Every year, tens of thousands of people end up in the hospital-not because their condition got worse, but because two medications they were taking clashed in their body. This isn’t rare. It’s happening right now to someone you know. Drug interactions aren’t just technical terms in a pharmacy brochure-they’re real, dangerous, and often completely preventable.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medication works in your body. That something could be another pill, a supplement, grapefruit juice, or even a health condition you already have. It doesn’t mean the drug is broken. It means something else is interfering with how it’s supposed to behave.
There are three main types:
- Drug-drug interactions: When one medication affects another. For example, taking the antibiotic clarithromycin with the blood thinner warfarin can make your blood too thin, increasing your risk of dangerous bleeding.
- Drug-food/drink interactions: When what you eat or drink changes how a drug is absorbed or broken down. Grapefruit juice is the most famous offender-it can make statins like simvastatin 300% to 600% more potent, leading to muscle damage or kidney failure.
- Drug-condition interactions: When an existing health problem changes how a drug works. For instance, if you have kidney disease, your body can’t clear certain drugs like ibuprofen as quickly, which can lead to toxic buildup.
These aren’t theoretical risks. According to a 2022 study in JAMA Internal Medicine, drug interactions cause around 106,000 deaths in the U.S. every year. That’s more than traffic accidents. And nearly 6.5% of all hospital admissions are linked to these kinds of mistakes.
How Do Interactions Actually Happen?
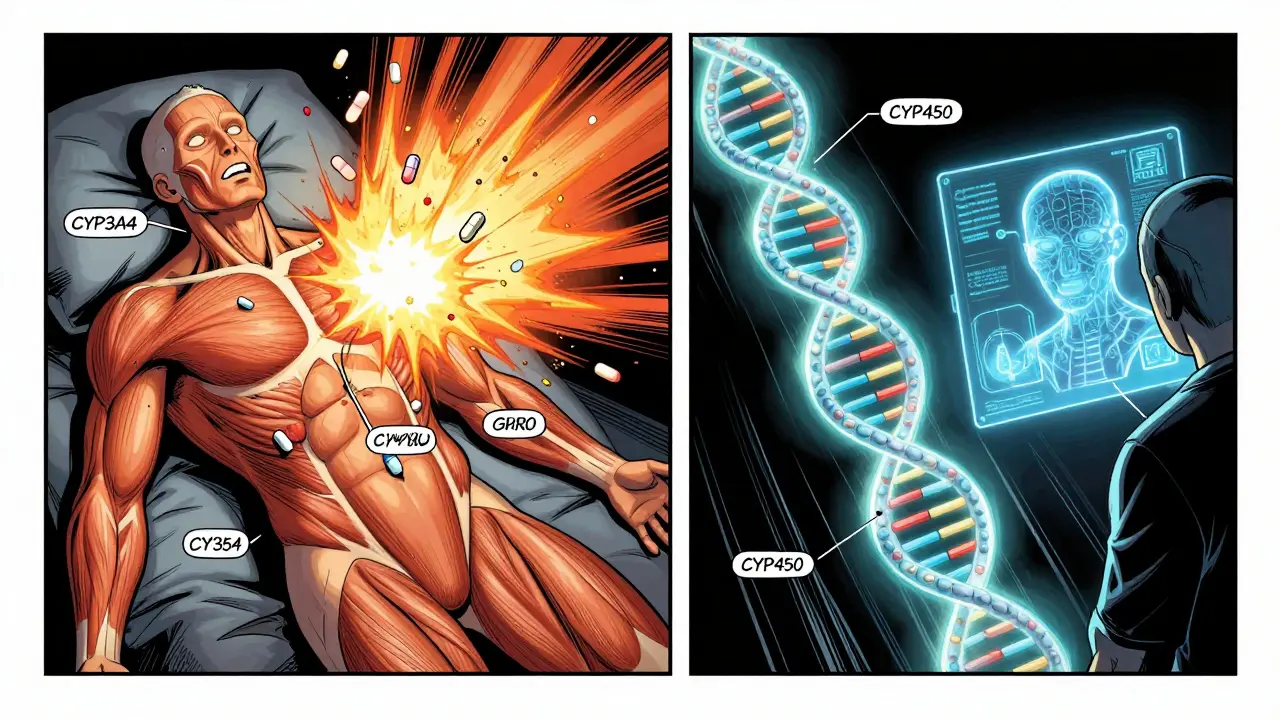
It’s not magic. It’s biology. Your body has systems designed to process drugs-mostly in the liver and gut. The most common players are enzymes called CYP450, especially CYP3A4. This enzyme breaks down about half of all prescription drugs. When something blocks or speeds up this enzyme, drug levels in your blood go haywire.
Take fluconazole (an antifungal) and simvastatin (a cholesterol drug). Fluconazole shuts down CYP3A4. That means simvastatin can’t be broken down. Its levels can spike by 2,000%. Result? Severe muscle breakdown called rhabdomyolysis, which can lead to kidney failure.
Then there’s the second kind: pharmacodynamic interactions. This is when two drugs hit the same target in your body-like two people pulling the same rope in opposite directions. For example, taking two sedatives (like a sleep pill and an anxiety med) can make you dangerously drowsy. Or NSAIDs like ibuprofen can block the effect of diuretics by making your body hold onto salt and water.
Some interactions are obvious. Others hide in plain sight. Levothyroxine (Synthroid), a thyroid hormone, won’t work properly if you take it with calcium, iron, or even coffee. The minerals bind to it in your gut and stop absorption. That’s why doctors tell you to take it on an empty stomach, 30 to 60 minutes before breakfast.
Why Are Some Drugs More Dangerous Than Others?
Not all medications are created equal when it comes to interactions. Some are like ticking bombs. Others barely notice what’s around them.
Warfarin (Coumadin) is the king of dangerous interactions. It has over 600 known substances that can affect it-antibiotics, antifungals, herbal supplements like St. John’s wort, even cranberry juice. Warfarin’s job is to thin your blood. Too little? Risk of clot. Too much? Risk of internal bleeding. A single interaction can flip your INR (a blood test that measures clotting) from safe to life-threatening in days.
Digoxin (Lanoxin), used for heart failure and irregular heartbeat, interacts with over 300 drugs. Diuretics can lower potassium, which makes digoxin more toxic. Antibiotics like erythromycin can cause digoxin levels to rise sharply. Both can lead to fatal heart rhythms.
Statins like atorvastatin and simvastatin are common, but they’re metabolized by CYP3A4. That means anything that affects this enzyme-grapefruit, certain antifungals, even some antibiotics-can turn a safe dose into a dangerous one.
Even over-the-counter meds can be risky. Cold medicines with pseudoephedrine can raise blood pressure dangerously if you’re on beta-blockers. Acetaminophen (Tylenol) can hurt your liver if you drink alcohol regularly or take other liver-metabolized drugs.

Who’s at the Highest Risk?
You might think drug interactions only affect older people. But it’s worse than that.
People over 65 make up only 16% of the U.S. population-but they account for 45% of serious drug interaction events. Why? Because they’re on more meds. The average elderly patient takes 4.7 prescription drugs daily. Add in supplements, OTC painkillers, and vitamins, and that number jumps.
Patients with five or more chronic conditions have a 68% chance of experiencing at least one significant interaction. That’s not a small risk. That’s a near certainty.
And it’s not just age. People seeing multiple doctors-cardiologist, endocrinologist, rheumatologist-are at higher risk because each provider may only see part of the picture. A 2022 study in the New England Journal of Medicine found that 34% of patients discharged from hospitals had at least one undocumented interaction risk because their medications weren’t fully reviewed.
Even young, healthy people aren’t safe. If you’re on birth control and start taking an antibiotic like rifampin, your birth control can fail. If you’re on antidepressants and take an OTC cold remedy with dextromethorphan, you could trigger serotonin syndrome-a rare but life-threatening condition.
What Can You Do to Stay Safe?
Knowing about interactions isn’t enough. You need to act.
- Keep a complete list of everything you take. Not just prescriptions. Include supplements, vitamins, herbal teas, and even OTC meds like ibuprofen or antacids. Write down the dose and how often you take it.
- Use one pharmacy. Pharmacies have systems that check for interactions across all your meds. If you spread prescriptions across multiple pharmacies, those systems can’t help you.
- Ask your pharmacist. They’re the medication experts. Don’t wait for them to ask you. Bring your list every time you pick up a new prescription. Say: “Can you check if this interacts with anything else I’m taking?”
- Be careful with grapefruit and alcohol. If you’re on a statin, calcium channel blocker, or certain psychiatric meds, avoid grapefruit juice entirely. Alcohol can make sedatives, painkillers, and antidepressants more dangerous.
- Time your doses. If you take levothyroxine, wait at least 4 hours before taking calcium or iron. Take warfarin at the same time every day to keep levels stable.
- Use trusted tools. The FDA-approved GoodRx Drug Interaction Checker and the free Medscape Drug Interaction Checker are reliable. Avoid random apps or websites without medical backing.
And if you’re over 65, ask your doctor if you should follow the Beers Criteria. It’s a list of 54 high-risk medications and interactions for older adults. Studies show using it reduces bad drug events by 27%.
Why Aren’t We Doing Better?
Here’s the uncomfortable truth: the system is broken.
The FDA requires drug interaction studies before approval-but only 25% of serious interactions are caught in clinical trials. Why? Because trials exclude older adults, people with multiple diseases, and those on multiple meds. The real world is messier.
Pharmaceutical companies often underreport risks. A 2022 study found that 73% of major interactions were only discovered after the drug hit the market.
Electronic health records (EHRs) show interaction alerts-but 58% of them are ignored because they’re too vague or too frequent. Doctors get alert fatigue. They start clicking “ignore” out of habit.
And patients? Only 30% get proper counseling about interactions, according to the Institute for Safe Medication Practices. Most people assume their doctor or pharmacist already checked everything. They don’t realize they need to be their own advocate.
What’s Changing?
There’s hope. The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable database with 12,000+ clinically validated interactions. It’s helping build smarter alert systems.
AI tools like IBM Watson Health are now scanning millions of patient records to find hidden interactions no one noticed before.
And the future? Pharmacogenomics. Testing your genes to see how you metabolize drugs. The FDA already includes genetic info for over 350 medications. By 2026, testing for CYP450 variants could become standard for high-risk drugs like warfarin or statins. That means your meds could be tailored to your biology-not a one-size-fits-all dose.
But until then, the most powerful tool you have is awareness. Not technology. Not algorithms. You.
Real Stories, Real Consequences
One patient on Reddit shared: “I took simvastatin for six months. No problems. Then I started drinking grapefruit juice every morning. Two days later, I couldn’t walk. My muscles were screaming. I ended up in the ICU with rhabdomyolysis.”
Another wrote: “My pharmacist caught that my new antidepressant would spike my blood pressure when mixed with my beta-blocker. She called my doctor. We switched meds before I even took the first pill. She saved my life.”
These aren’t outliers. They’re everyday stories. And they happen because someone didn’t ask the right question.
Medication safety isn’t just about the pill in your hand. It’s about everything around it-the juice you drink, the supplement you take, the other meds you forgot to mention, the condition your doctor didn’t think to ask about. It’s your body. It’s your health. You have the right-and the responsibility-to know how it all fits together.
What are the most common drug interactions?
The most common and dangerous ones involve warfarin (with antibiotics, antifungals, and even cranberry juice), statins (with grapefruit juice and certain antibiotics), and levothyroxine (with calcium, iron, and coffee). Drug-drug interactions make up about 80% of serious cases, while food-drug interactions like grapefruit juice account for another 15%.
Can over-the-counter meds cause drug interactions?
Yes. Even simple painkillers like ibuprofen or naproxen can reduce the effectiveness of blood pressure medications. Cold and flu remedies with pseudoephedrine can raise blood pressure dangerously if you’re on beta-blockers. Antacids with aluminum or magnesium can block absorption of antibiotics like tetracycline. Always check OTC meds with your pharmacist.
How do I know if a supplement interacts with my meds?
Many supplements aren’t tested for interactions like prescription drugs. St. John’s wort can make birth control, antidepressants, and warfarin less effective. Garlic and ginkgo can increase bleeding risk with blood thinners. Vitamin K can reduce warfarin’s effect. Always tell your pharmacist or doctor exactly what supplements you take-even if you think they’re "natural" or "safe."
Are drug interactions more dangerous for older adults?
Yes. Older adults are more likely to take multiple medications, have slower metabolism, and have reduced kidney or liver function. They’re also more sensitive to changes in drug levels. The American Geriatrics Society’s Beers Criteria identifies 54 high-risk medications and interactions specifically for people over 65. Following these guidelines can reduce adverse events by nearly a third.
What should I do if I think I’m having a drug interaction?
Stop taking the new medication or supplement immediately. Contact your pharmacist or doctor right away. Don’t wait for symptoms to get worse. Signs include unusual drowsiness, dizziness, rapid heartbeat, muscle pain or weakness, unexplained bruising or bleeding, confusion, or nausea. If symptoms are severe-like chest pain, trouble breathing, or loss of consciousness-go to the ER.


