Mood Stabilizer Interaction Checker
Check Medication Interactions
Enter your mood stabilizer and other medications to see potential risks.
Interaction Results
When you're managing bipolar disorder, finding the right mood stabilizer can feel like a breakthrough. But what happens when you need to take another medication - say, for high blood pressure, pain, or even a simple infection? Suddenly, your carefully balanced treatment can become risky. Lithium, valproate, and carbamazepine are three of the most commonly used mood stabilizers, but they don't play well with everything. Their interactions aren't just theoretical - they can land you in the hospital.
Why These Three Are Different
Lithium, valproate, and carbamazepine all help control mood swings, but they work in completely different ways. That’s why their interactions are so unpredictable. Lithium is cleared by your kidneys. Valproate is broken down in your liver using multiple pathways. Carbamazepine? It tricks your liver into speeding up its own metabolism - and it can force other drugs to disappear faster too.This matters because if you're on lithium and start taking ibuprofen, your lithium levels can jump 25-30% in just a few days. That’s enough to cause tremors, confusion, or even seizures. Valproate can make lamotrigine - another mood stabilizer - become twice as strong in your body. And carbamazepine? It can turn birth control pills useless and make antipsychotics like risperidone stop working.
Lithium: The Kidney-Sensitive Stabilizer
Lithium has one of the narrowest safety margins of any psychiatric medication. The difference between a helpful dose and a toxic one is tiny: 0.6 to 1.2 mmol/L. Even a small change in how your kidneys handle it can push you over the edge.NSAIDs like ibuprofen, naproxen, or celecoxib are the biggest culprits. They reduce blood flow to the kidneys, which means lithium doesn’t get flushed out as quickly. A 2021 survey by the International Bipolar Foundation found that 68% of lithium users needed a dose change when prescribed a common painkiller. One Reddit user described going from stable to confused and trembling after starting ibuprofen - his lithium level jumped from 0.8 to 1.3 in three days.
Diuretics (water pills) are another danger. Thiazide diuretics like hydrochlorothiazide can increase lithium levels by 25-40%. Even ACE inhibitors, used for blood pressure, can raise lithium by 25%. The fix? Check your lithium level five to seven days after starting any new medication. Keep your level at the lower end of safe range - 0.6 to 0.8 mmol/L - if you're on these drugs together.
Hydration matters too. Dehydration from sweating, illness, or not drinking enough water can spike lithium levels. That’s why doctors tell you to drink water, not coffee or alcohol, and avoid extreme heat. The simple rule: if you’re sick, sweating, or taking a new pill - check your lithium level.
Valproate: The Liver’s Double-Edged Sword
Valproate (also called valproic acid) is more complex. It binds tightly to proteins in your blood - but only up to a point. Above 100 mcg/mL, that binding breaks down, and free drug levels rise suddenly. That’s why monitoring levels is non-negotiable.Valproate doesn’t just sit still - it interferes with how other drugs are broken down. It can double or even triple lamotrigine levels. If you switch from carbamazepine to valproate, your lamotrigine dose might need to drop from 400 mg to 200 mg overnight. Many patients don’t realize this until they start feeling dizzy or developing a rash - signs of lamotrigine toxicity.
Valproate also gets pushed out of your system faster when you take carbamazepine. Carbamazepine turns on liver enzymes that break down valproate, cutting its levels by 30-50%. That means you might feel your mood slipping - not because your illness is worsening, but because your medication isn’t working anymore.
And then there’s the big one: pregnancy. Valproate carries a 10.7% risk of major birth defects - more than four times the normal rate. It can also lower a child’s IQ by 7-10 points by age six. Because of this, the FDA issued a boxed warning in 2013. In Australia and the U.S., doctors now avoid valproate in women of childbearing age unless there’s no other option.
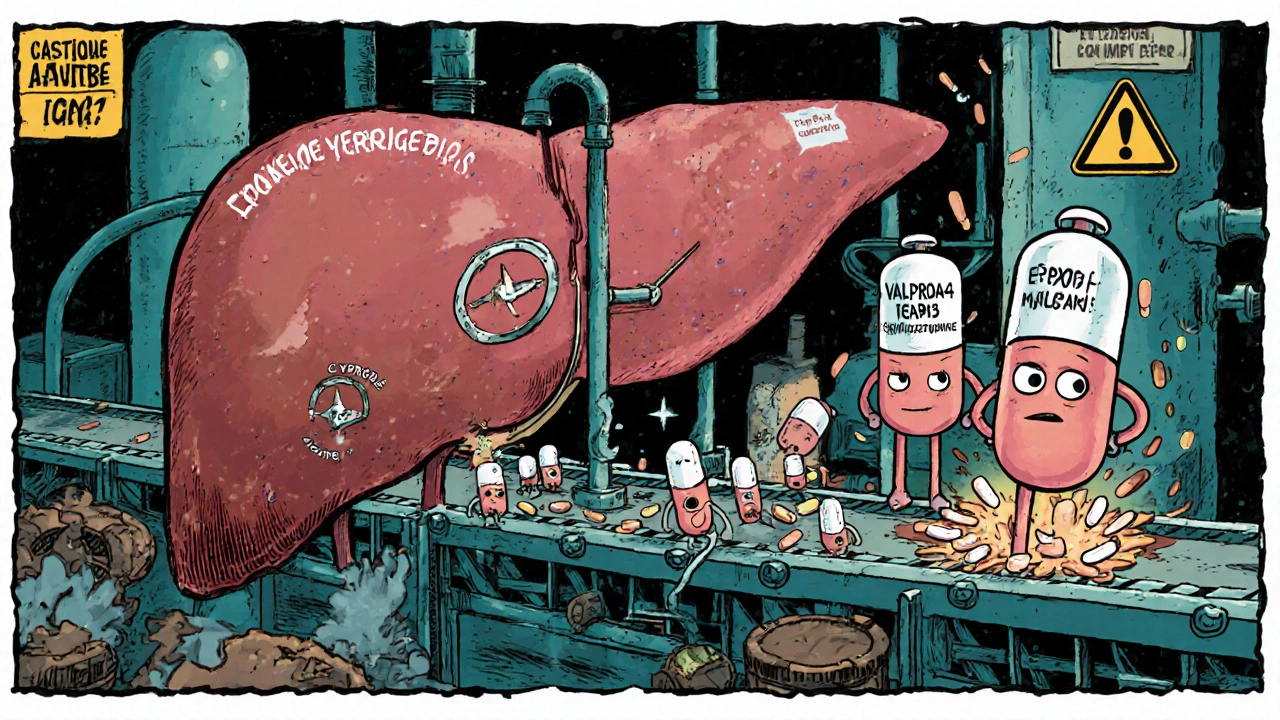
Carbamazepine: The Enzyme Activator
Carbamazepine is the most aggressive of the three. It doesn’t just interact - it actively changes how your liver works. It turns on CYP3A4, the main enzyme responsible for breaking down nearly half of all medications. That means drugs like risperidone, haloperidol, and oral contraceptives get metabolized too fast. You might stop getting relief from your antipsychotic, or accidentally get pregnant on birth control.But here’s the twist: when you add valproate to carbamazepine, things get even trickier. For years, doctors thought valproate just blocked one enzyme (epoxide hydrolase). New research shows it also blocks another - glucuronidation - meaning carbamazepine’s toxic byproduct, carbamazepine-epoxide (CBZ-E), builds up. CBZ-E causes dizziness, nausea, and loss of coordination. A 2019 survey of 853 psychiatrists found that 42% saw increased neurotoxicity in patients on this combo.
The fix? When starting valproate with carbamazepine, reduce the carbamazepine dose by 25%. Monitor both carbamazepine and CBZ-E levels. Keep CBZ-E under 3.5 mcg/mL. If you’re dizzy or unsteady, it’s not just fatigue - it could be a dangerous buildup of this metabolite.
Carbamazepine also has another quirk: it speeds up its own breakdown. In the first 3-5 weeks, your dose might feel too strong. Then suddenly, it stops working. That’s not tolerance - it’s autoinduction. Your liver adapts. Many patients stop taking it thinking it’s ineffective, when all they needed was a dose adjustment.
Real-Life Consequences
These aren’t abstract risks. They show up in ER visits, hospitalizations, and broken lives.A 2022 case study in the Journal of Affective Disorders followed a patient with 12 failed medication trials. Only when lithium and valproate were carefully combined - with levels monitored weekly - did they achieve stability for 18 months. But that only worked because the team checked levels constantly and avoided every known interaction.
On the flip side, a 2021 survey found that 22% of lithium users had experienced toxicity symptoms after starting a diuretic. Another patient reported her mood crashed after switching from carbamazepine to valproate - not because the new drug didn’t work, but because her lamotrigine level had doubled and she developed a severe skin reaction.
These stories aren’t rare. They’re predictable. And they’re preventable.
What You Need to Do
If you’re on one of these medications, here’s your action plan:- Always tell every doctor you see - even dentists or GPs - that you’re on a mood stabilizer. Many don’t ask.
- Never start a new OTC drug without checking. That includes ibuprofen, cold medicines with pseudoephedrine, or herbal supplements like St. John’s Wort.
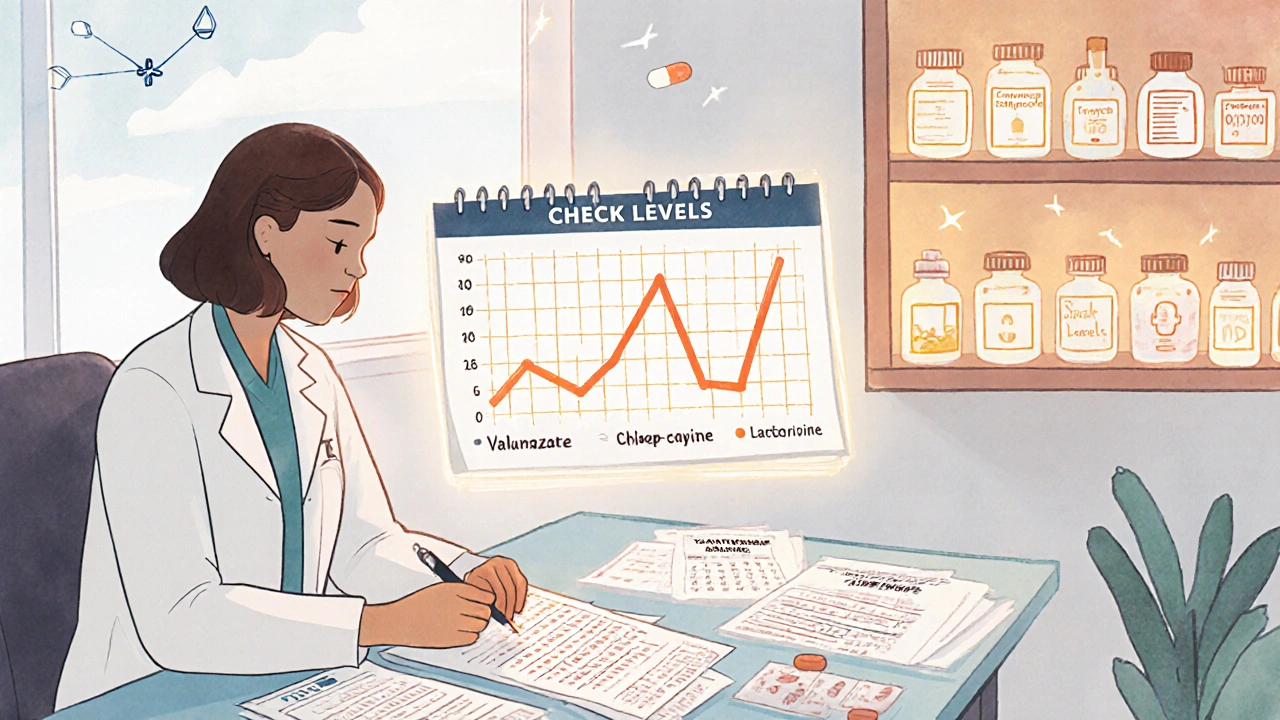
- Get regular blood tests. Lithium every 3-6 months. Valproate and carbamazepine every 3 months, or whenever your dose changes.
- Know the warning signs: for lithium - tremors, confusion, frequent urination. For valproate - nausea, drowsiness, swelling. For carbamazepine - dizziness, double vision, rash.
- Ask about alternatives. Lamotrigine, quetiapine, or lurasidone have fewer interactions. They might cost more, but they’re safer.
Medication changes aren’t emergencies - but they need planning. Don’t wait for symptoms to appear. Talk to your psychiatrist before you take anything new. Even if it seems harmless.
The Bigger Picture
Prescriptions for lithium have dropped from 35% of new starts in 2012 to just 15% today. Valproate has fallen too - from 55% to 40% - because of its risks in pregnancy. Carbamazepine holds steady at 10%. Meanwhile, lamotrigine has climbed to 35%. Why? Because it doesn’t play games with liver enzymes or kidney function. It’s simpler. Safer.But for many, these older drugs still work. The key isn’t avoiding them - it’s managing them with precision. That means knowing how they move through your body, what blocks them, what speeds them up, and what turns them toxic.
Technology is catching up. In 2023, researchers started testing for EPHX1 gene methylation - a possible reason why some people are more sensitive to carbamazepine. By 2027, genetic testing before starting carbamazepine could become standard. For lithium, the NIH is testing urine biomarkers to predict who’s at risk for interactions. These aren’t sci-fi - they’re coming.
Until then, the gold standard hasn’t changed: know your levels. Know your drugs. Know your body.
Can I take ibuprofen while on lithium?
No, not without medical supervision. Ibuprofen and other NSAIDs can increase lithium levels by 25-30%, raising your risk of toxicity. Symptoms include tremors, confusion, nausea, and muscle weakness. If you need pain relief, ask your doctor about acetaminophen (paracetamol) instead - it doesn’t affect lithium. Always check your lithium level 5-7 days after starting any new medication.
Does valproate interact with lamotrigine?
Yes, significantly. Valproate inhibits the enzyme that breaks down lamotrigine, causing its levels to increase by 100-200%. This raises your risk of a dangerous skin rash called Stevens-Johnson syndrome. If you’re adding valproate to lamotrigine, your dose of lamotrigine will likely need to be cut in half. Never adjust this yourself - your psychiatrist must guide the change slowly and monitor for rash.
Why does carbamazepine make birth control fail?
Carbamazepine activates liver enzymes (CYP3A4) that break down hormones in birth control pills, patches, and implants. This can reduce their effectiveness by 50-70%. If you’re on carbamazepine, use a non-hormonal method like an IUD or condoms. If you must use hormonal birth control, your doctor may need to increase the dose - but even then, it’s not fully reliable. Pregnancy while on carbamazepine also carries higher risks of birth defects.
Is it safe to combine lithium and valproate?
Yes, but only under close supervision. Unlike carbamazepine, valproate doesn’t interfere with lithium’s kidney clearance. In fact, this combination is often used for rapid-cycling bipolar disorder when single drugs fail. Levels of both drugs must be monitored regularly. Lithium should be kept at the lower end of the therapeutic range (0.6-0.8 mmol/L) to reduce risk. Studies show this combo can be effective for over a year without major issues - if monitored properly.
What should I do if I feel dizzy after starting valproate with carbamazepine?
Dizziness, unsteadiness, or nausea could mean your carbamazepine-epoxide (CBZ-E) level is too high. This toxic metabolite builds up when valproate blocks its breakdown. Don’t ignore it. Contact your doctor immediately. You’ll likely need a blood test to check both carbamazepine and CBZ-E levels. Your carbamazepine dose may need to be lowered by 25%. Never stop either drug suddenly - it can trigger seizures or mood episodes.
Are there safer alternatives to these three drugs?
Yes. Lamotrigine has far fewer drug interactions and is often preferred for bipolar depression. Quetiapine and lurasidone are antipsychotics approved for bipolar disorder with minimal interaction profiles. They’re more expensive than generics like lithium or carbamazepine, but they’re safer for long-term use, especially if you take multiple medications. Talk to your doctor about whether switching could reduce your risk.
Next Steps
If you’re on lithium, valproate, or carbamazepine, your next move is simple: make a list of every medication, supplement, and OTC product you take. Bring it to your next appointment. Ask: "Could any of these interact with my mood stabilizer?" Don’t assume your pharmacist or doctor knows - you’re the one living with this. Your safety depends on it.And if you’re starting a new medication - even something as small as a cold tablet - pause. Check. Ask. One interaction can undo months of stability. But with the right knowledge, you can stay safe, steady, and in control.
9 Comments
Timothy Sadleir
November 26, 2025 at 11:01 AM
It is imperative to recognize that the pharmacokinetic interplay between mood stabilizers and common analgesics constitutes a profound threat to neurohomeostasis. The renal clearance mechanism of lithium is exquisitely sensitive to prostaglandin inhibition, a phenomenon that, if unmonitored, precipitates iatrogenic encephalopathy. One must not treat psychiatric pharmacotherapy as a casual enterprise; it is a high-stakes calculus of molecular interactions.
The FDA's warnings, while adequate, remain insufficiently disseminated among primary care practitioners who prescribe NSAIDs without regard for psychiatric comorbidity. This is not negligence-it is systemic failure.
Furthermore, the rise in lamotrigine utilization reflects not therapeutic superiority, but a cultural retreat from the responsibility of monitoring. Lithium, despite its risks, remains the most empirically validated agent for long-term prophylaxis. To abandon it for convenience is to surrender to medical infantilism.
Carbamazepine’s autoinduction is not tolerance-it is the liver’s rebellion against pharmacological tyranny. Patients who discontinue it prematurely do so at peril, often triggering rebound mania or suicidal ideation. The burden of vigilance must be borne by the patient, the psychiatrist, and the pharmacist-in concert.
Genetic testing for EPHX1 methylation will not solve this crisis. It will merely delay the inevitable: a healthcare system that treats the body as a machine, not a living system. We must return to the art of medicine, not the algorithm.
And yet, we are told to “ask your doctor.” But who is the doctor? A 27-year-old resident with 12 minutes per patient? A pharmacist who has never seen a bipolar chart? The system is rigged. The pills are not the problem. The structure is.
I have watched three patients die from these interactions. Not because they were noncompliant. But because their providers were ignorant. And now, we are expected to be our own pharmacists. This is not empowerment. It is abandonment.
There is no safe medication. Only safe practices. And we have lost them.
Roscoe Howard
November 27, 2025 at 10:42 AM
It is a matter of national concern that American patients are being prescribed these medications without adequate oversight. In my country, we do not allow over-the-counter painkillers to be taken with mood stabilizers without a physician’s signature. This is not freedom-it is recklessness.
When a foreign doctor prescribes carbamazepine to a woman on birth control, and she becomes pregnant with a child at risk for neural tube defects, who bears responsibility? The patient? Or the system that failed to educate?
The decline in lithium use is a direct consequence of pharmaceutical marketing and the erosion of clinical judgment. We have traded proven efficacy for expensive alternatives because the bottom line matters more than the brain.
And let us not pretend that lamotrigine is some miracle drug. It causes rashes too. It just takes longer to kill you.
We need mandatory psychiatric-pharmacology training for all prescribers. Not optional modules. Not online videos. Real, accredited, in-person education. Or we will keep burying people who just wanted to feel better.
Patricia McElhinney
November 29, 2025 at 01:05 AM
Valproate and lamotrigine?? You think that's bad?? Try adding SSRI on top and then going on vacation to the desert. I had a full-body rash that looked like a third-degree burn. Took three months to heal. My doctor said 'it's rare'-like that helps when you're in the ER screaming.
And don't get me started on carbamazepine. I was on it for 8 months. Felt like I was walking through molasses. Then they added valproate and I couldn't stand up without holding onto walls. They never tested the epoxide. Never. I had to demand it. They acted like I was crazy for asking.
Doctors don't know this stuff. They read the pamphlet. That's it. You have to be your own advocate. Or die.
Agastya Shukla
November 29, 2025 at 22:30 PM
From a pharmacogenomics perspective, the CYP3A4 induction by carbamazepine is well-documented, yet the clinical implications remain underappreciated in resource-constrained settings. The emergence of CBZ-E as a neurotoxic metabolite-particularly in the context of valproate co-administration-demands therapeutic drug monitoring (TDM) protocols that are not universally accessible.
Furthermore, the protein-binding saturation kinetics of valproate above 100 mcg/mL represent a nonlinear pharmacokinetic phenomenon that complicates dose titration. Most clinicians rely on total serum concentrations, which may be misleading in hypoalbuminemic states or polypharmacy.
Interestingly, the 2023 EPHX1 methylation studies suggest epigenetic modulation may explain interindividual variability in carbamazepine metabolism, potentially enabling preemptive stratification. However, cost and infrastructure barriers limit scalability in low-income regions.
Lithium’s narrow therapeutic index necessitates not only frequent monitoring but also contextual awareness of hydration status, sodium intake, and diurnal variation in renal clearance. A 0.2 mmol/L fluctuation can shift a patient from euthymic to toxic.
While lamotrigine is favored for its interaction profile, its slow titration schedule and risk of SJS in genetically susceptible populations (e.g., HLA-B*15:02 carriers) demand pre-treatment screening, which is rarely performed outside tertiary centers.
Thus, the real challenge is not the drugs themselves, but the fragmentation of care. Psychiatry, neurology, and primary care operate in silos. Until we integrate pharmacovigilance into routine clinical workflows, these preventable toxicities will persist.
Pallab Dasgupta
December 1, 2025 at 10:15 AM
Bro. I was on lithium and took Advil for my back pain. Three days later I was in the hospital thinking my grandma was my therapist and that the TV was sending me messages. I didn’t even know I was on a mood stabilizer until the ER doc said ‘you’re lucky you’re alive.’
Now I only take Tylenol. And I text my psychiatrist every time I even think about taking something new. I don’t care if it’s a cough drop. I don’t care if it’s ‘natural.’ If it’s not on the approved list, it’s not getting in my body.
Also-carbamazepine and birth control? Yeah, I got pregnant on it. Twice. Both times I had to terminate. The doctors said ‘we didn’t think you’d be sexually active.’ What the actual f***. I’m not a robot. I’m a person.
If you’re on one of these meds, you’re not broken. You’re just playing Russian roulette with your brain. And the gun’s loaded.
But hey-you’re not alone. I’ve met people on Reddit who’ve been through the same thing. We’re the silent ones. The ones who don’t post about it because no one believes us until it happens to them.
So if you’re reading this? Please. Just check. Just ask. Just be paranoid. It’s better than being dead.
Ellen Sales
December 3, 2025 at 03:17 AM
I’ve been on valproate for 11 years. I’ve had two rashes. One was mild. One almost killed me. I learned the hard way that if your skin itches, stops peeling, or turns red like you’ve been boiled-you don’t wait. You call your doctor. You go to the ER. You don’t Google it.
And yes, I had to cut my lamotrigine in half when they added valproate. I cried. I was scared. But my psychiatrist sat with me for an hour. She didn’t just hand me a script. She explained it. She made me feel like I mattered.
That’s what this is really about. Not the drugs. Not the numbers. It’s about being seen. Being heard. Being treated like a human being, not a case file.
So if you’re reading this and you’re scared? I get it. I was too. But you’re not alone. And you’re stronger than you think. And your brain? It’s worth fighting for.
One pill at a time. One question at a time. One doctor who listens at a time.
You’ve got this.
Emily Craig
December 3, 2025 at 21:41 PM
Oh wow, so now I’m supposed to be my own pharmacist, nutritionist, and neurologist because doctors are too busy scrolling TikTok to read a drug interaction chart? How convenient.
And let’s not forget the $800/month lamotrigine that’s ‘safer’ but only if you can afford it. Meanwhile, my lithium costs $12. So thanks, capitalism, for making my brain a luxury item.
Also, carbamazepine made my birth control useless. I didn’t know. I thought it was just ‘stress.’ Then I got pregnant. I didn’t want it. I couldn’t afford it. And now I’m a single mom with a kid who might have developmental delays because some doctor didn’t think to ask if I was on meds.
So yeah. Keep telling us to ‘ask our doctors.’ Meanwhile, they’re on their 12th call of the day.
Karen Willie
December 4, 2025 at 15:19 PM
Thank you for writing this. I’ve been on lithium for 15 years. I’ve had two near-toxic episodes. Both times because I didn’t tell my dentist I was on it. He gave me a painkiller. I didn’t think it mattered.
Now I carry a card in my wallet. It says: ‘On Lithium. Avoid NSAIDs. Check levels.’ I show it to every provider. Even the physical therapist.
It’s not about being difficult. It’s about being alive.
If you’re reading this and you’re scared-me too. But we’re learning. We’re speaking up. We’re not giving up.
You’re not alone.





Jennifer Griffith
November 25, 2025 at 21:12 PM
lithium and ibuprofen? bad combo. i took both once for a headache and woke up feeling like my brain was melting. never again. just take tylenol. duh.