Rifampin Drug Interaction Checker
Check if your current medications interact with rifampin. Select all medications you're taking:
When treating tuberculosis, rifampin is one of the most powerful drugs doctors have. It cuts the treatment time from 18 months down to just six. That’s a huge win. But here’s the catch: rifampin doesn’t just kill TB bacteria-it also messes with almost every other medication you’re taking. If you’re on birth control, blood thinners, HIV meds, or even common stomach drugs, rifampin could make them useless. And you might not even know it until something goes wrong.
How Rifampin Actually Works
Rifampin, also called rifampicin, attacks tuberculosis by shutting down the bacteria’s ability to make RNA. Without RNA, the bacteria can’t build proteins or reproduce. It’s targeted, precise, and doesn’t touch human cells. A single 600 mg dose reaches peak levels in your blood within about two hours, hitting around 7 mcg/mL. But if you take it with food, absorption drops by nearly a third. That’s why it’s always recommended on an empty stomach-usually one hour before breakfast.
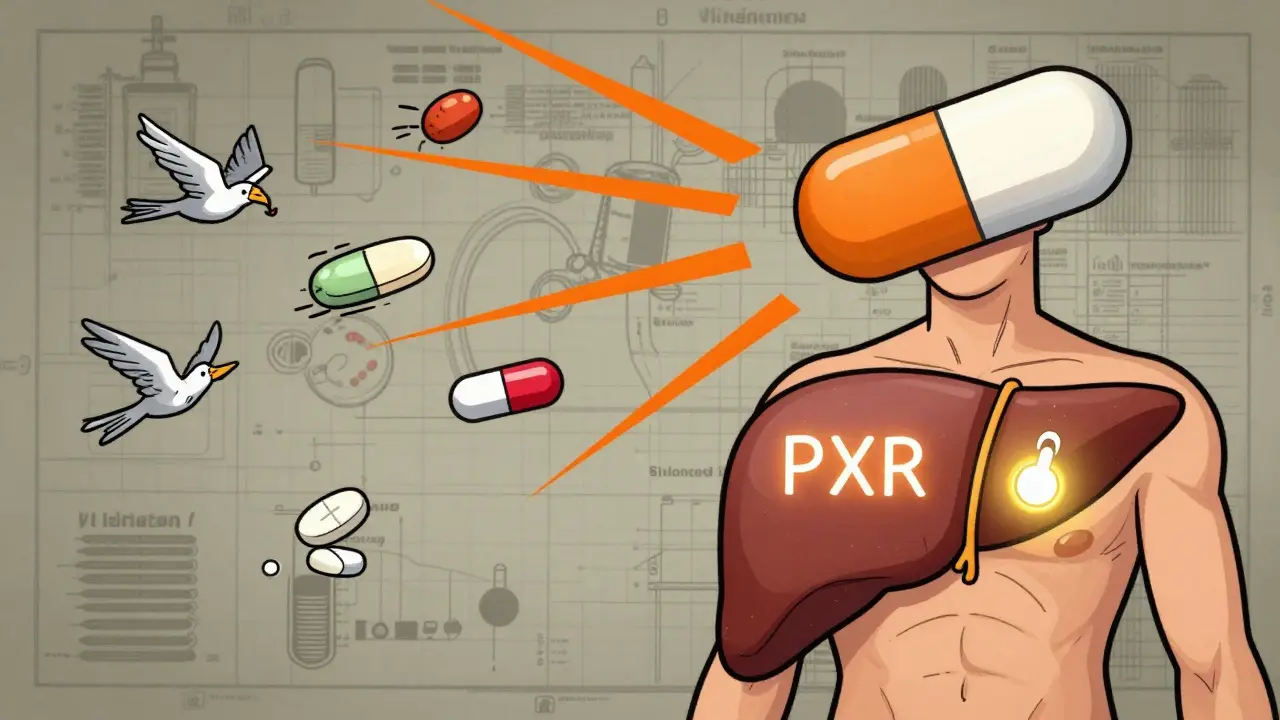
It’s not just effective-it’s fast. Within 24 hours of your first dose, your body starts changing how it handles other drugs. That’s because rifampin activates something called the pregnane X receptor, or PXR. Think of PXR as a master switch that flips on a whole set of liver enzymes, especially CYP3A4. This enzyme is responsible for breaking down over half of all prescription medications. When rifampin turns it up, those drugs get cleared out of your system too quickly.
The Hidden Danger: Drug Interactions
Let’s say you’re on warfarin to prevent blood clots. Your doctor carefully adjusts your dose so your INR stays in the safe range. Then you start rifampin for TB. Within a week, your INR drops. Why? Rifampin boosts CYP3A4 activity by 200-400%. Warfarin gets metabolized faster. Your blood doesn’t thin enough. Suddenly, you’re at risk for a stroke or pulmonary embolism.
The same thing happens with oral contraceptives. Studies show rifampin reduces estrogen levels by up to 67%. Women on birth control pills can get pregnant-even if they take them perfectly. There are documented cases of unplanned pregnancies in women taking both drugs. No warning. No red flag. Just a missed period and a positive test.
HIV medications are even more dangerous. Protease inhibitors like ritonavir and atazanavir can lose up to 90% of their effectiveness with rifampin. That’s not just a drop in efficacy-it’s a gateway to drug-resistant HIV. In places where TB and HIV overlap, this interaction has led to treatment failures and outbreaks of multi-drug resistant strains.
Even common drugs like statins, antidepressants, and antifungals can become unsafe. Simvastatin, for example, can build up to toxic levels if taken with rifampin after the enzyme induction wears off. That’s because rifampin’s effects linger for two weeks after you stop taking it. The enzymes it induced don’t disappear overnight. They stick around, slowly fading. So if you stop rifampin and immediately start a new medication, you’re still at risk.
Rifampin’s Strange Paradox: Helping TB Survive
Here’s the twist: rifampin doesn’t just affect your body-it affects the bacteria too. Research shows that within hours of exposure, *Mycobacterium tuberculosis* starts fighting back. At low doses, rifampin triggers the bacteria to produce more of a protein called RpoB, which helps them survive the drug’s effects. This isn’t resistance in the traditional sense-it’s tolerance. The bacteria aren’t genetically changed. They’re just better at hiding.
Even worse, the bacteria activate efflux pumps-tiny molecular valves that push rifampin out before it can kill them. These pumps are turned on within 48 hours of infection in immune cells. That’s why TB treatment takes so long. Even if most bacteria die, this hidden population survives, ready to come back if treatment stops too soon.
That’s why six months is the minimum. Shorter courses? Relapse rates jump to over 25%. The bacteria aren’t gone-they’re just waiting.
What Can You Do? Managing Interactions
There’s no way around rifampin’s power. But there are ways to manage it.
First: Know your meds. Tell your doctor every pill, patch, or supplement you take. That includes over-the-counter painkillers, herbal teas, and vitamins. Even St. John’s wort can interfere.
Second: Time matters. If you need to start a new drug after rifampin, wait at least two weeks. For high-risk drugs like warfarin or certain HIV meds, wait four weeks. Don’t guess. Ask.
Third: Use alternatives. If you’re on birth control, switch to an IUD or implant. They’re not affected by rifampin. If you’re on a statin, switch from simvastatin to pravastatin or rosuvastatin-they’re less dependent on CYP3A4.
Fourth: Monitor closely. If you’re on warfarin, check your INR weekly during the first month of rifampin. If you’re on HIV meds, your viral load should be checked every four weeks. Don’t assume everything’s fine because you feel okay.
New Hope: Blocking the Bacteria’s Escape Routes
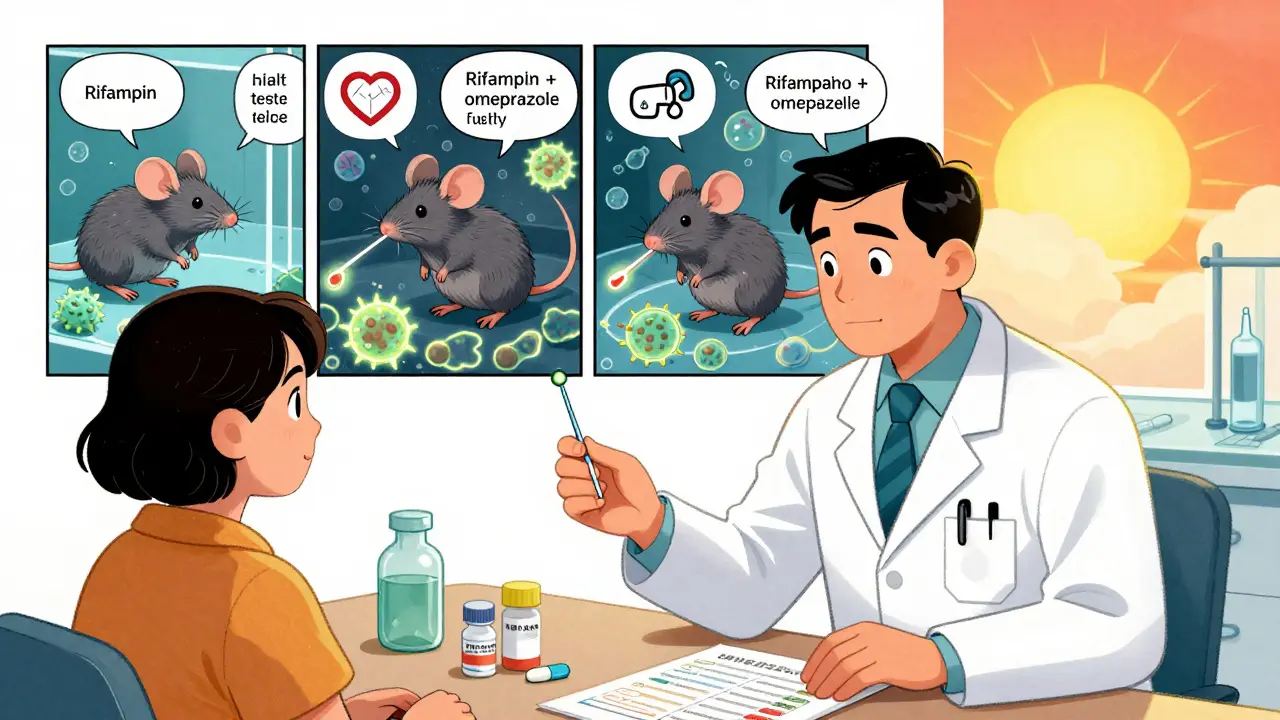
Scientists are now looking at ways to outsmart the bacteria’s defense system. One promising idea? Use drugs already on the shelf to block those efflux pumps.
Verapamil, a heart medication, and omeprazole, a common acid reducer, have both been shown to block the pumps that push rifampin out of TB bacteria. In lab studies, omeprazole blocked up to 68% of the efflux. That means more rifampin stays inside the bacteria, killing them faster.
Early trials in mice show that adding omeprazole to standard TB treatment cuts relapse rates from 25% to under 5%. Human trials are now underway. If they work, we might be able to shorten TB treatment from six months to three. That’s life-changing-not just for patients, but for global health systems struggling to keep up.
Side Effects You Can’t Ignore
Rifampin isn’t just about interactions. It can hurt your liver. About 1 in 5 people on TB treatment with rifampin see their liver enzymes rise above safe levels. That doesn’t always mean symptoms-but it’s a warning. If you notice dark urine, yellow eyes, or constant nausea, get tested immediately.
It also turns your bodily fluids orange. Urine, sweat, tears-even contact lenses can get stained. It’s harmless, but startling. Tell patients upfront so they don’t panic.
And yes, it can cause itching. That sounds odd, but it’s real. In people with liver disease, rifampin actually helps relieve itching by helping the body break down bile acids. It’s one of the few drugs that turns a side effect into a treatment.
Why This Matters Beyond TB
Rifampin is used in other infections too-like MRSA, Lyme disease, and even some cases of prosthetic joint infections. Every time it’s used, the same risks apply. A patient on rifampin for a joint infection might also be on a blood thinner or antidepressant. The interaction risk doesn’t disappear just because the infection isn’t TB.
And globally, over 3.5 million people start rifampin-based TB treatment every year. That’s millions of people who need to be monitored, educated, and followed up. Missing one interaction can cost a life.
Understanding rifampin isn’t just about TB. It’s about learning how one drug can ripple through an entire system-your body, your meds, your bacteria, and your future health.
Can rifampin make birth control pills ineffective?
Yes. Rifampin reduces the effectiveness of oral contraceptives by up to 67% by speeding up how fast your body breaks down estrogen and progestin. Even perfect use won’t prevent pregnancy. Switch to an IUD, implant, or injection-these are not affected by rifampin.
How long do rifampin’s drug interactions last after stopping?
Rifampin’s effects on liver enzymes can last up to two weeks after you stop taking it. For drugs with narrow therapeutic windows-like warfarin or certain HIV meds-wait four weeks before starting them. Don’t assume the interaction ends when you finish your TB course.
Why does TB treatment take six months if rifampin kills bacteria fast?
Rifampin kills most TB bacteria quickly, but a small group survives by activating efflux pumps and increasing protective proteins. These dormant bacteria can restart the infection if treatment stops too soon. Six months ensures they’re fully wiped out. Shorter courses lead to relapse in over 25% of cases.
Can I take omeprazole with rifampin for my stomach?
Yes, and it might even help. Omeprazole can block the bacterial efflux pumps that make TB resistant to rifampin. Studies show it improves rifampin’s effectiveness in lab settings. While not yet standard, some clinical trials are testing this combo to shorten TB treatment. Always check with your doctor before combining them.
What should I do if I’m on rifampin and need surgery?
Tell your anesthesiologist and surgeon you’re on rifampin. It can interfere with pain meds, sedatives, and blood thinners. You may need to adjust doses or delay surgery until two weeks after stopping rifampin. Never assume standard doses are safe.
Is there a safer alternative to rifampin for TB?
For drug-sensitive TB, no. Rifampin is the most effective first-line drug and the only one that shortens treatment to six months. Alternatives like rifabutin are less potent and still cause interactions, just fewer. For drug-resistant TB, other drugs are used-but they’re less effective and more toxic. Rifampin remains essential.
10 Comments
Mohammed Rizvi
January 27, 2026 at 19:20 PM
Rifampin is the ultimate biological middle finger to modern medicine. One pill and suddenly your entire pharmacy becomes a useless paperweight. It’s like your body turns into a drug-eating monster that only respects one thing: the TB bug.
And yet we still use it because it’s the only thing that works. We’re stuck between a rock and a hard place-save lives or risk everything else. The real tragedy? This isn’t new. We’ve known about these interactions for decades. Yet doctors still prescribe it like it’s a magic bullet without a manual.
Meanwhile, people die quietly because no one told them their antidepressant just became a sugar pill. This isn’t science. It’s Russian roulette with a prescription pad.
Allie Lehto
January 29, 2026 at 15:04 PM
Okay but like… if your body starts metabolizing everything faster because of a drug that’s supposed to kill bacteria… isn’t that just evolution on fast-forward? Like, we’re basically forcing the whole human system to adapt to survive the very thing meant to save us?
And then we get mad when people get pregnant or have strokes? Like… maybe we shouldn’t be using a drug that turns our liver into a drug shredder? Maybe we need to stop treating medicine like a vending machine and start treating it like a living system?
I mean… we’re not just treating TB, we’re treating the entire ecosystem inside us. And we’re doing it with a sledgehammer. 😔
Also, orange pee is a sign of divine intervention. God’s way of saying ‘hey, you’re on something wild.’
Dan Nichols
January 29, 2026 at 21:19 PM
Let’s be real nobody reads the fine print anymore. You take a pill because your doctor says so and assume it’s safe. That’s not healthcare that’s negligence wrapped in a white coat.
Rifampin’s interactions are documented in every pharmacology textbook since the 80s. If your doctor doesn’t warn you about warfarin or birth control you’re not getting care you’re getting lucky.
And omeprazole helping? That’s not a miracle that’s basic science. You block the pump the drug works better. Why isn’t this standard yet? Because profit > patients. Always.
Stop acting surprised. This was predictable. Always is.
Renia Pyles
January 31, 2026 at 02:39 AM
So let me get this straight-we’re telling women to switch to IUDs because a drug that’s supposed to save lives also makes birth control useless? And we’re not screaming about this in the media?
What if you’re poor and can’t afford an IUD? What if you live in a state that bans contraception? What if you’re a trans man on testosterone and now your TB treatment is actively endangering your hormone therapy?
This isn’t medical science. This is systemic cruelty disguised as a treatment protocol. And the fact that people are still dying from this because no one bothered to warn them? That’s murder by bureaucracy.
Rakesh Kakkad
January 31, 2026 at 12:14 PM
Dear colleagues, the pharmacokinetic profile of rifampin necessitates a paradigm shift in therapeutic management. The induction of cytochrome P450 3A4 is not merely an adverse effect but a systemic modulation of endogenous metabolic pathways.
As per WHO guidelines, concomitant use of hormonal contraceptives with rifampin is contraindicated due to a documented 67% reduction in serum estrogen concentration.
Furthermore, the persistence of enzyme induction for up to fourteen days post-cessation mandates a minimum four-week washout period prior to initiation of narrow-therapeutic-index agents.
It is imperative that primary care providers implement mandatory medication reconciliation protocols prior to rifampin initiation.
Thank you for your attention to this critical public health matter.
Nicholas Miter
January 31, 2026 at 19:07 PM
I’ve seen this play out in the clinic a dozen times. Someone comes in for TB, gets rifampin, then two weeks later shows up with a clot or a positive pregnancy test.
Most of them don’t even know they were on something that could interact. Doctors don’t always have time to explain. Pharmacies don’t always flag it.
But the real fix? Better communication. Not just between doc and patient, but between all the systems. A simple alert in the EHR could save lives.
And honestly? The omeprazole thing? That’s the kind of low-cost, high-impact idea we need more of. Why are we still waiting for trials when the science is already there?
Just… talk to your patients. Even if it’s just five minutes.
Suresh Kumar Govindan
February 2, 2026 at 17:30 PM
Western medicine’s arrogance is on full display here. We weaponize nature, then act shocked when nature fights back. The bacteria aren’t resistant-they’re smarter than our arrogance.
And now we want to add omeprazole? A drug invented to treat heartburn? This isn’t innovation. This is desperation dressed as science.
Global health systems are collapsing because we treat disease like a math problem. We ignore ecology. We ignore evolution. We ignore the fact that life adapts.
There is no fix. Only damage control.
George Rahn
February 4, 2026 at 01:12 AM
This is why America needs to stop importing foreign drugs and start making our own. Rifampin is a relic from the Cold War. We’re letting other countries dictate our medicine because we’re too lazy to innovate.
Why aren’t we developing a new TB drug that doesn’t turn your body into a chemical warzone? Because it’s cheaper to keep using this junk and hope no one dies.
And don’t get me started on the orange pee. That’s not science. That’s a warning sign from God that we’ve gone too far.
We need American-made antibiotics. Not this colonial-era garbage.
Ashley Karanja
February 4, 2026 at 05:34 AM
What’s fascinating to me is how this entire pharmacological cascade reveals the profound interconnectedness of biological systems-especially the gut-liver axis, the microbiome-immune crosstalk, and the epigenetic modulation of efflux pump expression under subtherapeutic drug pressure.
When rifampin activates PXR, it doesn’t just upregulate CYP3A4-it triggers a downstream transcriptional reprogramming of xenobiotic metabolism pathways, including UGTs, SULTs, and ABC transporters, which collectively create a systemic metabolic phenotype that’s essentially a pharmacological storm.
And the fact that *M. tuberculosis* responds with RpoB upregulation and efflux induction within 48 hours? That’s not just tolerance-it’s a coordinated bacterial stress response, likely mediated by sigma factor networks and quorum-sensing-like signaling in granulomas.
Which is why adjunctive omeprazole is so promising: it’s not just blocking pumps, it’s disrupting bacterial metabolic adaptation at the membrane level, potentially reversing the phenotypic resistance that makes six-month regimens necessary.
And if we can shorten treatment to three months? That’s not just a clinical win-it’s a global health equity breakthrough. Millions of people in LMICs spend months traveling to clinics, losing wages, facing stigma. Three months means fewer relapses, fewer transmissions, fewer deaths.
But we need policy change too. Not just clinical trials. We need integrated care pathways, pharmacist-led medication reviews, and patient education that’s culturally competent and trauma-informed.
This isn’t just about a drug. It’s about how we value human life in the face of systemic complexity.




Betty Bomber
January 26, 2026 at 16:16 PM
I had no idea rifampin could mess with birth control like that. My cousin got pregnant while on it and thought she was just stressed. Turns out she didn’t even know the drug could do that. Scary how common this is.
Also, the orange urine thing? Total nightmare if you’re not prepared. Thought I was bleeding internally my first week on it. Took me 3 days to google it and realize it was normal. Should be on the prescription label in bold.
And yeah, the liver thing? I had mine checked weekly. No symptoms, but enzymes were spiking. Doc paused treatment for a week. Saved my liver. Always get tested.
Also, why isn’t this more widely known? My pharmacist didn’t mention any of this. Just handed me the script like it was Advil.