Rheumatoid Arthritis: Causes, Treatments, and What Works Best
When your immune system turns on your own joints, you’re dealing with rheumatoid arthritis, a chronic autoimmune disease where the body attacks the lining of joints, leading to pain, swelling, and long-term damage. Also known as RA, it doesn’t just affect hands and knees—it can hit the lungs, heart, and eyes too. Unlike regular wear-and-tear arthritis, rheumatoid arthritis flares up randomly and often starts in small joints like fingers and toes before spreading. It’s not just aging—it’s your immune system misfiring, and it affects about 1.3 million people in the U.S. alone.
People with rheumatoid arthritis often struggle with morning stiffness that lasts over an hour, fatigue that doesn’t go away with rest, and joints that feel warm or swollen. Over time, without proper treatment, the damage can become permanent. That’s why early diagnosis matters. Doctors look for specific antibodies like RF and anti-CCP in blood tests, plus imaging like X-rays or MRIs to spot joint erosion. But here’s the thing: you don’t need to wait for full damage to start treatment. The goal isn’t just to manage pain—it’s to stop the immune system from destroying your joints in the first place.
DMARDs, disease-modifying antirheumatic drugs, are the first-line treatment for rheumatoid arthritis and work by slowing or stopping the immune attack.Methotrexate is the most common, often used alone or with other drugs. If that’s not enough, biologic drugs, targeted therapies that block specific parts of the immune system like TNF-alpha or IL-6 come in—drugs like Humira, Enbrel, or Orencia. These aren’t magic bullets, but for many, they mean the difference between being able to hold a cup or not. And yes, they come with risks—like higher infection rates—but when monitored, they’re far safer than letting RA run wild.
Some people wonder if diet, supplements, or acupuncture can replace meds. The answer? They might help with symptoms, but they won’t stop joint damage. You still need the right drugs. And while steroids like prednisone give quick relief, they’re not for long-term use—too many side effects. Physical therapy, gentle exercise, and pacing your activity help too. But none of that works if the core problem—the autoimmune attack—isn’t addressed.
What you’ll find below are real, practical guides on how RA connects to other conditions, what medications are safest, how side effects show up over time, and what to do when treatments stop working. No fluff. Just what you need to know to protect your joints, avoid dangerous interactions, and live better with this condition.
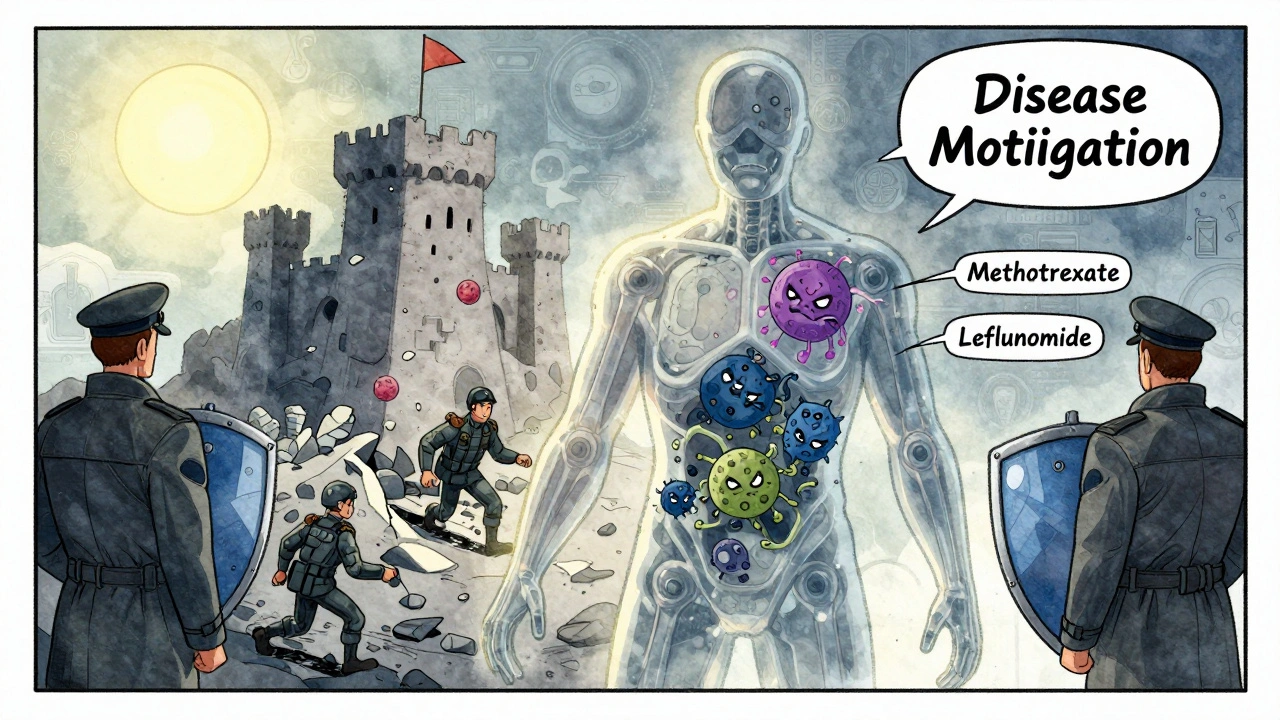
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are cornerstone treatments for autoimmune diseases like rheumatoid arthritis. Learn how they work, their differences, risks, costs, and what to expect when starting therapy.
View More