Biologic Medications: What They Are, How They Work, and What You Need to Know
When you hear biologic medications, complex drugs made from living organisms that target specific parts of the immune system. Also known as biologics, they’re not like regular pills — they’re injections or infusions designed to stop inflammation at its source. These aren’t new, but they’ve changed how we treat serious conditions like rheumatoid arthritis, psoriasis, Crohn’s disease, and even some cancers. Unlike traditional drugs that affect your whole body, biologics go straight for the troublemakers — like TNF-alpha or IL-17 — leaving other systems mostly alone.
That’s why they work so well for people who haven’t responded to older meds. But they’re not magic. Because they quiet down your immune system, you’re more at risk for infections — think TB, pneumonia, or even fungal infections. Some people develop rashes or fatigue. And because they’re made from proteins, your body might react to them over time, making them less effective. That’s where biosimilars, highly similar versions of original biologics, approved after patents expire come in. They’re cheaper, and studies show they work just as well for most people. But they’re not generics — you can’t swap them in like you would with metformin or lisinopril. Your doctor has to prescribe them specifically.
Biologics don’t work the same for everyone. Some people get relief fast — in weeks. Others take months. And if one stops working, switching to another type — say, from a TNF blocker to an IL-23 inhibitor — can make all the difference. That’s why knowing your options matters. You’ll also need regular blood tests to watch for liver issues or low blood cell counts. And if you’re on one of these, you should avoid live vaccines. The good news? Many people stay on biologics for years without major problems, especially when they’re paired with healthy habits and smart monitoring.
These treatments are often used for autoimmune diseases, conditions where the immune system mistakenly attacks the body’s own tissues — things like lupus, multiple sclerosis, and ulcerative colitis. But they’re also being studied for new uses every year. What’s clear is that they’re not a one-size-fits-all fix. You need to understand your condition, your risks, and how these drugs fit into your life. That’s why the posts below cover real patient experiences, side effect timelines, drug interactions, and how biologics compare to other treatments like small-molecule drugs. Whether you’re just starting out or switching therapies, you’ll find practical advice that cuts through the noise.
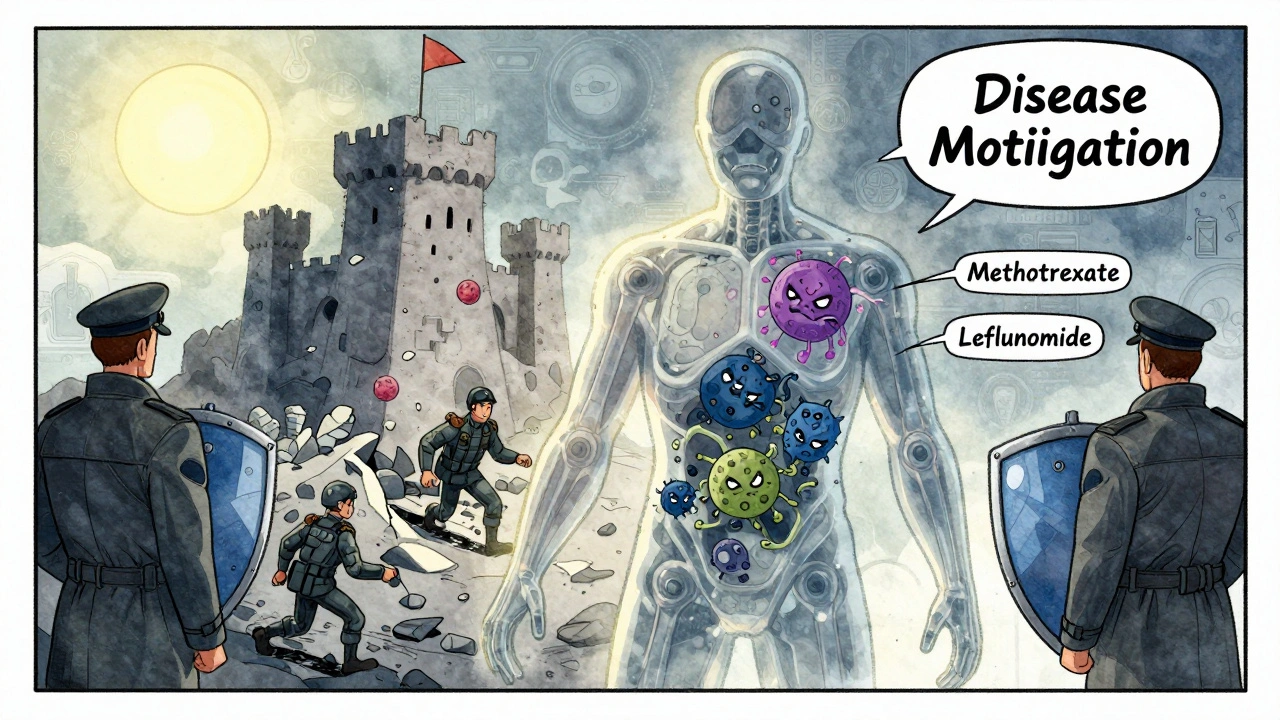
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are cornerstone treatments for autoimmune diseases like rheumatoid arthritis. Learn how they work, their differences, risks, costs, and what to expect when starting therapy.
View More