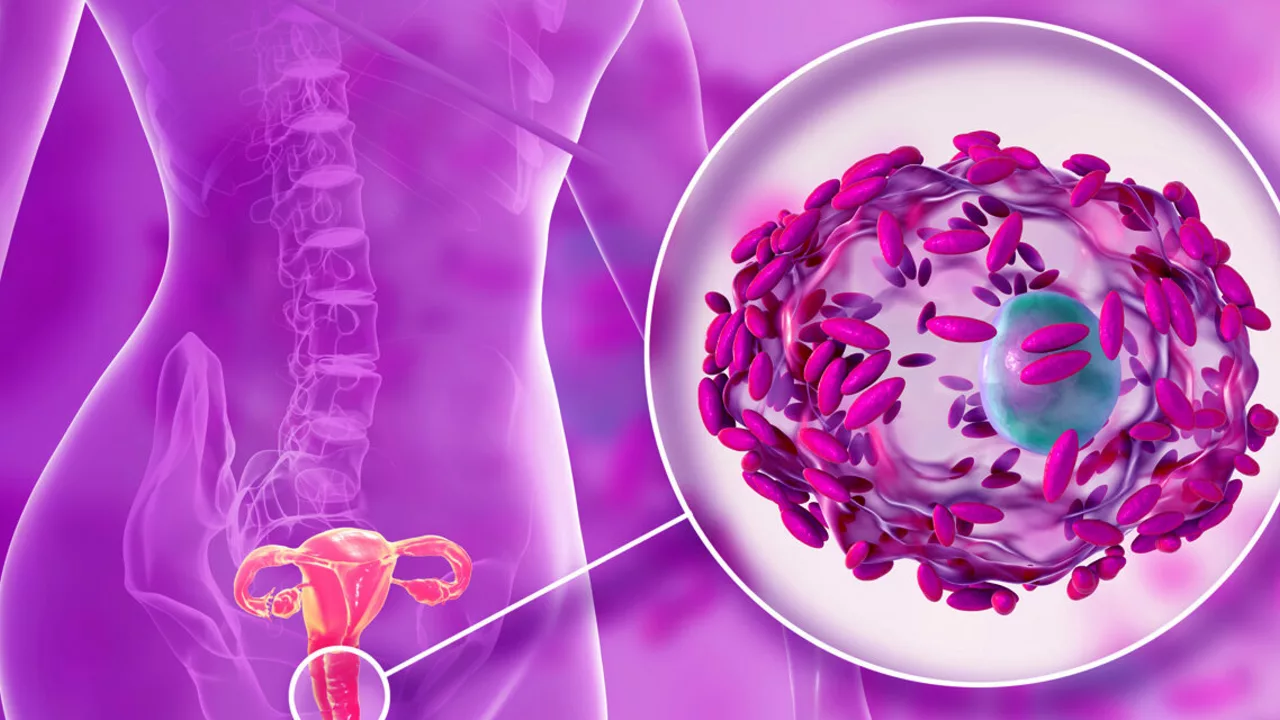
Bacterial vaginosis (BV) is the most common vaginal infection in women of childbearing age, yet it’s often misunderstood.
You may get unusual discharge, a fishy smell, or mild irritation — sometimes no symptoms at all. The cause? An imbalance in the normal vaginal bacteria, not a classic sexually transmitted infection. That matters because it changes how doctors treat it and how you can prevent repeat episodes.
If you suspect BV, a quick trip to a clinic or a telehealth visit usually sorts it out. Diagnosis is simple: a clinician checks symptoms, looks at discharge under a microscope, or runs a pH test. Treatment most often means a short course of antibiotics — oral metronidazole or a topical metronidazole or clindamycin — taken exactly as prescribed. Left untreated, BV can raise the risk of other infections and complications during pregnancy, so don’t ignore persistent symptoms.
Want to reduce your chances of getting BV again? Avoid douching, cut back on heavily scented soaps or washes around the vulva, and use condoms with new or multiple partners. Keeping sex toys clean and using water-based lubricants helps too. Some people find that finishing a full course of antibiotics and using a probiotic afterward reduces recurrences, though evidence varies. If you try over-the-counter products, check with a provider first to avoid delays in effective treatment.
Shopping for medications online?
Be careful. Look for verified online pharmacies, check for a physical address and pharmacist contact, and avoid sites offering prescription drugs without a prescription. Our site reviews several online pharmacies and guides on buying safely — read patient experiences, shipping times, and what to watch for before you click buy.
When should you see a doctor right away?
If you have fever, severe pain, heavy bleeding, or signs of an allergic reaction to medications, get urgent care. Also see a provider if symptoms come back within a month after treatment or if you’re pregnant and have any vaginal symptoms. Pregnant people with BV need prompt evaluation because BV can increase the risk of preterm birth.
Questions to ask your clinician: What antibiotic do you recommend and why? How long before symptoms should improve? Should I avoid sex during treatment? Will this affect my partner? Can I use probiotics and which ones? Clear answers make it easier to follow the plan and avoid trips back to the clinic.
If you want quick reads, check related pieces on our site: articles about antibiotic choices, safe online pharmacies, and ways to cut prescription costs. Use the tag page to find practical posts about treatment options, where to buy meds safely, and how to prevent repeat BV. If you need personalized advice, book a visit with a clinician — BV is common and treatable, but getting the right care fast matters.
Track symptoms, note triggers like new products or partners, and share that info with your clinician so they can tailor treatment. Sometimes longer antibiotic courses or partner treatment are needed — honest tracking speeds better results. Act early today.
The Connection Between Bacterial Vaginosis and Hormonal Changes
In my recent research, I've discovered an intriguing link between bacterial vaginosis and hormonal changes. It appears that hormonal fluctuations, particularly those related to menstrual cycles and menopause, can significantly impact the balance of bacteria in the vagina, leading to bacterial vaginosis. This condition is characterized by a shift in healthy bacterial levels, often resulting in discomfort and unpleasant symptoms. It's essential for women to understand this connection and seek appropriate treatment if they experience these changes. Keep in mind, maintaining hormonal balance can prove vital in preventing bacterial vaginosis.
View More


