Immunosuppressive Therapy: What It Is, How It Works, and What You Need to Know
When your immune system turns against your own body, it can cause serious damage — attacking joints, skin, liver, or even transplanted organs. That’s where immunosuppressive therapy, a medical approach that reduces immune system activity to prevent damage. Also known as immunosuppression, it’s not about weakening your body — it’s about stopping it from attacking itself. This therapy is used for conditions like autoimmune hepatitis, a chronic liver disease where the immune system destroys liver cells, after organ transplant, when the body tries to reject the new organ, and in diseases like lupus or rheumatoid arthritis.
Drugs used in this therapy fall into a few main groups. corticosteroids, like prednisone, reduce inflammation and immune activity quickly but aren’t meant for long-term use because of side effects like weight gain, bone loss, and high blood sugar. Then there are immunosuppressant drugs, such as tacrolimus, cyclosporine, and mycophenolate, that target specific immune cells over time. These are the backbone of transplant care and long-term autoimmune treatment. They work slower but last longer, and often get combined to lower doses and reduce risks. The goal isn’t to shut down your immune system completely — it’s to dial it back just enough to stop the attack without leaving you defenseless against infections.
People on these drugs need regular monitoring. Blood tests check for signs of infection, liver stress, or kidney changes. Some meds interact with common drugs like antibiotics or grapefruit juice, which can spike levels dangerously. You’ll also need to be extra careful about vaccines — live vaccines are usually off-limits. The biggest fear isn’t the disease anymore — it’s the side effects of the treatment. But for many, the trade-off is worth it: avoiding liver failure, kidney damage, or transplant rejection.
Below you’ll find real, practical guides on how these drugs affect the body, what to watch for, and how they connect to other conditions like liver disease, drug interactions, and long-term health risks. Whether you’re on this therapy, caring for someone who is, or just trying to understand why someone needs to take powerful meds for life — this collection gives you clear, no-fluff answers.
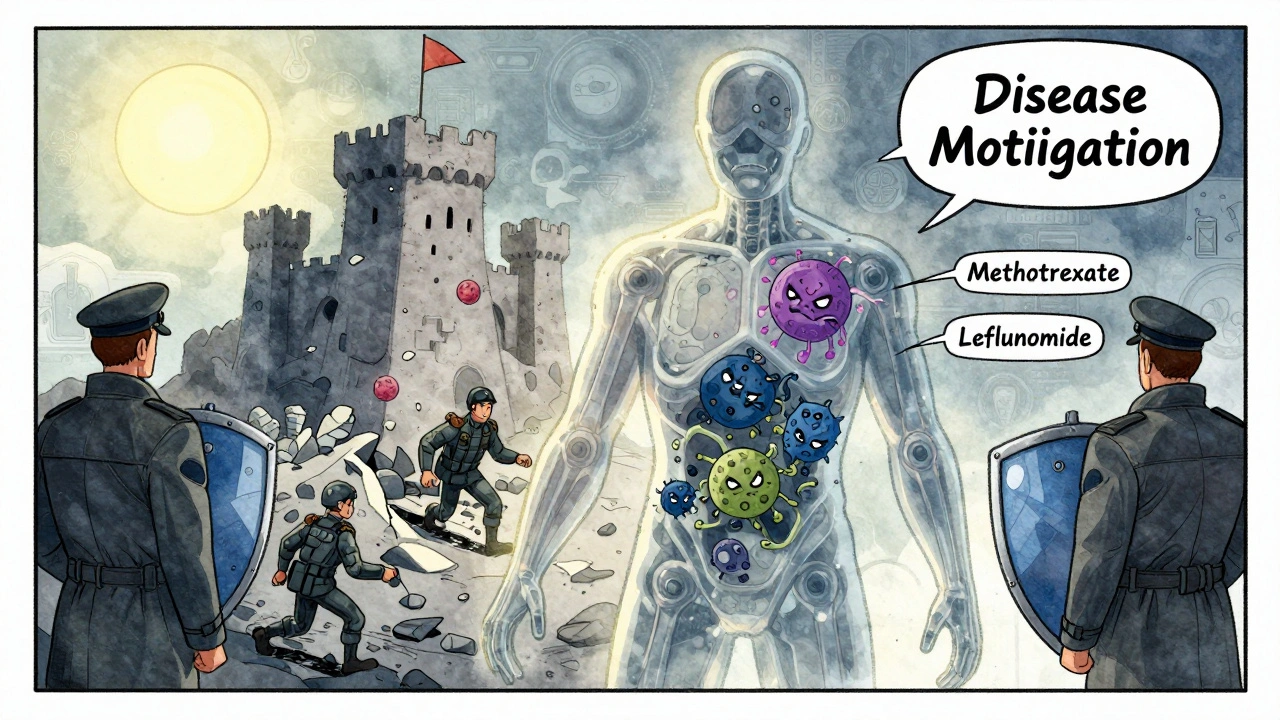
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are cornerstone treatments for autoimmune diseases like rheumatoid arthritis. Learn how they work, their differences, risks, costs, and what to expect when starting therapy.
View More