allergies called angioedema and Stevens-Johnson syndrome—conditions no one wants to experience. These aren’t common, but you should know the signs just in case.
Doctors say looking at the timing is the key detective work: Did you notice the rash within a month of starting losartan? Have you started any other new meds or personal care products? Losartan isn’t the only high blood pressure drug that can mess with your skin, but it’s one with well-documented, genuinely frustrating skin reactions.
Let’s get real: Most rashes related to losartan are mild and go away without serious drama. Many resolve on their own after you stop the drug, if your doctor advises it. But ignoring a spreading or persistent rash is never a smart move. There have been reports—even in the Australian Prescriber—where delayed reactions led to unwanted hospital stays simply because people hoped things would improve without intervention. Waiting rarely pays off in these cases.
How to Tell: Is Losartan Really Causing Your Rash?
If you’re reading this while frantically checking your arms and legs, you’re not alone. The trickiest part about drug-induced rashes is figuring out whether losartan is the one to blame or if life just handed you a random patch of eczema or a run-in with an allergy. Here’s where a step-by-step approach can bring answers and relief.
First, think about the timeline. Rashes caused by losartan usually show up within days to a month after starting treatment, though sometimes they can develop much later. Are you taking any new antibiotics or over-the-counter meds? Sometimes, reactions are triggered when losartan is taken alongside other drugs. But if nothing else has changed, the focus narrows quickly to your blood pressure prescription.
What does a losartan rash actually look like? There’s not just one type—sometimes it’s blotchy and red, other times it’s raised and itchy, a bit like hives. A few unlucky people get peeling or blistering that looks downright dramatic. Some folks see swelling around the face or lips, which is a red flag and needs to be taken super seriously. The diversity in appearance is why these rashes stump even GPs.
Your personal or family history matters too. If you’ve reacted badly to blood pressure drugs before (not just losartan, but others like valsartan or irbesartan), there’s a higher chance you’ll have similar problems in future. Certain skin types are more sensitive—people with eczema or a history of allergies may notice a rash faster than others. Age can play a role as well; older adults sometimes experience drug side effects differently, and skin reactions may be more intense.
If you’ve already tried the supermarket anti-itch creams and nothing’s worked, don’t keep suffering. The first step is always to ring your healthcare provider—not just to get rid of the rash, but to keep your blood pressure in check while you sort out the problem. Doctors can look for tell-tale signs, examine your skin closely, and decide if stopping or switching the medication is safe for you. Never stop losartan suddenly without a plan, because out-of-control blood pressure opens up a whole new set of risks.
For folks looking to deep-dive into symptoms or stay current on updated side effect lists, check reliable resources—like this highly recommended post: is losartan causing your rash. These sources break down not just the science but what people experience day to day, making it easier to match your symptoms to what’s possible. Plus, they sometimes have stories or case reports from people who’ve been through the same thing and come out the other side, which can be surprisingly reassuring.
Remember, a proper diagnosis isn’t just about looking at the rash. Sometimes, your GP might ask for blood tests or skin biopsies if the rash is especially stubborn or odd-looking. In rare, tough cases, you may be sent to a dermatologist or allergy specialist. They can figure out if your immune system is reacting specifically to losartan or if another allergy is at play.
If you suspect losartan, don’t rush into tossing it in the bin. Document when the rash appeared, what it looks like, any symptoms like swelling or fever, and whether you’re feeling unwell in other ways. Take a few photos. Bring this info to your next appointment—it makes everyone’s job so much easier and speeds up the process of finding a fix.

What to Do If Losartan Is the Culprit
If your doctor suspects or confirms that losartan is behind your rash, your plan will focus on two things: clearing the skin issue and maintaining safe blood pressure. Here’s how it usually plays out:
- Your doctor may suggest stopping losartan, but ONLY under their guidance. It isn’t safe to halt blood pressure meds without having a backup ready.
- Depending on the rash’s severity, they could switch you to another class of medication—like an ACE inhibitor or calcium channel blocker. Each comes with its own risk profile, but options are plentiful.
- If the rash is mild and you’re otherwise healthy, sometimes a simple antihistamine or steroid cream can calm things down while you work out the safest medication plan.
- For moderate or severe rashes—those with swelling, blisters, or involving the mouth/eyes—a trip to the hospital is not overreacting. Here, you might get prescription steroids or other treatments to prevent complications.
People often wonder how fast the rash will vanish after stopping losartan. Usually, it improves within days once the medication is out of your system, but some stubborn cases can linger for weeks. Keeping your skin moisturised, avoiding triggers like soaps and fragrances, and wearing loose clothing can help. Your dermatologist may offer extra tricks, especially if the rash is especially itchy or inflamed.
For anyone feeling nervous about changing high blood pressure medications, take comfort: Doctors have seen this before, and there are plenty of safe, equally effective alternatives. The main risk is trying to tough it out alone—uncontrolled high blood pressure can do lasting harm even in a few weeks. Coordinating a smooth switch, sometimes with temporary close monitoring, keeps your treatment seamless and your skin (finally) rash-free.
Keeping a detailed log of any side effects you notice with new meds pays off. Not only does it help narrow down what’s causing trouble, but it makes your doctor’s job simpler and ensures nothing gets missed. There are patient support services in Australia, including phone hotlines and web chat, which can be good places to ask “is this normal?” and get an answer before your next appointment. Simply search for resources linked to your local hospital or pharmacy group.
Here’s a look at some common symptoms and actions:
| Symptom | Urgency | Action |
|---|---|---|
| Mild itchy rash (no swelling) | Low | Contact GP within days; consider antihistamines |
| Swelling of lips/face | High | Seek urgent medical attention |
| Blistering/peeling | High | Contact GP immediately or go to hospital |
| Rash and difficulty breathing | Very High | Call emergency services |
This table’s not meant to cause anxiety, but to give you a quick read on what’s minor and what definitely needs a professional’s eye.
Staying Safe: Long-Term Tips When Taking Blood Pressure Meds
By now, you might be feeling a bit wary about your daily dose. The truth is, thousands rely on losartan safely every day. Should you panic about rashes? Not at all—most people never get them. But staying alert to the possibility means you catch problems early and fix them fast.
Routine is your best friend here. Before you pop any pills, scan your skin briefly in the shower or before bed—just a few seconds every couple of days. If you see something different, it’s worth a quick photo on your phone (just for your eyes or to show your doctor). If you have a history of allergies or sensitive skin, let your pharmacist know before you start a new prescription—they can flag possible overlapping risks and give you a heads-up on what to watch.
When starting or changing blood pressure meds, jot down the start date and note any new symptoms, even if they seem minor. Sometimes, the symptoms are subtle at first—maybe a faint bump, mild itch, or your skin is just a bit more reactive to sun or soaps. People with darker skin tones should especially note changes in evenness of pigment, as rashes may appear more subtle or gray rather than red.
- Never mix medications without checking for cross-reactions, especially supplements and herbal products.
- Avoid using strong soaps, hot showers, and rough scrubs during your first month on a new blood pressure drug—it keeps your skin less reactive.
- If you do get a rash, don’t hide it or feel embarrassed—doctors deal with this every week, and you won’t be the first patient to come in with a photo on your phone.
The risk of severe skin reactions is tiny, but if you notice anything dramatic—like sudden swelling of your face, thick hives, breathing issues—drop everything and get medical help. It’s so much better to be safe (and a bit dramatic) than to regret waiting. For everything else, a check-in with your doctor or pharmacist is the smartest move.
Knowledge is your power. Being aware of what to look for, and knowing when to reach out, means you control your health rather than your meds controlling you. Blood pressure treatment doesn’t have to come with nasty surprises—just a dash of awareness and a cooperative GP can keep your skin and your heart in the clear.
11 Comments
allen doroteo
April 26, 2025 at 00:35 AM
Honestly, this whole "losartan rash" hype feels blown out of proportion!!! i think most people just blame the med for anything that pops up on their skin, even if it’s just a bug bite or dry skin. People love to point fingers at drugs without checking the basics. It’s like, "oh my new pill, my rash!" no wonder doctors are swamped!!! take a look at your laundry detergent first, lol.
Corey Jost
April 26, 2025 at 01:00 AM
When you examine the epidemiological data, you see that the incidence of dermatologic adverse events among losartan users hovers around one percent, which translates to a relatively low absolute risk when contextualized against the millions of prescriptions written each year. That figure, however, can be misinterpreted if you fail to account for confounding variables such as concurrent allergies, seasonal changes, and the prevalence of comorbid skin conditions in the hypertensive population. Moreover, the latency period for immunologically mediated reactions can span weeks to months, making causality attribution a nuanced endeavor that requires more than just a temporal association. Clinicians often employ rechallenge protocols or dermatologic patch testing to clarify the offending agent, and these methods are rarely discussed in lay summaries. It is also worth noting that alternative antihypertensive classes are not free from cutaneous side effects; ACE inhibitors, for example, have their own documented rash profiles. Therefore, while vigilance is prudent, the narrative that losartan is a rash‑inducing villain is an oversimplification that overlooks the broader pharmacovigilance landscape. In practice, a balanced risk‑benefit analysis, informed by patient history and phenotypic presentation, guides therapeutic decisions more effectively than anecdotal alarmism. Ultimately, maintaining open communication with your prescribing physician remains the cornerstone of safe medication management.
Nick Ward
April 26, 2025 at 01:08 AM
That’s a solid overview – I’d add that keeping a symptom diary can really help the doctor see patterns. 😊 Also, a gentle reminder to never stop losartan abruptly; tapering under supervision is key.
felix rochas
April 26, 2025 at 01:33 AM
Wake up!!! The pharma giants don’t want you to know that losartan is part of a massive skin‑reaction cover‑up!!! They push these “safe” labels while secretly monitoring adverse events and burying the data! If you’re seeing rashes, it’s not a coincidence – it’s a deliberate suppression of truth!!! Demand transparency!!
inder kahlon
April 26, 2025 at 01:41 AM
While vigilance is important, current clinical guidelines suggest that most losartan‑related rashes are mild and resolve after discontinuation or symptomatic treatment. If you experience severe symptoms, seek immediate medical care.
Dheeraj Mehta
April 26, 2025 at 02:06 AM
Hey there! It’s great you’re paying attention to your skin – a little proactive habit can save a lot of hassle later. If you notice any new spots, snap a quick photo, jot down the date, and let your doctor know. A simple check‑in can keep things smooth.
Oliver Behr
April 26, 2025 at 02:15 AM
Spot on! Keeping a visual log is a practical tip that works across cultures – a picture is worth a thousand words, especially for dermatologists.
Tiffany W
April 26, 2025 at 02:40 AM
From a pharmacovigilance standpoint, the incidence of cutaneous adverse drug reactions (cADRs) associated with ARBs, including losartan, is substantiated by post‑marketing surveillance data, which underscores the necessity of rigorous risk‑assessment frameworks and informed consent protocols in clinical practice.
Rajeshwar N.
April 26, 2025 at 02:48 AM
True, the data exists, but let’s not forget that absolute risk remains low. Over‑emphasizing rare side effects can inadvertently cause patients to abandon effective therapy.
Louis Antonio
April 26, 2025 at 02:56 AM
Sounds like a placebo effect.


Uju Okonkwo
April 26, 2025 at 00:26 AM
If you’ve just started noticing a patch of red on your arm or chest, the first thing to do is pause and take a quick inventory of any recent changes in your medication regimen. The timing is often the most telling clue, because drug‑induced rashes typically surface within a few days to a month after the new prescription is filled. Compare the start date of losartan with the onset of the skin irritation; if they line up, you have a solid lead. Next, document the rash with a clear photo – a smartphone camera works fine – and note whether it’s itchy, painful, or spreading to new areas. Keep track of any accompanying symptoms like swelling around the lips, shortness of breath, or fever, because those could signal a more severe reaction. Bring this information to your next GP visit; a concise report saves the doctor time and speeds up the decision‑making process. Your doctor may recommend a short trial of antihistamines or a low‑potency steroid cream to see if the rash eases, which can help differentiate an allergic reaction from a simple irritation. If the rash improves after a few days, you might be looking at a mild, self‑limiting response, but if it persists or worsens, the clinician will likely suggest pausing losartan under medical supervision. Switching to an alternative antihypertensive, such as a calcium channel blocker, is a common strategy and typically does not jeopardize blood pressure control. Throughout this process, stay hydrated, avoid harsh soaps and hot showers, and wear loose, breathable fabrics to reduce further skin stress. Remember that even though severe reactions like Stevens‑Johnson syndrome are rare, early detection and intervention are key to preventing escalation. Finally, keep an eye on any future medication changes – a rash can sometimes reappear with a different drug if you have a predisposition, so maintaining a personal side‑effect log is a smart habit. By staying proactive and communicative with your healthcare team, you can protect both your skin and your cardiovascular health.