DMARDs: What They Are, How They Work, and Which Conditions They Treat
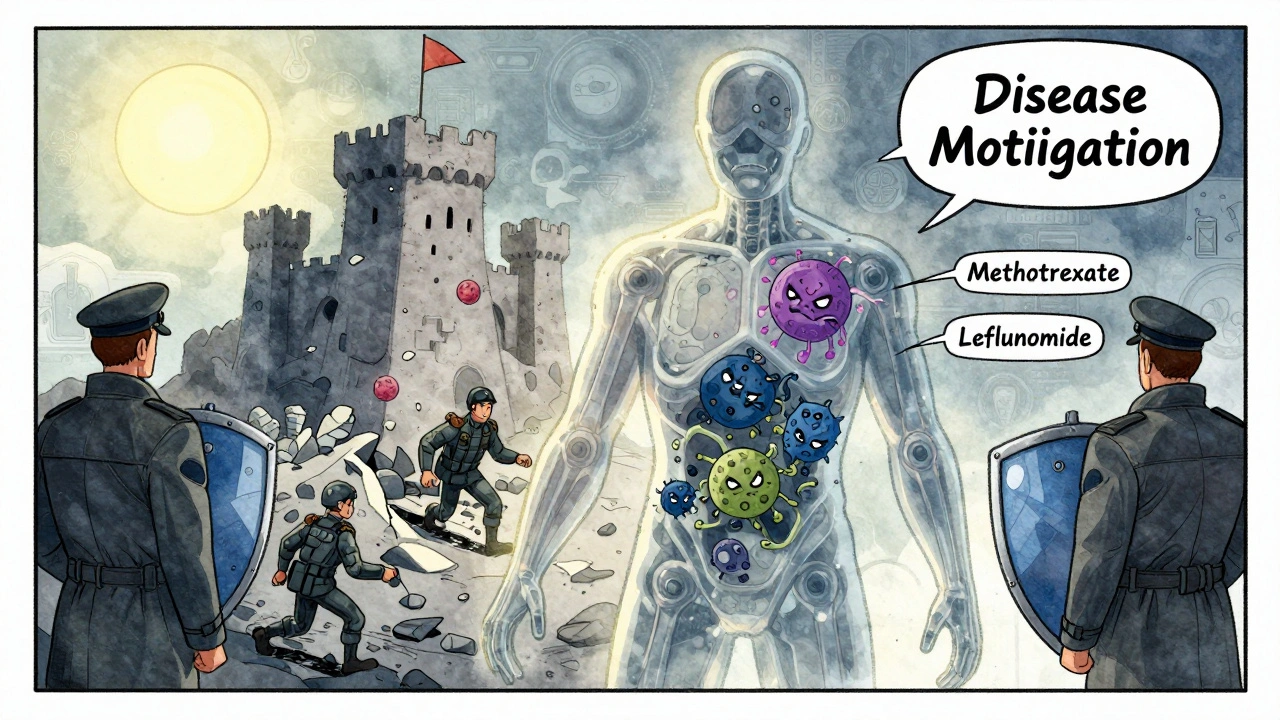
When your immune system turns on your own body, DMARDs, disease-modifying antirheumatic drugs that slow or stop autoimmune damage. Also known as disease-modifying drugs, they don’t just ease pain—they change the course of diseases like rheumatoid arthritis, psoriatic arthritis, and lupus. Unlike painkillers or anti-inflammatories, DMARDs work deep inside your immune system to calm the attack before it destroys joints, skin, or organs. They’re not quick fixes. It can take weeks or months to feel the full benefit, but that’s when the real win happens: less joint damage, fewer flares, and a better chance at staying active.
There are two main types: traditional DMARDs and biologic DMARDs. Methotrexate, the most common traditional DMARD, often the first choice for rheumatoid arthritis, is cheap, effective, and used for decades. Biologic DMARDs, targeted drugs like adalimumab or etanercept that block specific immune signals, came later. They’re more powerful but also more expensive and carry higher infection risks. Both types are used for autoimmune diseases, conditions where the body attacks its own tissues—not just arthritis, but also Crohn’s, ulcerative colitis, and even severe psoriasis. What they all share is one goal: stop the immune system from running wild.
Timing matters. Starting DMARDs early can prevent permanent damage. Waiting until your joints are already deformed means you’re fighting damage, not preventing it. That’s why doctors push for early diagnosis and early treatment—even if your symptoms feel mild. And while side effects like liver stress, low blood counts, or infections can happen, they’re monitored closely with regular blood tests. Most people tolerate them fine when tracked properly.
You’ll find posts here that dig into how DMARDs compare to other treatments, what happens when they stop working, and how they interact with common meds like NSAIDs or antidepressants. Some articles explain why certain patients respond better to one type over another. Others cover the real-life trade-offs—like managing fatigue, avoiding infections, or dealing with long-term use. There’s no one-size-fits-all answer, but the information here is grounded in what actually works for patients—not just theory.
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are cornerstone treatments for autoimmune diseases like rheumatoid arthritis. Learn how they work, their differences, risks, costs, and what to expect when starting therapy.
View More