When you take a proton pump inhibitor (PPI) like omeprazole for heartburn and an antifungal like itraconazole for a stubborn fungal infection, you might think you’re just managing two separate conditions. But in your body, these drugs are having a silent, potentially dangerous conversation - one that can leave you with too little medicine in your bloodstream to fight the infection.
Why Your Stomach Acid Matters More Than You Think
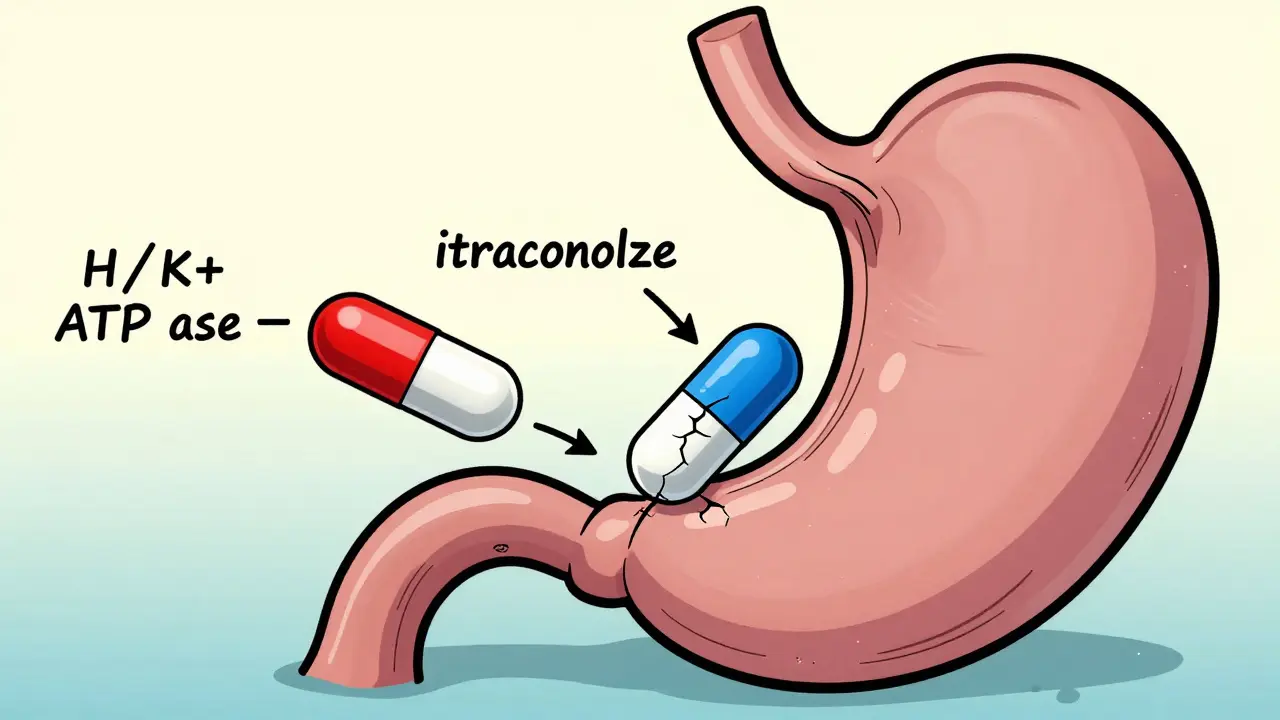
Most people don’t realize that stomach acid isn’t just there to digest food. It’s also a key player in how certain drugs get absorbed. Proton pump inhibitors work by shutting down the acid-producing pumps in your stomach lining. That’s great if you have GERD - your heartburn fades. But it’s a problem if you’re taking an antifungal that needs acid to dissolve properly. Itraconazole, one of the most commonly prescribed oral antifungals for serious infections like aspergillosis or coccidioidomycosis, is a weak base. That means it needs a low pH (high acid) to dissolve and get absorbed into your blood. When you take a PPI, your stomach pH rises from around 1-2 to 4-6. At that level, itraconazole doesn’t dissolve well. The result? Up to 60% less of the drug enters your bloodstream. A 2023 study in JAMA Network Open showed that when patients took omeprazole with itraconazole capsules, their overall drug exposure (measured as AUC) dropped by 60%. That’s not a small dip - it’s the difference between a therapeutic dose and a useless one. In some cases, patients with invasive fungal infections ended up with trough levels below 0.3 mcg/mL when they needed at least 0.5-1.0 mcg/mL to kill the fungus.Not All Antifungals Are Affected the Same Way
This isn’t a blanket rule. Some antifungals don’t care about your stomach pH at all. Fluconazole is one of them. It’s highly water-soluble, so it absorbs just fine whether your stomach is acidic or not. Studies confirm no meaningful drop in absorption even with long-term PPI use. If you’re on fluconazole for a yeast infection or candidiasis, you don’t need to worry about your PPI. Voriconazole is in the middle. It’s moderately affected - studies from the European Medicines Agency show about a 22% drop in absorption when taken with omeprazole. It’s not as bad as itraconazole, but it’s still enough to matter in serious cases like invasive aspergillosis. Posaconazole is tricky because it comes in two forms: an oral suspension and delayed-release tablets. The suspension is less affected by PPIs - only about a 15% drop. But the tablets? They lose up to 40% of their absorption. That’s why some pharmacists now recommend taking posaconazole tablets with a cola drink. The acidity in soda can help compensate for the lack of stomach acid. And then there’s itraconazole solution - a liquid form that’s already dissolved. Because it doesn’t rely on stomach acid to break down, the interaction with PPIs is minimal: only 10-15% reduction in absorption. That’s why, when possible, clinicians now prefer the solution over capsules for patients on PPIs.PPIs vs. Other Acid Reducers: Who’s the Real Culprit?
Not all acid-reducing drugs are created equal. H2 blockers like famotidine (Pepcid) or ranitidine also lower stomach acid, but not as deeply or as long. PPIs can keep your stomach pH elevated for 12-24 hours. H2 blockers last 4-10 hours. One study found that omeprazole reduced itraconazole absorption by 57%, while famotidine only cut it by 41%. That might sound like a small difference, but in life-threatening infections, every percentage point matters. Antacids? They’re different. They neutralize acid temporarily. If you take them 2 hours before or after your antifungal, they won’t interfere much. That’s why some patients are told to take their antifungal in the morning on an empty stomach, then take their antacid later with lunch.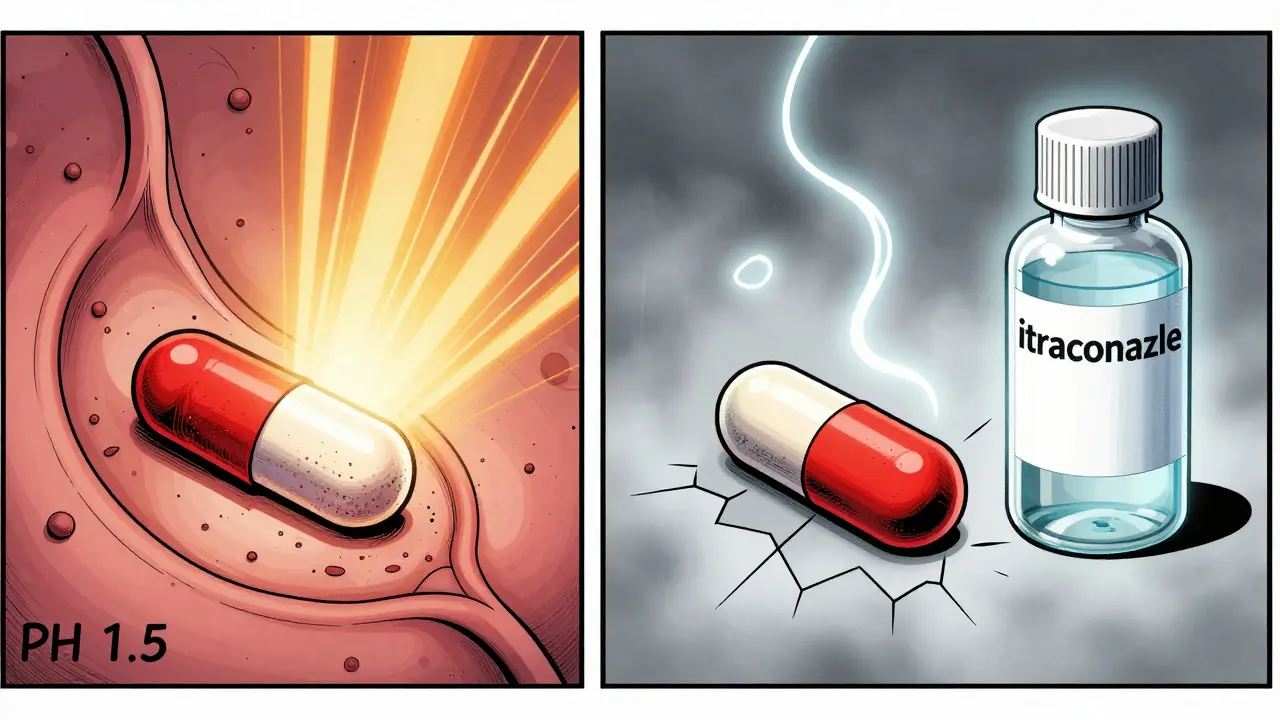
Real-World Consequences: When the Interaction Fails
This isn’t theoretical. In 2022, a survey of 1,247 hospital pharmacists found that 68% saw at least one case per month where a patient’s antifungal treatment failed because of a PPI interaction. Twenty-three percent reported confirmed treatment failures - patients who got sicker, needed longer hospital stays, or even died because their drug levels were too low. One case from Massachusetts General Hospital involved a patient with chronic pulmonary aspergillosis. His itraconazole levels were stuck at 0.3 mcg/mL - barely detectable. His doctors switched him from omeprazole to famotidine, dosed 10 hours after the antifungal. Within two weeks, his levels jumped to 1.7 mcg/mL. He went from being hospitalized to being discharged. Another patient at MD Anderson Cancer Center had invasive aspergillosis and needed both voriconazole and omeprazole. His team didn’t stop the PPI - they timed the doses. They gave voriconazole 2 hours before the PPI. That small adjustment kept his drug levels in the therapeutic range. Medicare data shows 38.7% of patients prescribed itraconazole capsules also got a PPI within the same month. That’s nearly 4 in 10. For the solution form? Only 12.3%. That gap tells you something: doctors are starting to learn.What to Do: Practical Steps to Avoid the Trap
If you’re prescribed an antifungal and you’re already on a PPI, here’s what you need to know:- For itraconazole capsules: Avoid PPIs entirely. Switch to fluconazole if possible. If you must use itraconazole, switch to the solution form.
- For itraconazole solution: You can take it with a PPI, but separate them by at least 2 hours. Take the antifungal first, then the PPI later.
- For posaconazole delayed-release tablets: Take with food and an acidic beverage like cola. Avoid PPIs if possible. If you can’t, monitor drug levels.
- For voriconazole: Try to separate doses by 2 hours. Monitor levels if you’re on long-term therapy.
- For fluconazole: No changes needed. It’s safe with PPIs.
The Unexpected Twist: Could PPIs Actually Help?
Here’s the curveball: recent lab studies suggest PPIs might actually help fight some fungal infections - but only in combination. A 2025 study in Frontiers in Pharmacology found that when omeprazole and itraconazole were mixed together in a lab dish, they worked better than either drug alone - especially against azole-resistant strains of Aspergillus fumigatus. In 77.6% of cases, the combination killed the fungus more effectively. That’s not a mistake. It’s a discovery. Researchers at the National Institutes of Health are now running a Phase I trial (NCT05678901) to test whether low-dose omeprazole can boost the effect of low-dose itraconazole in patients with drug-resistant aspergillosis. The idea? Maybe we’re not just dealing with a drug interaction - maybe we’re seeing a hidden synergy. It’s early, but if this works, we could be looking at a whole new way to treat resistant fungal infections - by turning a problem into a tool.New Solutions Are Coming
The pharmaceutical industry is responding. In 2023, the FDA approved a new version of itraconazole called Tolsura. Unlike the old capsules, Tolsura is designed to absorb regardless of stomach pH. In trials, it showed only an 8% drop in absorption with PPIs - compared to 50-60% for the old capsules. This isn’t just a minor upgrade. It’s a game-changer. Patients who need long-term antifungal therapy and also have ulcers, GERD, or are on blood thinners can now take both drugs without the risk of treatment failure. The American Gastroenterological Association and IDSA are working on updated guidelines expected by the end of 2024. They’ll likely recommend Tolsura over older itraconazole formulations when PPIs are needed.Bottom Line: Know Your Drugs, Protect Your Treatment
If you’re on a proton pump inhibitor and your doctor prescribes an antifungal, don’t assume everything’s fine. Ask: Which antifungal is it? Is it a capsule or a solution? Do I need to change how I take my PPI? This interaction isn’t rare. It’s common. And it’s deadly if ignored. But it’s also avoidable - with the right knowledge, timing, and sometimes, a simple switch in medication. The best outcome? You don’t just survive the infection. You get treated properly the first time.Can I take fluconazole with a proton pump inhibitor?
Yes. Fluconazole is highly water-soluble and doesn’t rely on stomach acid for absorption. Multiple studies confirm that PPIs like omeprazole, pantoprazole, or lansoprazole do not reduce fluconazole levels in the blood. You can take them together without any dose adjustments or timing changes.
Why does itraconazole capsule fail with PPIs but the solution doesn’t?
Itraconazole capsules contain solid particles that need to dissolve in stomach acid to be absorbed. When PPIs raise stomach pH above 3, the drug doesn’t dissolve well - leading to up to 60% less absorption. The solution form, however, is already dissolved in liquid. It doesn’t need acid to break down, so PPIs have little to no effect - absorption drops by only 10-15%.
What should I do if I’m on both itraconazole and omeprazole?
If you’re on itraconazole capsules, stop the omeprazole if possible. Switch to fluconazole instead. If you can’t stop the PPI, ask your doctor about switching to itraconazole solution and take it at least 2 hours before your PPI. For severe infections, therapeutic drug monitoring (measuring blood levels) is recommended to ensure you’re getting enough drug.
Can I take antacids with antifungals if I’m on a PPI?
Yes, but timing matters. Antacids neutralize acid temporarily. If you take them 2 hours before or after your antifungal, they won’t interfere significantly. However, if you’re already on a PPI, antacids won’t help restore acid levels - they’re just a short-term fix. The real solution is switching to an antifungal that doesn’t need acid, like fluconazole or itraconazole solution.
Is there a new itraconazole that works with PPIs?
Yes. Tolsura, approved by the FDA in 2023, is a new formulation of itraconazole designed for pH-independent absorption. Unlike older capsules, it doesn’t rely on stomach acid to dissolve. Studies show it loses only 8% of its absorption when taken with PPIs - compared to 50-60% for the old version. If you need long-term antifungal therapy and a PPI, Tolsura is now the preferred choice.
10 Comments
Lana Kabulova
January 24, 2026 at 14:02 PM
Wait-so if you’re on omeprazole and get prescribed itraconazole capsules, you’re basically getting a placebo? That’s not a drug interaction-it’s a medical malpractice waiting to happen. And why isn’t this on every prescription label?!!? Someone’s getting rich off this. Someone’s dying. And we’re all just scrolling past it.
Rob Sims
January 26, 2026 at 07:01 AM
Oh wow, so the real villain isn’t the fungus-it’s the guy who wrote the PPI prescription without checking the antifungal. Classic. I mean, I get it-doctors are busy. But if your solution is ‘just take it with cola,’ maybe your entire medical education needs a reboot. 🤡
arun mehta
January 26, 2026 at 18:19 PM
Thank you for this deeply insightful breakdown 🙏
As a healthcare professional from India, I’ve seen too many patients suffer because of this exact interaction. The fact that fluconazole remains unaffected is a gift. And Tolsura? A true breakthrough. Let’s hope global access follows soon. 🌍💊
Knowledge saves lives. Keep sharing.
Chiraghuddin Qureshi
January 26, 2026 at 22:00 PM
India has over 200 million people on PPIs. Imagine how many are unknowingly getting robbed of antifungal efficacy. This needs to be in every Ayurvedic clinic, every rural pharmacy. We need posters. We need WhatsApp blasts. We need awareness. 🙏🫶
Kenji Gaerlan
January 27, 2026 at 13:34 PM
so like... if u take pepcid instead of omeprazole u cool? or is it still bad? idk man i just want my heartburn to stop
Oren Prettyman
January 28, 2026 at 11:21 AM
It is not merely a pharmacokinetic interaction-it is a systemic failure of prescriber education, regulatory oversight, and pharmaceutical transparency. The fact that this interaction has persisted for over two decades, despite documented evidence, suggests a profound institutional apathy toward patient safety. One must question whether the pharmaceutical-industrial complex prioritizes profit margins over physiological integrity. The absence of mandatory drug interaction alerts in EHR systems is not an oversight-it is complicity.
Tatiana Bandurina
January 29, 2026 at 11:26 AM
Did you know that in 2021, the FDA received 3,421 adverse event reports related to antifungal treatment failure? Only 12% mentioned PPI use. That’s not patient ignorance. That’s provider negligence. And now you’re telling me the solution is ‘take it with cola’? That’s not a workaround-it’s a joke wrapped in a prescription.
Philip House
January 30, 2026 at 18:44 PM
Look. I’ve been to med school. I’ve seen the data. But here’s the thing-this isn’t about science. It’s about control. Who decides what gets approved? Who profits when you switch from capsules to solution? Who gets paid when you prescribe Tolsura instead of the generic? It’s not the patient. It’s not the doctor. It’s the boardroom. And now they’re selling us ‘cola therapy’ like it’s a miracle. Wake up.
Akriti Jain
January 30, 2026 at 23:56 PM
They say PPIs help fungal infections in labs? LOL. Of course they do. That’s the same way they said aspartame was safe. They’re testing it with low-dose itraconazole because they want to make you think the problem is fixable. But the real agenda? Keep you on both drugs forever. And charge you twice. 🧪💰




Lauren Wall
January 23, 2026 at 10:08 AM
Wow. So we’re just letting Big Pharma profit off of patients who don’t know their meds are canceling each other out? 🤦♀️