Hydroxyzine QT Prolongation Risk Calculator
Risk Assessment Tool
This tool helps you understand your personal risk of QT prolongation when taking hydroxyzine based on factors discussed in the article. Please answer all questions honestly for the most accurate assessment.
Hydroxyzine is one of those medications that many doctors still prescribe without thinking twice. It’s cheap, it works for anxiety, itching, and even nausea, and for decades, it was considered safe. But here’s the truth: hydroxyzine can mess with your heart rhythm - and in rare but dangerous cases, it can trigger a life-threatening arrhythmia called Torsade de Pointes. This isn’t just theoretical. It’s happening in real patients, and the data is clear: if you’re over 65, have a history of heart issues, or are taking other medications, hydroxyzine could be riskier than you were told.
How Hydroxyzine Affects Your Heart
Hydroxyzine doesn’t just block histamine receptors. It also blocks something called the hERG potassium channel in your heart. This channel helps your heart reset after each beat. When it’s blocked, your heart takes longer to repolarize - and that shows up on an ECG as a prolonged QT interval. A longer QT interval means your heart is more vulnerable to chaotic electrical signals. That’s when Torsade de Pointes can kick in - a wild, irregular heartbeat that can lead to fainting, seizures, or sudden death.
This isn’t a new discovery. The European Medicines Agency (EMA) confirmed it back in 2015 after reviewing over 50 case reports. Since then, they’ve cut the maximum daily dose from 150 mg to 100 mg for adults, and 50 mg for people over 65. Why? Because the risk isn’t random. It’s dose-dependent. Take more, and your chance of a dangerous rhythm goes up. Take it with other drugs that also prolong QT, and the risk multiplies.
Who’s at Risk? Not Everyone - But Many More Than You Think
Most healthy young adults can take hydroxyzine without issue. But here’s where it gets dangerous: the people who are most likely to get it are also the most likely to be at risk.
- Elderly patients - Their kidneys and liver don’t clear the drug as well. Hydroxyzine builds up. Half-life can stretch from 14 to over 25 hours.
- People with low potassium or magnesium - Electrolyte imbalances are common in diabetics, dialysis patients, or those on diuretics. These make the heart extra sensitive to QT prolongation.
- Those on other QT-prolonging drugs - Think antibiotics like azithromycin, antidepressants like citalopram, or antiarrhythmics like amiodarone. Combine these with hydroxyzine? You’re playing with fire.
- People with undiagnosed long QT syndrome - Some genetic conditions make the heart unusually sensitive. One case report described a 45-year-old man who fainted 15 minutes after taking just 25 mg of hydroxyzine for itching. He had never been tested for long QT.
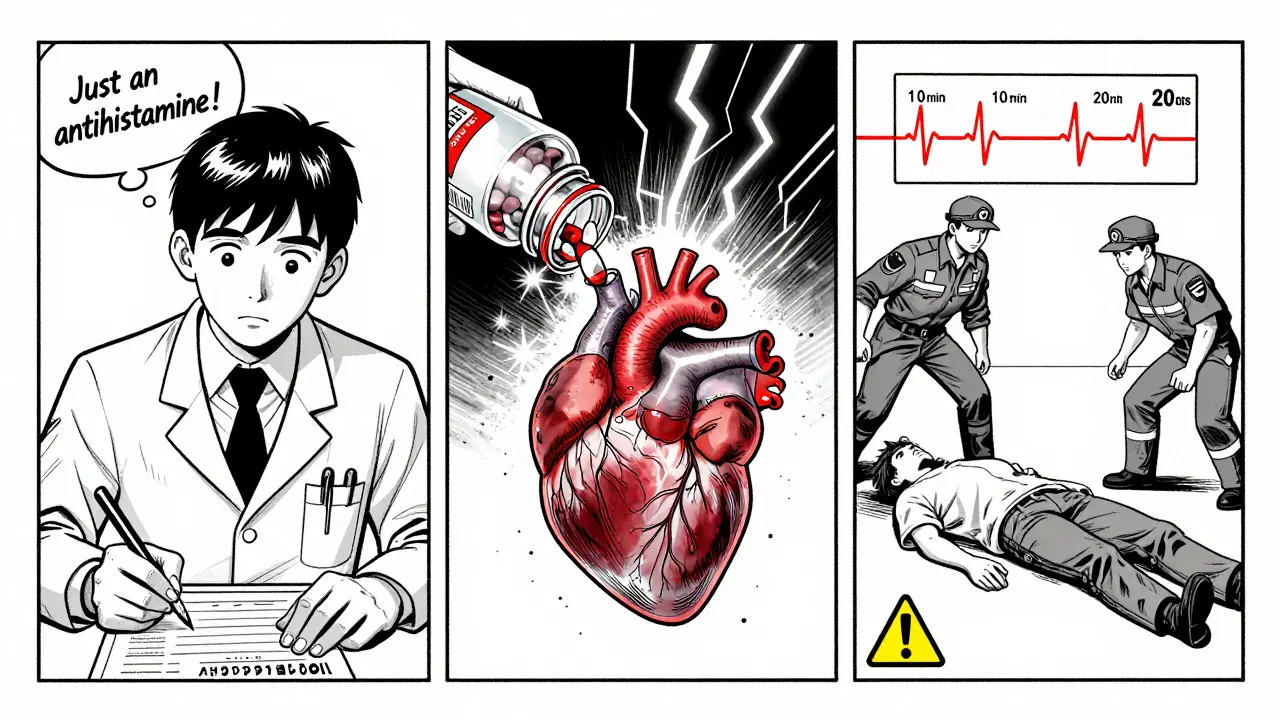
A 2021 survey of 127 hospital pharmacists found that 63% had seen hydroxyzine prescribed to patients with two or more risk factors - even though guidelines say to avoid it in that group. That’s not negligence. That’s ignorance. Many prescribers still think antihistamines are “safe.” They’re not.
How Hydroxyzine Compares to Other Antihistamines
Not all antihistamines are created equal when it comes to heart risk.
| Drug | Generation | QT Prolongation Risk | hERG Blockade | Common Use |
|---|---|---|---|---|
| Hydroxyzine | First | Known Risk (CredibleMeds) | High | Anxiety, pruritus, sedation |
| Diphenhydramine | First | Possible Risk | Moderate | Allergies, insomnia |
| Cetirizine | Second | Minimal Risk | Very Low | Allergies |
| Loratadine | Second | Minimal Risk | Negligible | Allergies |
| Fexofenadine | Second | No Risk | None | Allergies |
Second-generation antihistamines like cetirizine and loratadine are almost completely safe for the heart. They don’t cross the blood-brain barrier well, so they’re less sedating - and they don’t touch the hERG channel. If you’re taking hydroxyzine for allergies or itching, there’s almost never a reason not to switch.
Even among first-generation drugs, hydroxyzine is riskier than diphenhydramine. Why? Its chemical structure lets it bind more tightly to the hERG channel. A 2020 study from UC Davis showed hydroxyzine blocks potassium flow at concentrations you actually reach with normal doses. Diphenhydramine? It needs higher doses to do the same.

What Should You Do If You’re Taking Hydroxyzine?
If you’re on hydroxyzine, here’s what to do right now:
- Check your dose. Are you taking more than 50 mg a day if you’re over 65? More than 100 mg if you’re under 65? Stop. Talk to your doctor.
- Review all your meds. Use the CredibleMeds website (or ask your pharmacist) to see if anything you’re taking also prolongs QT. Combine even one other drug with hydroxyzine? Risk jumps.
- Get an ECG. If you’ve been on hydroxyzine for more than a few weeks, ask for a 12-lead ECG. QTc should be under 450 ms for men, 470 ms for women. Anything above 500 ms? Hydroxyzine is a hard no.
- Watch for symptoms. Dizziness, palpitations, fainting - especially within an hour of taking it? That’s not just anxiety. That’s your heart warning you.
One 68-year-old woman in a 2022 case report had no heart history. She took 50 mg of hydroxyzine for anxiety. Six hours later, she went into Torsade de Pointes. She needed emergency cardioversion. She was on amiodarone - a known risk. But her doctor didn’t check her meds. She got lucky. Others don’t.
The Bigger Picture: Why This Still Happens
Hydroxyzine prescriptions dropped from 18.3 million in 2014 to 12.7 million in 2022 in the U.S. That’s progress. But it’s still the go-to drug for anxiety in elderly patients - especially in nursing homes and outpatient clinics. Why? Because it’s cheap. Because it’s familiar. Because no one told the prescribers.
The American Geriatrics Society Beers Criteria now lists hydroxyzine as “potentially inappropriate” for older adults. The FDA added it to its official QT prolongation list in 2019. But many doctors still don’t know. Or they think, “It’s just an antihistamine.”
Here’s the hard truth: we treat hydroxyzine like a harmless sedative. But its cardiac risk profile is closer to drugs like citalopram - not Benadryl. And unlike citalopram, there’s no monitoring requirement. No ECG. No dose adjustment. Just a script.
Alternatives That Are Safer
If you need something for anxiety, itching, or sleep - here are better options:
- For anxiety: Buspirone, SSRIs (like sertraline), or low-dose mirtazapine (which doesn’t prolong QT).
- For itching: Cetirizine, fexofenadine, or gabapentin (which has its own risks, but none related to QT).
- For sleep: Melatonin, doxylamine (in low doses), or cognitive behavioral therapy - not hydroxyzine.
A 2022 study found that after the EMA guidelines, gabapentin prescriptions for itching jumped 62%. Mirtazapine use for insomnia in the elderly rose 45%. These aren’t perfect - but they’re safer than hydroxyzine when your heart’s on the line.
What’s Next? The Future of Hydroxyzine
Researchers are already working on a new version - called VH-01 - that keeps the antihistamine effect but cuts hERG binding by 87%. Phase I trials are promising. But that’s years away.
Right now, the 2025 European Society of Cardiology guidelines are expected to ban chronic hydroxyzine use entirely. It will only be allowed as a single dose for procedural anxiety - like before a dental visit.
That’s the future. And it’s coming fast.
Can hydroxyzine cause sudden death?
Yes. Hydroxyzine can trigger Torsade de Pointes, a type of ventricular arrhythmia that can lead to sudden cardiac arrest. While rare, this has been documented in multiple case reports - especially in elderly patients, those with electrolyte imbalances, or those taking other QT-prolonging drugs. The risk is low in healthy people but becomes dangerous with even one additional risk factor.
Is hydroxyzine safe if I have a pacemaker?
Having a pacemaker doesn’t protect you from QT prolongation. Pacemakers manage slow heart rates but don’t prevent dangerous fast rhythms like Torsade de Pointes. If you have a pacemaker and are on hydroxyzine, you’re still at risk - especially if you have other risk factors like low potassium or are taking other QT-prolonging drugs. Always get an ECG before starting hydroxyzine, even with a pacemaker.
How long does it take for hydroxyzine to affect the QT interval?
QT prolongation can occur as soon as 10 minutes after taking hydroxyzine, but it can also take up to 20 days. The risk builds with repeated doses because the drug accumulates in the body. That’s why some patients seem fine at first - then suddenly collapse days later. Don’t assume safety just because you’ve taken it before.
Can I take hydroxyzine if I’m on a beta-blocker?
Beta-blockers can help stabilize heart rhythm and are sometimes used to treat long QT syndrome. But they don’t cancel out hydroxyzine’s effect on the hERG channel. If you’re on a beta-blocker and hydroxyzine, you’re still at risk - especially if you have other factors like low magnesium or are elderly. Always get an ECG before combining them.
Should I stop hydroxyzine if I feel dizzy after taking it?
Yes. Dizziness, lightheadedness, or palpitations within an hour of taking hydroxyzine could be your body’s warning sign. These aren’t just side effects - they can be early signs of QT prolongation. Stop the medication and contact your doctor immediately. Don’t wait for a fainting spell. That’s too late.
Final Thought
Hydroxyzine isn’t evil. It’s useful. But it’s not harmless. We’ve spent decades treating it like a sleepy-time pill. Now we know better. It’s a drug that needs an ECG, a risk assessment, and a second thought - not just a prescription pad. If you’re taking it, ask: Do I really need it? Is there a safer option? And most importantly - has anyone checked my heart?
15 Comments
Angie Datuin
February 11, 2026 at 18:28 PM
My grandma was prescribed this for 'sleep issues' last year. She fainted once. We thought it was just old age. This makes so much sense now.
Kathryn Lenn
February 13, 2026 at 02:06 AM
So let me get this straight - the same drug that's been in every nursing home since the '80s is now a 'cardiac time bomb' because some pharma watchdogs got bored? Classic. Next they'll ban aspirin because it 'might' thin your blood too much. Wake up, sheeple.
Joseph Charles Colin
February 14, 2026 at 15:51 PM
hERG blockade is dose-dependent and cumulative. The real issue is polypharmacy in elderly populations. Hydroxyzine’s half-life extends to >25h in renal impairment. When combined with amiodarone or citalopram, the QTc can spike >500ms within 72h. ECG monitoring isn't optional - it's mandatory. Also, fexofenadine is the gold standard for non-sedating antihistamine replacement. No hERG binding, renal excretion only. Simple swap.
Frank Baumann
February 16, 2026 at 01:50 AM
I work in a rural clinic. We prescribe hydroxyzine because it's $3, it works, and the patients don't complain. We don't have ECG machines. We don't have pharmacists on staff. We don't even have time to check for drug interactions. So yeah - you're right. But what are we supposed to do? Tell a 72-year-old with chronic itching to 'just take cetirizine' when she can't afford it? This isn't a medical ethics debate - it's a healthcare access crisis.
Ritteka Goyal
February 16, 2026 at 15:48 PM
I live in India and we use hydroxyzine ALL THE TIME. No ECG, no labs, no problem. Why should Americans overthink everything? In my village, grandmas take it for anxiety and sleep and live to 90. Maybe your system is broken, not the drug. Also, why are you so scared of a simple antihistamine? We don't have this drama here.
Andrew Jackson
February 17, 2026 at 12:46 PM
This is what happens when we abandon common sense for regulatory dogma. Hydroxyzine has been used safely for 70 years. Now, because a few rare cases were documented, we're going to ban it for millions? What's next? Banning ibuprofen because it might cause GI bleeds? This isn't science - it's fearmongering dressed up as public health.
Scott Conner
February 17, 2026 at 15:05 PM
wait so hydroxyzine is like a quiet killer? i took it for like 2 years for allergies and never knew. i thought it was just making me sleepy. also i was on zoloft. did i almost die? lol
John Sonnenberg
February 18, 2026 at 15:08 PM
I took hydroxyzine for anxiety after my divorce. Six months later, I had a near-fainting episode during yoga. My cardiologist said, 'You're lucky you didn't die.' I didn't know my meds were playing musical chairs with my heart. This post? It's a wake-up call. I'm telling everyone I know.
PAUL MCQUEEN
February 19, 2026 at 11:38 AM
I'm not saying the risk isn't real, but you're overreacting. Most people who take hydroxyzine don't have underlying conditions. You're scaring people into switching to SSRIs - which have their own hellish side effects. Maybe the solution isn't banning hydroxyzine - it's better education. Not every patient needs an ECG before a $3 script.
Monica Warnick
February 21, 2026 at 11:33 AM
I read this whole thing. I'm not even sure what to think anymore. I've been on it for 4 years. I don't have heart problems. I'm not on anything else. But now I'm scared. I think I'll call my doctor tomorrow.
Ashlyn Ellison
February 21, 2026 at 18:44 PM
I used to take it for sleep. Stopped after a weird dizzy spell. Didn't connect the dots until now. Thanks.
Jonah Mann
February 22, 2026 at 01:01 AM
sooo… if i’m on metoprolol and take hydroxyzine for allergies, am i safe? i mean, beta blockers should help right? or is that a myth? also, can u recommend a good free ekg app? i saw one on reddit but not sure if legit.
glenn mendoza
February 23, 2026 at 22:09 PM
Thank you for bringing this critical issue to light with such clarity and precision. The convergence of pharmacokinetic data, clinical evidence, and real-world prescribing patterns reveals a systemic gap in patient safety protocols. It is imperative that healthcare providers engage in proactive risk stratification, particularly in geriatric populations, and prioritize evidence-based alternatives over convenience-driven therapeutics. The moral imperative to prevent iatrogenic harm cannot be overstated.
Joshua Smith
February 25, 2026 at 00:40 AM
To Jonah: Beta-blockers help stabilize rhythm but don't block hERG. You're still at risk. No app replaces a real ECG - ask your doc for a 12-lead. And yes, metoprolol + hydroxyzine = still dangerous if you're over 65 or low on Mg/K. I got mine done - QTc was 482. They switched me to buspirone. No more dizziness.


Joshua Smith
February 10, 2026 at 18:08 PM
I never realized hydroxyzine could be this risky. I've been taking 50mg for anxiety for years and never had an ECG. Guess I'm scheduling one this week. Thanks for laying this out so clearly.