Blood Pressure & Decongestant Risk Calculator
Assess Your Risk
This tool evaluates potential interactions between your blood pressure medications and decongestants. Based on the 2024 data showing 1 in 5 emergency visits for uncontrolled high blood pressure in adults over 50 were linked to decongestant misuse.
If you're taking medication for high blood pressure and you're fighting a cold, you might be tempted to reach for a nasal decongestant. After all, it’s just a little spray or pill to clear your nose, right? Nasal decongestants might seem harmless, but for people with hypertension, they can be dangerous - even life-threatening. Many don’t realize that over-the-counter remedies can push blood pressure into dangerous territory, interfere with prescribed medications, or trigger heart rhythm problems. This isn’t a rare issue. In 2024, nearly one in five emergency visits for uncontrolled high blood pressure in adults over 50 were linked to improper use of decongestants.
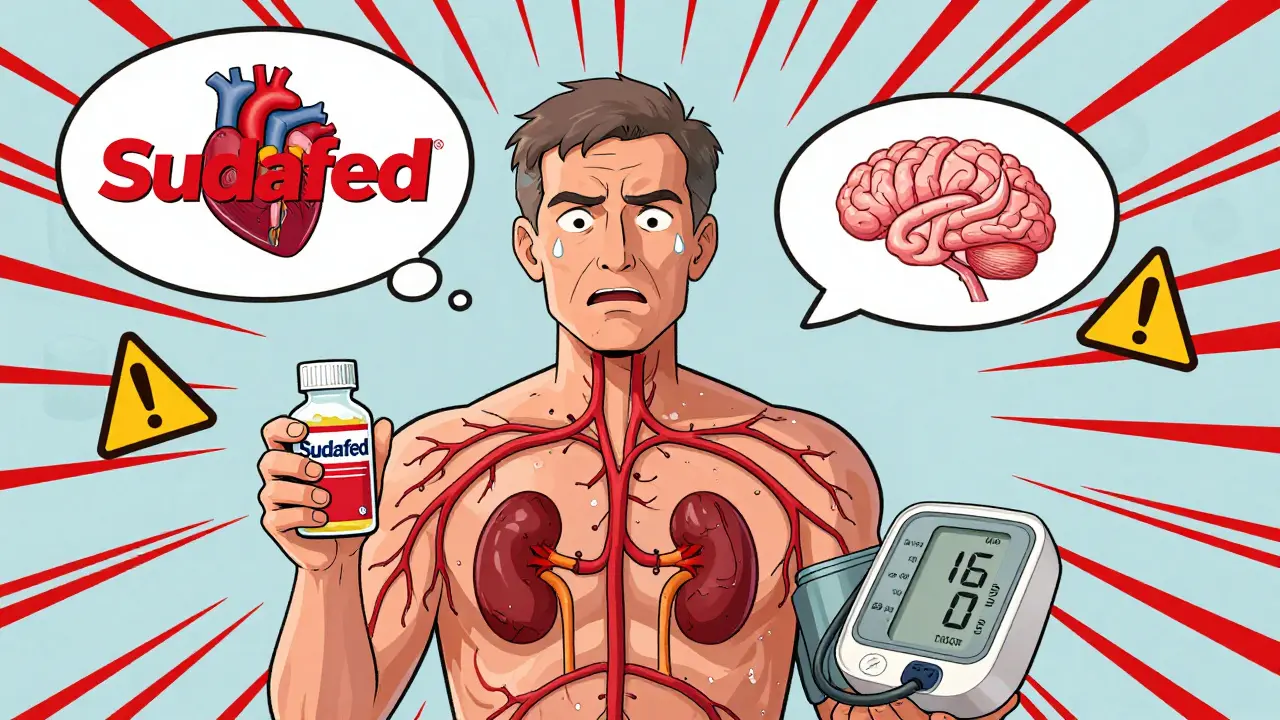
How Nasal Decongestants Raise Blood Pressure
Nasal decongestants like pseudoephedrine (found in Sudafed) and phenylephrine (common in many cold medicines) work by tightening blood vessels in your nose. That reduces swelling and helps you breathe easier. But here’s the catch: they don’t just tighten vessels in your nose. They tighten vessels everywhere - including those in your heart, brain, and kidneys. This forces your heart to pump harder and faster, which raises your blood pressure.
Even a small rise in blood pressure can be risky if you’re already on medication to keep it under control. A 2005 study in the Journal of Clinical Hypertension found that pseudoephedrine caused a measurable increase in systolic blood pressure - the top number - in most people. The effect was stronger with higher doses and immediate-release forms. For someone with uncontrolled hypertension, that spike could mean a stroke, heart attack, or irregular heartbeat.
Topical decongestants like oxymetazoline (Afrin) aren’t any safer. Many assume that since they’re sprayed into the nose, they don’t enter the bloodstream. But studies from the University of Michigan Health System show that even these products can be absorbed into the body, especially with frequent or prolonged use. The American Heart Association warns that all forms of decongestants - oral, nasal spray, or even eye drops - carry the same risks for people with high blood pressure.
Which Blood Pressure Medications Are Affected?
Decongestants don’t just raise blood pressure - they can mess with how your blood pressure meds work. For example:
- Beta-blockers like metoprolol or atenolol: Decongestants can block their effect, making them less able to slow your heart rate or lower pressure.
- Calcium channel blockers like amlodipine or nifedipine: These may not be able to relax your arteries properly when decongestants are tightening them.
- ACE inhibitors like lisinopril: Decongestants can reduce their ability to lower pressure by increasing fluid retention and vascular resistance.
- Diuretics: Some decongestants contain hidden sodium, which counteracts the fluid-removing effect of diuretics.
It gets worse. Decongestants can also interact with other common medications, including certain antidepressants (like tricyclics), antibiotics (like linezolid), and migraine drugs (ergot derivatives). These combinations can cause sudden, extreme spikes in blood pressure - sometimes to levels above 200/120 mmHg. That’s a medical emergency.
What the Experts Say
Major medical organizations are united on this: avoid decongestants if you have high blood pressure.
The American Heart Association says people with hypertension should use decongestants only under a doctor’s supervision. The Mayo Clinic, Cleveland Clinic, and Houston Methodist Hospital all say the same thing: if your blood pressure isn’t fully controlled, skip decongestants entirely. Even if your pressure is usually stable, a decongestant can still push it too high.
Dr. Salman Al-Kindi, a cardiologist at Houston Methodist Hospital, puts it plainly: “There are many types of blood pressure medications, and some people take more than one. It’s not something you can figure out on your own.”
And it’s not just about the decongestant itself. Many cold and flu remedies combine decongestants with pain relievers, antihistamines, or cough suppressants. You might think you’re just taking a “cold tablet,” but if it contains pseudoephedrine or phenylephrine, you’re at risk. A 2024 survey by the Cleveland Clinic found that only 38% of hypertension patients knew decongestants could raise their blood pressure.
What to Look For on the Label
You can’t rely on marketing names like “Sinus Relief” or “Daytime Cold Formula.” You have to read the active ingredients list. Here are the ones to avoid:
- Pseudoephedrine
- Phenylephrine
- Ephedrine
- Oxymetazoline
- Phenylpropanolamine (banned in the U.S., but still found in some imported products)
Also watch out for sodium content. Some liquid cold medicines contain as much as 200-300 mg of sodium per dose - enough to worsen fluid retention and counteract your blood pressure meds. The American Heart Association specifically warns against “medications high in sodium.”
And remember: pseudoephedrine is sold behind the pharmacy counter in the U.S. for a reason. The pharmacist is supposed to ask you if you have high blood pressure. Don’t skip that conversation. Use it as a chance to say, “I’m on blood pressure medication - is this safe?”
Safe Alternatives for Congestion Relief
You don’t have to suffer through congestion. There are safer ways to breathe easier:
- Nasal saline spray or neti pot: Flushes out mucus and irritants without affecting blood pressure. Use plain saline - no additives.
- Humidifiers or steam: A hot shower or bowl of hot water with a towel over your head can loosen congestion naturally.
- Antihistamines like loratadine (Claritin) or cetirizine (Zyrtec): These help if your congestion is due to allergies, not a cold. They don’t raise blood pressure.
- Hydration and rest: Drinking water and sleeping more helps your body fight off the cold faster.
- Elevating your head: Sleep with an extra pillow to reduce nighttime congestion.
These alternatives may take longer to work, but they won’t put your heart at risk. As Dr. Al-Kindi says, “Home remedies are usually enough for mild colds that will pass on their own.”

What to Do If You’ve Already Taken a Decongestant
If you’ve taken a decongestant and you’re on blood pressure medication, monitor yourself closely. Watch for:
- Headache
- Chest pain or tightness
- Fast or irregular heartbeat
- Dizziness or blurred vision
- Severe anxiety or restlessness
If you notice any of these, stop the decongestant immediately. Check your blood pressure if you have a home monitor. If your systolic pressure (top number) rises above 160 mmHg or you feel unwell, call your doctor or go to urgent care. Don’t wait.
Even if you feel fine, talk to your pharmacist or provider. They can help you adjust your cold treatment plan and avoid future risks.
How to Stay Safe Long-Term
Prevention is key. Here’s how to protect yourself:
- Keep a full list of all your medications - prescriptions, OTC, vitamins, supplements - and bring it to every doctor’s visit.
- Always ask your pharmacist: “Is this safe for someone with high blood pressure?”
- Choose single-symptom products. If you only have a stuffy nose, don’t take a “total cold relief” pill that includes cough suppressants or painkillers you don’t need.
- Set a 3-day limit. If congestion lasts longer than 3 days, see a doctor. It might be something else - like sinusitis - that needs different treatment.
- Use apps or pill organizers that flag interactions. Some pharmacy apps will warn you if a new OTC drug conflicts with your blood pressure meds.
Studies show that pharmacist-led counseling reduces inappropriate decongestant use by nearly half. That means your pharmacist is one of your best defenses - use them.
What’s Changing in 2026?
Health experts are taking this issue more seriously. The American College of Cardiology is updating its 2026 hypertension guidelines to include specific warnings about OTC medications. Pharmaceutical companies are testing new non-vasoconstrictive decongestants in Phase 2 trials - drugs that relieve congestion without tightening blood vessels. These could be game-changers.
For now, though, the message is clear: if you have high blood pressure, treat congestion like a landmine. Don’t reach for the first OTC product you see. Ask. Read. Wait. Choose safer options. Your heart will thank you.
14 Comments
Neha Motiwala
February 15, 2026 at 10:52 AM
you think this is bad? wait till you find out how Big Pharma is secretly using decongestants to make people dependent on blood pressure meds. they know people will panic when their BP spikes, so they keep selling the pills. it’s a cycle. i read this on a forum in Kerala. they’ve been doing it since 2018. the FDA? silent. the WHO? quiet. someone needs to blow this wide open.
athmaja biju
February 15, 2026 at 23:44 PM
As an Indian man who has been managing hypertension for over a decade, I must say this article is long but correct. In India, we have a culture of self-medication. We buy cold tablets at the corner shop without asking. And yes, many of them contain pseudoephedrine. I’ve seen friends collapse after taking 'cold cures' from local pharmacies. This is not a Western problem-it’s a global one. We need public awareness campaigns in regional languages. Not just English. Not just in hospitals. On TV. On WhatsApp. On roadside billboards.
Gloria Ricky
February 17, 2026 at 22:08 PM
thank you for writing this. i’ve been on lisinopril for 7 years and i had no idea that my 'daytime cold relief' had phenylephrine in it. i just thought i was being proactive. now i keep a printed list of banned ingredients taped to my medicine cabinet. also, saline spray changed my life. no more headaches. no more panic. just breathe. you’re not alone.
Stacie Willhite
February 18, 2026 at 00:57 AM
i’ve been there. took a decongestant during a bad cold last winter. felt fine until 3am when my heart started doing the cha-cha. i called 911. turned out i was fine, but the scare stuck. now i use a humidifier, drink hot tea with lemon, and sleep with three pillows. it’s slower, but i’m alive. and that’s what matters.
Annie Joyce
February 18, 2026 at 22:41 PM
here’s the wild part: some of those 'safe' antihistamines? they’re loaded with sugar and sodium too. i used to think Zyrtec was harmless-until i checked the label. 180mg sodium per dose. that’s like chugging a can of soda. your diuretic is fighting a losing battle. always read the tiny print. if it says 'sodium-free' on the front? check the back. it’s usually a lie. also-neti pots? holy god. they’re a game changer. just use distilled water. don’t be lazy. your sinuses will thank you.
Rob Turner
February 19, 2026 at 02:26 AM
it’s funny how we treat our bodies like machines you can just plug and play with. take a pill, fix the problem. no. our biology isn’t a car. it’s a symphony. and decongestants? they’re the guy who shows up with a chainsaw and says 'i’m just here to clear the noise.'
also, i love that you mentioned pharmacists. they’re the unsung heroes. next time you go in, ask them what they’d do if they were in your shoes. they’ll tell you. and they won’t sell you junk.
Luke Trouten
February 19, 2026 at 16:24 PM
the most dangerous assumption in modern medicine is that 'over-the-counter' means 'safe for everyone.' that’s a myth. every medication has a risk profile. even water can kill you in excess. the real issue isn’t the decongestant-it’s the lack of systemic education. we teach kids how to do long division but not how to read a medicine label. we need mandatory OTC literacy in high school health classes. it’s not optional. it’s survival.
Gabriella Adams
February 19, 2026 at 21:52 PM
as someone who works in public health, i can tell you: the 38% stat? it’s probably lower in rural areas. we’ve run campaigns in Ohio and Mississippi-people literally didn’t know 'pseudoephedrine' was in their 'all-in-one' cold tablet. they thought it was just 'vitamin C and herbs.' we printed pocket cards with pictures of the banned ingredients. people loved them. one woman said, 'i didn’t know my cold medicine was trying to kill me.' i cried. we need more of this. not just info. empathy. connection.
Kristin Jarecki
February 20, 2026 at 13:26 PM
the guidelines are clear. the science is solid. yet we still see patients presenting with hypertensive emergencies after taking 'just one pill.' the disconnect isn’t ignorance-it’s normalization. we’ve normalized self-medication. we’ve normalized ignoring labels. we’ve normalized assuming 'it’s just a cold.' until someone dies, we won’t change. and that’s the tragedy.
Jonathan Noe
February 22, 2026 at 07:05 AM
you’re all overthinking this. if you’re on blood pressure meds, don’t take decongestants. period. end of story. the real problem? people don’t want to wait. they want to feel better NOW. so they pop pills. here’s the hack: use a neti pot every night. drink chicken soup. sleep 10 hours. your body knows how to heal. you just have to stop interfering. also, if you’re using Afrin for more than 3 days? you’re not treating congestion-you’re addicted. go to the doc. not the store.
Rachidi Toupé GAGNON
February 23, 2026 at 20:53 PM
just took a saline spray before bed. felt like i was breathing through a mountain pass. 🌄 no meds. no panic. just peace. you don’t need chemistry to heal. sometimes you just need steam and patience. stay chill, stay safe.
Jim Johnson
February 24, 2026 at 06:26 AM
my grandma used to say, 'if it’s not in your kitchen, it’s not medicine.' she’d make ginger tea, put Vicks on her chest, and sleep with a humidifier. she lived to 98. no heart issues. no hospital trips. just good sense. maybe we’ve forgotten the simple stuff. try it. it works. and it doesn’t cost a dime.
Vamsi Krishna
February 25, 2026 at 16:24 PM
you all are being too nice. this isn’t just about decongestants. it’s about how the entire pharmaceutical industry preys on vulnerable people. they market these drugs like candy. they hide the warnings in 6-point font. they pay influencers to say 'this is the best cold remedy ever.' and then they profit when you end up in the ER. this is capitalism. not healthcare. i’ve seen it. in Delhi. in Mumbai. in Chicago. it’s the same script. the only solution? boycott Big Pharma. demand transparency. or die quietly.



steve sunio
February 14, 2026 at 12:22 PM
so like... i just took sudafed yesterday and now my head feels like a balloon that's about to pop? maybe that's why i'm seeing floaty dots? lol. anyway, if you're reading this and you're on blood pressure meds, don't be dumb like me. just say no to decongestants. my heart is still mad at me.