Autoimmune diseases like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis don’t just cause joint pain-they slowly eat away at your body’s ability to move, work, and live normally. The immune system, meant to protect you, turns against your own tissues. That’s where DMARDs and biologic medications come in. These aren’t painkillers. They don’t just mask symptoms. They change the course of the disease. And understanding how they work can make all the difference in your treatment journey.
What Are DMARDs, Really?
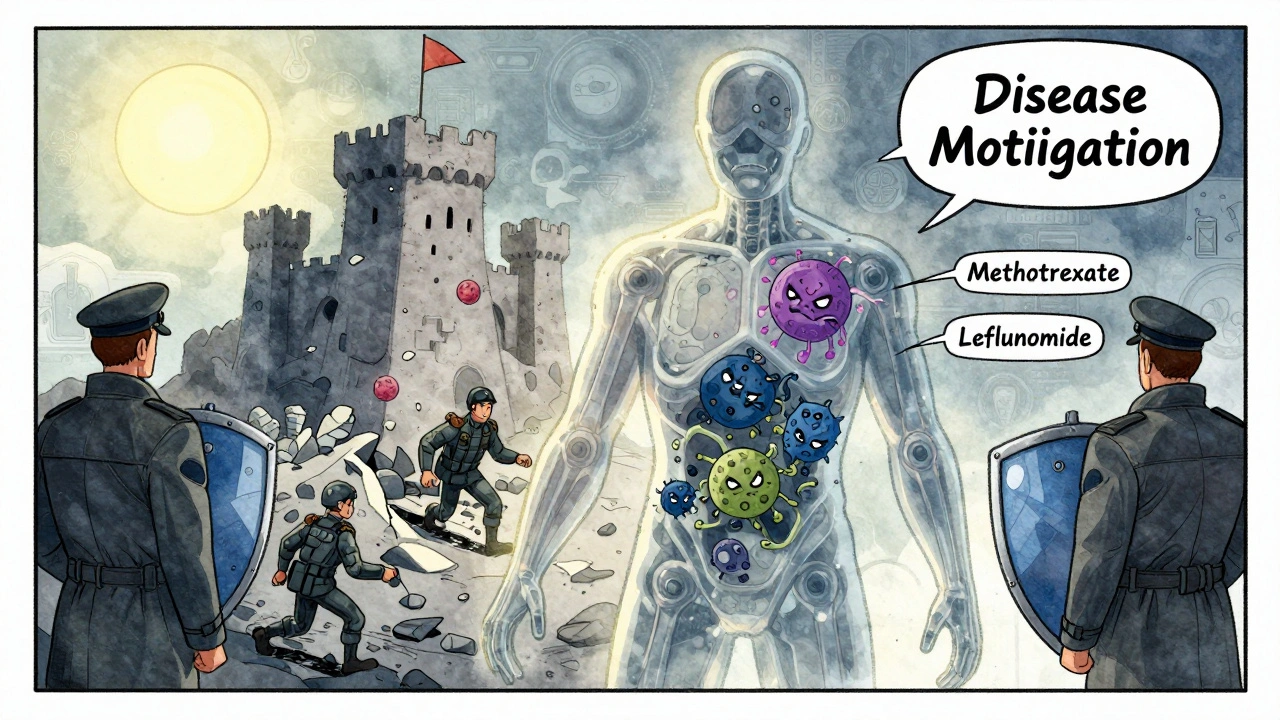
DMARD stands for disease-modifying antirheumatic drug. The word “disease-modifying” is key. Unlike ibuprofen or cortisone shots that calm inflammation temporarily, DMARDs go after the root problem: your overactive immune system. They slow or stop the damage before it becomes permanent. Think of them as peacekeepers inside your body, stopping the immune system from attacking your joints, skin, or organs.
There are three main types. The first are conventional synthetic DMARDs-the original, older drugs. These include methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine. Most are taken as pills once a day or once a week. Methotrexate, for example, is the most commonly prescribed. It’s been used since the 1980s and is still the first-line treatment for rheumatoid arthritis because it works, and it’s affordable-often under $30 a month without insurance.
But these drugs aren’t precise. They dampen the whole immune system. That’s why side effects like nausea, fatigue, liver stress, and low blood counts happen. That’s also why you need regular blood tests every 4 to 8 weeks, especially when starting out. Your doctor isn’t being overly cautious-they’re watching for hidden problems before they become serious.
Biologic Medications: The Next Generation
Biologics came on the scene in the early 1990s and changed everything. These aren’t made from chemicals in a lab. They’re made from living cells-proteins designed to target one specific part of the immune system. Instead of shooting in the dark, they’re like sniper rifles. One drug blocks TNF-alpha, another stops IL-6, another wipes out B-cells. Each targets a different pathway that’s driving inflammation.
Common biologics include adalimumab (Humira), etanercept (Enbrel), infliximab (Remicade), rituximab (Rituxan), and tocilizumab (Actemra). Most are given as injections you can do at home or as IV infusions at a clinic. You’ll need training to give yourself the shot. Many patients say the first few injections feel intimidating, but after a couple of tries, it becomes routine-like brushing your teeth.
Biologics often work faster than conventional DMARDs. While methotrexate might take 3 to 6 months to show real results, some biologics start helping in just a few weeks. For people who haven’t responded to methotrexate alone, biologics can mean the difference between staying in a wheelchair and walking again. One study showed a 70% improvement in joint pain scores after 6 months on a biologic.
Why Do Doctors Start with Conventional DMARDs First?
You might wonder: if biologics are so powerful, why not start with them? The answer is simple: cost, safety, and evidence.
Biologics are expensive. Without insurance, they can cost $1,000 to $5,000 a month. Even with insurance, co-pays can hit $500 or more. Methotrexate? A few dollars. Insurance companies know this. They almost always require you to try a conventional DMARD first before approving a biologic. This isn’t bureaucracy-it’s based on decades of data showing that for many people, methotrexate alone is enough.
Also, biologics carry higher risks. Because they’re so targeted and potent, they leave you more vulnerable to serious infections. Tuberculosis, pneumonia, even fungal infections can become dangerous. That’s why you get screened for TB before starting any biologic. You also need to avoid live vaccines while on them. If you get a fever, sore throat, or unexplained cough, you call your doctor immediately-not wait it out.
And here’s something many don’t realize: your body can build antibodies against some biologics. Over time, they stop working. That’s called loss of response. When that happens, your doctor might switch you to a different biologic or add another drug. It’s not failure-it’s part of the process.
Targeted Synthetic DMARDs: The Oral Alternative
There’s a newer category that sits between conventional and biologic DMARDs: targeted synthetic DMARDs. These are pills, like tofacitinib (Xeljanz) and upadacitinib (Rinvoq). They’re called JAK inhibitors. They block specific enzymes inside immune cells that trigger inflammation.
They’re faster than methotrexate, easier than injections, and often used when biologics aren’t an option. But they come with their own risks. The FDA added black box warnings for increased risk of blood clots, heart problems, and certain cancers. That’s why they’re usually reserved for people who can’t take biologics or haven’t responded to them.
Still, for many, the convenience of an oral pill outweighs the risks-especially if they hate needles or have trouble getting to infusion centers.
What to Expect When You Start Treatment
Starting DMARD therapy isn’t a quick fix. It’s a marathon. You won’t feel better overnight. With methotrexate, it can take 8 to 12 weeks before you notice less stiffness or swelling. Biologics might show results sooner, but you still need patience.
Side effects are common early on. Nausea from methotrexate? Take it with food or at night. Mouth sores? Folic acid supplements help. Injection site redness or itching? Apply ice and rotate spots. These aren’t reasons to quit-they’re signs your body is adjusting.
Regular blood work is non-negotiable. You’ll need liver and kidney tests, complete blood counts, and sometimes lung function checks. Skipping tests isn’t worth the risk. Many patients stop because they feel fine. But damage can be happening silently.
Adherence is a huge issue. Studies show 30% to 50% of patients miss doses at some point. Life gets busy. You forget. You feel better and think you don’t need it anymore. But stopping DMARDs-even for a few days-can trigger a flare that takes weeks to control again. Set phone alarms. Use pill organizers. Keep a log. Your future self will thank you.

Cost, Access, and the Reality of Insurance
The biggest barrier for many isn’t the medicine-it’s getting it. Biologics require prior authorization. That means your doctor submits paperwork, your insurance reviews it, and you wait. It can take 2 to 6 weeks. During that time, your joints keep getting damaged.
Biosimilars are helping. These are near-identical copies of brand-name biologics. Humira has several biosimilars now, cutting the price by 15% to 30%. That’s a big deal. But not all insurers cover them automatically. You might still need to fight for coverage.
Some drug companies offer patient assistance programs. If you’re struggling to pay, ask your rheumatologist’s office. They often have specialists who help navigate financial aid, co-pay cards, and free drug programs.
Long-Term Outlook: Is This Treatment Forever?
For most people with autoimmune diseases, DMARDs aren’t a short-term fix. They’re a long-term commitment. The goal isn’t to cure the disease-it’s to keep it quiet. Many patients stay on methotrexate or a biologic for years, even decades.
But some do achieve remission. That means no signs of active disease for six months or longer. In those cases, doctors may slowly reduce the dose-not stop it entirely. Stopping too soon can bring the disease roaring back.
Research is moving fast. New drugs targeting different immune pathways are in clinical trials. The hope is for treatments that work just as well but with fewer side effects. The American College of Rheumatology predicts biologic use will grow 5% to 7% each year through 2030. But access remains unequal. In developing countries, many still can’t get these medicines at all.
What You Can Do Today
If you’re on DMARD therapy:
- Take your meds exactly as prescribed-even on days you feel fine.
- Track your symptoms and side effects in a notebook or app.
- Get your blood work done on time.
- Report any fever, chills, or unusual fatigue immediately.
- Ask about biosimilars if cost is a problem.
- Don’t skip vaccinations (but avoid live ones like the nasal flu spray).
If you’re not on treatment yet but have symptoms:
- See a rheumatologist-not just your primary doctor.
- Don’t wait for X-rays to show damage. Early treatment changes outcomes.
- Ask about methotrexate first. It’s the gold standard for a reason.
DMARDs and biologics aren’t perfect. But they’ve turned what used to be a life-limiting disease into a manageable condition for millions. The key isn’t finding the perfect drug-it’s finding the right one for you, sticking with it, and staying in close contact with your care team.
How long does it take for DMARDs to start working?
Conventional DMARDs like methotrexate usually take 6 to 12 weeks to show noticeable improvement. Biologics can start working in as little as 2 to 4 weeks, but full benefits often take 3 months. Patience is critical-these drugs work by changing the immune system’s behavior, not by masking pain.
Can I stop taking DMARDs if I feel better?
No-not without talking to your doctor. Feeling better means the medication is working. Stopping it suddenly can cause a flare-up, sometimes worse than before. Some patients in remission may reduce their dose slowly under medical supervision, but most need to stay on some form of treatment long-term to keep the disease controlled.
Are biologics safe during pregnancy?
Some biologics, like adalimumab and etanercept, are considered low-risk during pregnancy and may be continued under doctor supervision. Others, like rituximab, are not recommended. Methotrexate is dangerous during pregnancy and must be stopped at least 3 months before trying to conceive. Always discuss pregnancy plans with your rheumatologist before making any changes.
What are the biggest risks of biologic medications?
The biggest risks are serious infections (like tuberculosis, pneumonia, or sepsis), reactivation of latent viruses like hepatitis B, and a slightly higher chance of certain cancers, especially lymphoma. That’s why screening and monitoring are required. The risk is low for most people, but it’s real-so never ignore signs like fever, night sweats, or unexplained weight loss.
Why do I need blood tests every few weeks?
Conventional DMARDs like methotrexate can affect your liver, kidneys, and bone marrow. Blood tests check for early signs of damage-like rising liver enzymes or dropping white blood cells-before you feel symptoms. Biologics need less frequent testing, but your doctor still needs to monitor for infection markers and overall health. Skipping tests can lead to serious, avoidable complications.
Can I take herbal supplements with DMARDs?
Many herbal supplements can interfere with DMARDs. Turmeric, ginger, and echinacea may increase immune suppression or liver stress. St. John’s wort can reduce the effectiveness of some drugs. Always tell your rheumatologist about every supplement you take-even if you think it’s “natural” and harmless. What seems safe might be dangerous when combined with your treatment.
If you’re managing an autoimmune disease, you’re not alone. Millions are on DMARDs and biologics, and many are living full, active lives because of them. The road isn’t easy, but with the right information and support, you can take control-not just of your symptoms, but of your future.
8 Comments
Irving Steinberg
December 2, 2025 at 15:27 PM
People act like biologics are magic bullets but honestly most of them just make you a walking infection waiting to happen 😅
Kay Lam
December 3, 2025 at 03:26 AM
I’ve been on biologics for seven years now and I still remember the first time I walked into a grocery store without needing a cane it wasn’t just physical it was emotional like my body finally stopped betraying me and yes I know the risks but the alternative was worse and if you’re scared of needles just remember the first shot feels like a needle prick and then you do it again and again and it becomes part of your routine like brushing your teeth or checking your phone and honestly if you’re reading this and you’re hesitant you’re not alone but you’re also not broken you’re just fighting something invisible and that’s okay
Courtney Co
December 3, 2025 at 19:57 PM
I know you think you’re helping but have you ever thought about how your insurance denies you because you didn’t try methotrexate first and then you wait six weeks and your joints turn to cement and your husband leaves because he can’t handle watching you cry every morning and you’re just trying to live but the system is designed to break you and I’m not mad I’m just tired
Shashank Vira
December 4, 2025 at 04:11 AM
The notion that DMARDs are merely pharmacological tools is a gross oversimplification. One must consider the ontological shift in patient identity that occurs when one internalizes chronic illness as a permanent condition. The pharmaceutical industry, in its capitalist hegemony, commodifies suffering through exorbitant pricing structures that render biologics inaccessible to the global majority. One cannot speak of treatment without speaking of justice.
Jaswinder Singh
December 4, 2025 at 12:37 PM
You think you're tough because you take your meds? Try doing it when you're working two jobs and your insurance won't cover the blood tests. I've missed three in a row and I'm still here. You think you're helping by saying 'just take it'? You have no idea.
Bee Floyd
December 5, 2025 at 18:08 PM
I used to hate the needle. Now I call it my weekly power-up. It’s not perfect but it’s mine. And yeah, the blood tests are annoying but they’re the price of staying in the game. I’ve got a spreadsheet now. Track my pain, my meds, my sleep. It’s weirdly satisfying. Like being a detective in my own body. And if you’re scared of losing your job because you need an infusion? You’re not alone. I got laid off last year. Took me six months to get back on my feet. But I’m still here. Still moving. Still fighting. That’s the win.
Jeremy Butler
December 6, 2025 at 19:04 PM
The epistemological framework underpinning the administration of disease-modifying antirheumatic agents necessitates a rigorous adherence to clinical protocols predicated upon longitudinal observational data. Deviation from such protocols, irrespective of subjective symptomatology, constitutes a metaphysical rupture in the therapeutic contract between patient and physician, thereby compromising the integrity of the biomedical paradigm.

Lydia Zhang
December 1, 2025 at 13:49 PM
I took methotrexate for a year and it just made me feel like a zombie. No energy, constant nausea. I switched to Humira and life changed. But yeah, the cost is insane.