
Protease Inhibitor & St. John's Wort Interaction Checker
Your HIV Treatment
Result Analysis
No significant interaction detected
You're not taking St. John's Wort or using low-hyperforin formulation.
Important: Hyperforin is the key compound in St. John's Wort that causes drug interactions. Most products contain 2-5% hyperforin. Only formulations with ≤1mg total hyperforin per day are potentially safe.
When you’re taking protease inhibitors for HIV, your life depends on those pills working exactly as they should. But what if something you’re taking to feel better-like St. John’s Wort for low mood-is quietly sabotaging your treatment? This isn’t theory. It’s happened. And it’s still happening.
What Happens When St. John’s Wort Meets Protease Inhibitors
St. John’s Wort, a popular herbal supplement for mild depression, doesn’t just sit quietly in your body. Its active ingredient, hyperforin, turns on powerful enzymes in your liver and gut-CYP3A4 and P-glycoprotein-that are supposed to help your body get rid of toxins. But here’s the problem: those same enzymes are also responsible for breaking down protease inhibitors like lopinavir, ritonavir, and others.When hyperforin wakes up these enzymes, they start chewing through your HIV meds faster than they should. Studies show that after taking standard St. John’s Wort (900 mg daily), plasma levels of indinavir dropped by 57% in area under the curve (AUC) and by 81% in peak concentration (Cmax). That’s not a minor dip. That’s enough to push your drug levels below the threshold needed to suppress HIV.
Think of it like this: your protease inhibitor is a lock, and HIV is the key trying to turn it. If you don’t have enough of the lock (the drug) in your system, the key (the virus) slips through. That’s how viral load spikes, resistance builds, and treatment fails-all because of a supplement you thought was harmless.
The Evidence Isn’t Hypothetical-It’s Documented
This isn’t just a theory from a lab. In 2000, a real-world study in HIV-negative volunteers showed that St. John’s Wort crashed indinavir levels. By 2002, Dr. Linda Henderson’s review of clinical cases confirmed this wasn’t an isolated event-it was a pattern. The FDA responded in 2003 by requiring all protease inhibitor labels to carry a black box warning: Do not take with St. John’s Wort.The University of Liverpool’s HIV Drug Interactions Database, updated in October 2025, still lists this combination as “Do Not Coadminister.” Why? Because the data doesn’t lie. When people on lopinavir/ritonavir took St. John’s Wort, their drug levels dropped by up to 57%. That’s enough to cause virologic failure. In some cases, patients developed resistance to the entire protease inhibitor class.
And it’s not just one drug. The interaction hits all major protease inhibitors-atazanavir, darunavir, saquinavir, tipranavir. The Merck Manual confirms: concentrations can fall by 40% to 80%. That’s not a risk you gamble with when your life depends on undetectable viral load.
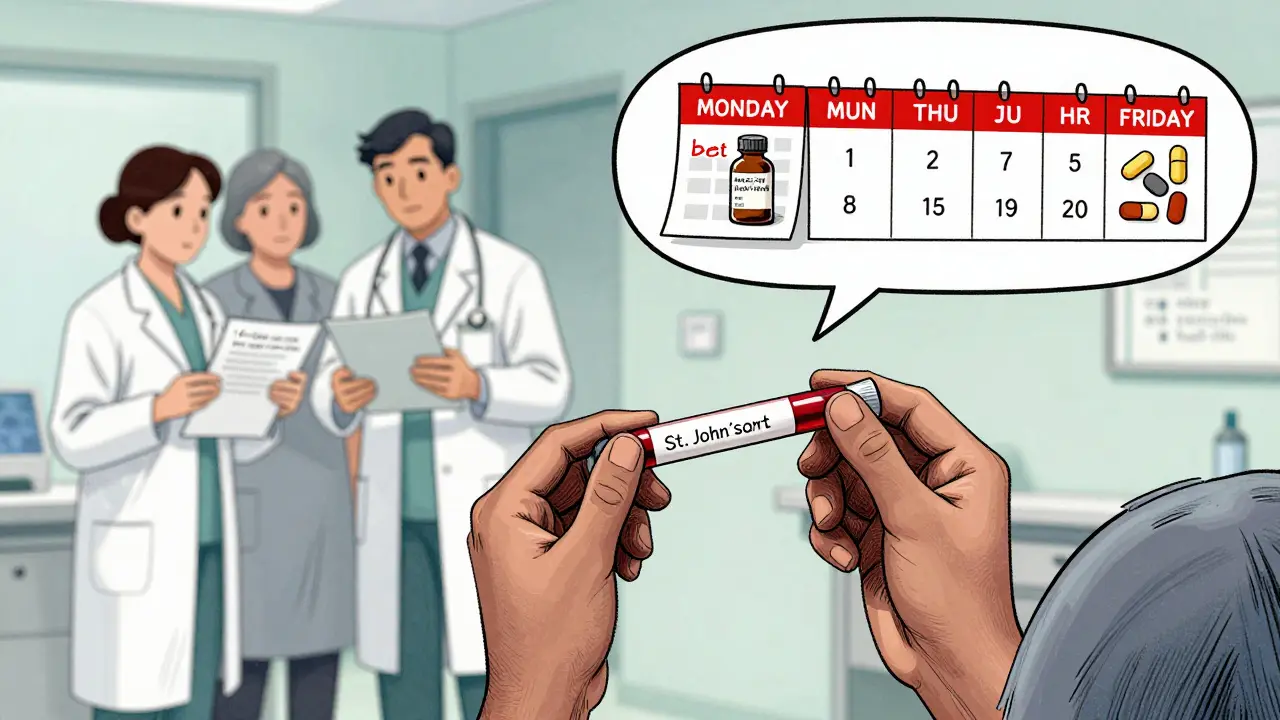
The Hidden Danger: It Doesn’t Stop When You Quit
Here’s what most people don’t realize: the damage doesn’t end when you stop taking St. John’s Wort. The enzymes it induced stay turned on for at least two weeks. That means even if you quit the herb, your HIV meds still won’t work properly for days-or even weeks-afterward.One patient might stop taking St. John’s Wort on Monday, feel better, and assume they’re safe. But by Friday, their viral load could be climbing because their body is still breaking down their HIV drugs too fast. That’s why guidelines say: if you’ve taken St. John’s Wort, monitor your viral load closely for at least 14 days after stopping. And don’t assume your dose is still right-your provider may need to adjust it.

The Nuance: Not All St. John’s Wort Is the Same
In 2021, a breakthrough changed the conversation. Researchers found that not all St. John’s Wort is created equal. Standard extracts contain 2-5% hyperforin. But a new generation of products now contains less than 1 mg of hyperforin per day. That’s a tiny amount-far below the level that triggers enzyme induction.Studies showed that with these low-hyperforin formulations, lopinavir levels dropped by only 12.3%, not 57%. That’s within acceptable limits. The University of Liverpool’s database now says: “Coadministration may be considered with St. John’s Wort formulations that clearly state the hyperforin content and which have a total daily hyperforin dose of 1 mg or less.”
But here’s the catch: only 37% of St. John’s Wort products sold in the U.S. actually list hyperforin content on the label. Most still say “standardized to 0.3% hypericin”-a completely different compound that doesn’t cause this interaction. That’s a dangerous loophole. You can’t trust a bottle that doesn’t tell you how much hyperforin it has.
What Happens When People Ignore the Warning
In 2021, a study of 2,450 HIV patients found that 8.3% had detectable levels of hyperforin in their blood-even though they were on protease inhibitors. Of those, 3.1% had clear virologic failure directly tied to the interaction. Based on CDC data from 2023, that translates to roughly 27,000 cases of potential treatment failure every year in the U.S. alone.Why does this keep happening? Because many patients don’t think of herbal supplements as “drugs.” They think, “It’s natural, so it’s safe.” But natural doesn’t mean harmless. St. John’s Wort interacts with over 50 medications, including blood thinners, birth control, and antidepressants. For someone with HIV, the stakes are life-or-death.
GoodRx’s 2024 analysis warns: “It’s not recommended to take St. John’s Wort with HIV medications.” And the Mayo Clinic says bluntly: “It could lessen the medicine’s effect.”
What Should You Do Instead?
If you’re on protease inhibitors and struggling with depression, St. John’s Wort is not your answer. But you don’t have to suffer either.- Ask your doctor about SSRIs like sertraline or escitalopram. These are safe with HIV meds.
- Consider therapy. Cognitive behavioral therapy (CBT) is proven to help with mild to moderate depression.
- If you’re already taking St. John’s Wort, stop it-and tell your provider immediately. Don’t wait.
- Never switch supplements without checking the hyperforin content. If it’s not listed, assume it’s dangerous.
Some people try to “dose low” or take it only occasionally. That doesn’t work. Even a single dose can trigger enzyme induction. There’s no safe middle ground with standard products.
The Bigger Picture: Regulation Is Lagging
The FDA and EMA have mandated warnings since 2003-2005. But herbal supplements aren’t held to the same standards as prescription drugs. Labels don’t have to prove safety, purity, or consistency. A bottle labeled “St. John’s Wort” could contain anything from 0.5 mg to 15 mg of hyperforin per capsule.That’s why the International Association of Providers of AIDS Care updated its 2024 guidelines to say: “Clinicians must ask every HIV patient about herbal supplement use at every visit.” This isn’t optional. It’s essential.
Future solutions may include hyperforin-free extracts or point-of-care blood tests to detect hyperforin levels. But for now, the rule is simple: if you’re on protease inhibitors, avoid St. John’s Wort unless you have a verified low-hyperforin product-and even then, only with your doctor’s approval.
Bottom Line: Don’t Risk Your Treatment
Your HIV meds are precise. They’re designed to keep your viral load undetectable. St. John’s Wort, even in small amounts, throws that precision off. The data is clear: this interaction causes treatment failure, resistance, and worse outcomes.If you’re thinking about trying St. John’s Wort for mood, anxiety, or sleep-stop. Talk to your doctor. There are safer, proven options. And if you’re already taking it, don’t wait for symptoms to appear. Get your viral load checked. Tell your provider. Your health isn’t worth the gamble.
Can I take St. John’s Wort if I’m on HIV meds?
No, not with standard St. John’s Wort products. It can drop your protease inhibitor levels by up to 80%, leading to treatment failure and drug resistance. Only consider low-hyperforin formulations (≤1 mg/day) if your provider approves and the label clearly states the hyperforin content.
How long does St. John’s Wort affect HIV drugs after I stop taking it?
The enzyme-inducing effect lasts at least 14 days after you stop. Your HIV meds may still be broken down too quickly during this time. Monitor your viral load and talk to your provider about possible dose adjustments.
Are all St. John’s Wort supplements the same?
No. Most contain 2-5% hyperforin, which causes dangerous interactions. Some newer products contain ≤1 mg of hyperforin per day and may be safer-but only if the label clearly states the amount. Many products don’t list hyperforin at all, making them unsafe.
What should I take instead of St. John’s Wort for depression?
SSRIs like sertraline, escitalopram, or fluoxetine are safe with HIV medications. Therapy, especially cognitive behavioral therapy (CBT), is also effective. Always talk to your doctor before starting any new treatment.
Why do some people still take St. John’s Wort with HIV meds?
Many believe herbal means safe, or they don’t tell their provider out of fear of judgment. Others don’t realize their supplement contains hyperforin. Studies show 15% of HIV patients on complementary therapies have tried St. John’s Wort despite warnings. That’s why doctors now ask about supplements at every visit.
8 Comments
kumar kc
January 21, 2026 at 01:38 AM
If you’re dumb enough to mix herbs with HIV meds, you deserve whatever happens.
Emily Leigh
January 21, 2026 at 05:16 AM
Okay but... like... isn’t it just so... ironic? We live in a world where you can buy a $30 supplement that’s basically a chemical weapon against your own body... and no one’s regulating it... but if you take a pill made in a lab that’s been tested on 12,000 people? Oh no, that’s ‘dangerous.’ 🙄 We’re all just playing Jenga with our lives and pretending the blocks are labeled.
Renee Stringer
January 21, 2026 at 11:15 AM
I understand the science. But I also understand that people are scared. They’re lonely. They’re depressed. And they don’t trust doctors who talk like they’re reading a textbook. So they turn to something that feels… gentle. That doesn’t mean they’re stupid. It means the system failed them first.
Shane McGriff
January 22, 2026 at 00:26 AM
Listen - I’ve been on ART for 12 years. I’ve seen people lose their minds over this stuff. But here’s the thing: if you’re on protease inhibitors and you’re thinking about St. John’s Wort, you’re not just risking your viral load - you’re risking your future. I get it. Depression sucks. But there are safe options. SSRIs? Therapy? Talking to someone who actually gets it? Do that. Not some bottle from a gas station that says ‘natural’ on it like it’s a badge of honor. You’re worth more than a gamble. Talk to your provider - today. Not tomorrow. Today.
pragya mishra
January 23, 2026 at 14:44 PM
Wait - so if I buy St. John’s Wort from Walmart, how do I know it’s not the dangerous kind? Do I need a lab report? Should I send a sample to a university? What if I can’t afford that? Who’s gonna help me? You just say ‘don’t do it’ like it’s that easy. I’m trying to survive, not pass a chemistry exam.
Andy Thompson
January 23, 2026 at 21:01 PM
THEY’RE HIDING THE TRUTH!! 🇺🇸🔥 St. John’s Wort is a gift from the Earth - but the FDA and Big Pharma are scared because it’s FREE and it WORKS. They made up this ‘enzyme’ nonsense to sell you $1,200/month antidepressants! They even put black boxes on the labels to scare you! Wake up! I’ve seen people get better on herbs while the pills made them zombies! 🌱💪 #FreeTheHerbs #HIVisACorporateLie
Thomas Varner
January 25, 2026 at 03:06 AM
So… the real issue isn’t the herb… it’s the label. Like… imagine if every pill bottle had to say ‘this contains 2.3mg hyperforin, may reduce lopinavir by 57%’ instead of ‘natural mood booster’? That’d be… actually helpful. But nah. We’d rather have a 10-page FDA warning and 37% of products not saying a word. So we’re stuck in this weird limbo where the science is crystal clear… but the packaging is a minefield. 😅

sagar sanadi
January 19, 2026 at 14:12 PM
So let me get this straight - the government says St. John’s Wort kills HIV meds, but they’re cool with Big Pharma selling pills that make you puke for 3 weeks? 🤔 Meanwhile, grandma in Kerala takes this herb for 40 years and still dances at weddings. Maybe the real problem is they don’t want you healing yourself? 🌿💀