
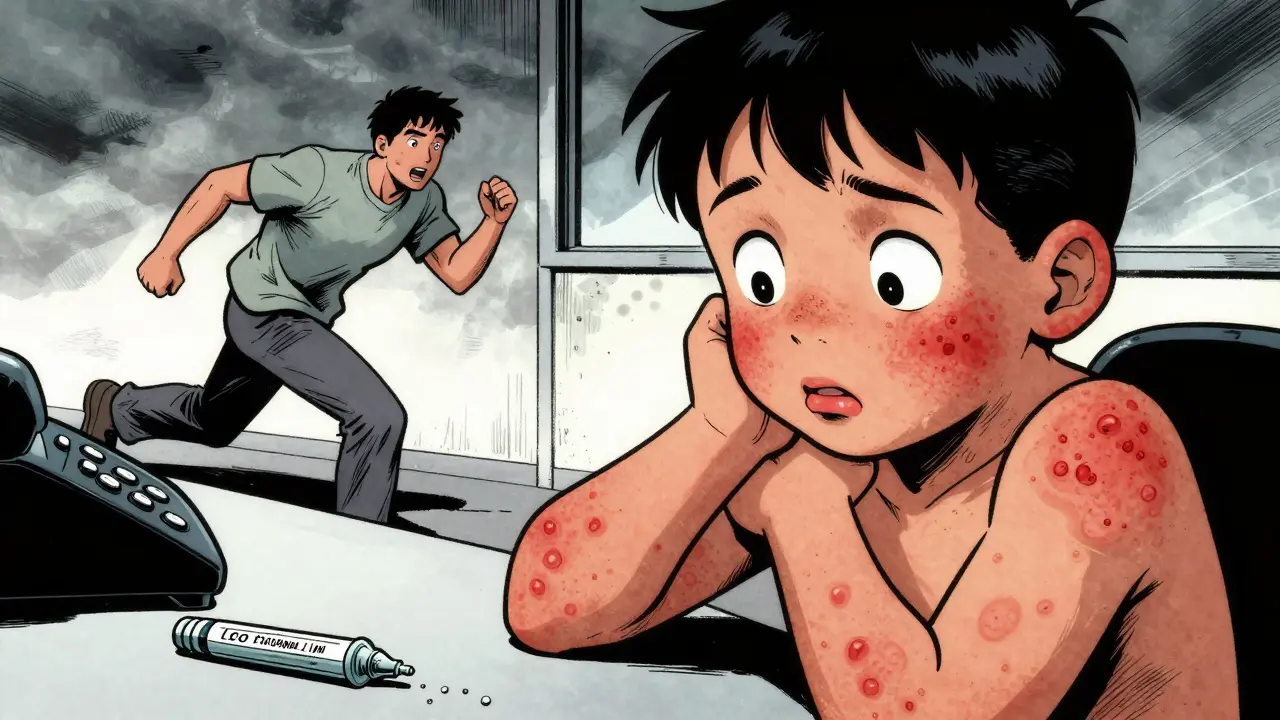
Most parents and even some adults panic when a rash shows up while taking an antibiotic. It’s common. It’s scary. And most of the time, it’s not an allergy. If you stop the antibiotic because of a rash, you might be making things worse-not better.
Not All Rashes Are Allergies
About 90% of kids labeled allergic to amoxicillin because of a rash aren’t actually allergic. That’s not a guess-it’s what testing shows. The rash you see? It’s often not your body rejecting the drug. It’s your immune system reacting to a virus you already have, like Epstein-Barr or a common cold, while the antibiotic is in your system. The two get mixed up. The rash appears around day 5 to 7, right when the virus is peaking and the antibiotic is at its highest level in your blood. That’s why it looks like the drug caused it-but it didn’t.This mistake has real consequences. People with a false penicillin allergy label end up on stronger, broader antibiotics. Those drugs cost more, cause more diarrhea, and increase your risk of life-threatening infections like C. difficile. In fact, patients with a mislabeled allergy are 63% more likely to get antibiotic-associated diarrhea and 30% more likely to catch C. diff. That’s not just inconvenient-it’s dangerous.
How to Tell the Difference
There are two main types of rashes you’ll see with antibiotics. One is harmless. The other needs emergency care.Non-allergic rash (most common): This looks like flat, pink or red spots-like tiny bruises-spread across the chest, back, or stomach. It doesn’t itch much, if at all. It doesn’t move around. It doesn’t swell. It just shows up, stays put, and fades on its own in 5 to 10 days. You’ll often see this in kids on amoxicillin, especially if they had a recent virus. No fever. No swollen lips. No trouble breathing. Just a rash.
True allergic rash (hives): This is different. Hives are raised, red, itchy welts that look like mosquito bites. They come and go-sometimes on your arm, then your leg, then your face. They show up fast: within minutes to an hour after taking the antibiotic. And they’re often paired with swelling of the lips, tongue, or throat. You might feel dizzy, nauseous, or have trouble breathing. This is anaphylaxis. It’s an emergency.
Then there’s the rare but deadly kind: Stevens-Johnson Syndrome (SJS) or toxic epidermal necrolysis (TEN). These involve blistering, peeling skin, and sores in your mouth, eyes, or genitals. You’ll have a high fever, feel extremely sick, and your skin might come off in sheets. This isn’t a rash you wait out. It’s a hospital-level emergency with a death rate as high as 50% in the worst cases.
What to Do When a Rash Appears
If it’s a non-itchy, flat rash with no fever or swelling: Keep taking the antibiotic. Don’t stop. The infection you’re treating is still there. Stopping it means the bacteria win. You’ll likely need a stronger, more expensive drug later-and you’ll risk spreading antibiotic resistance. Research shows that when parents stop antibiotics because of a non-allergic rash, their child is 37% more likely to have a treatment failure. That means a return visit, another round of meds, and more side effects.For comfort, you can use over-the-counter cetirizine (Zyrtec) or loratadine (Claritin) for itching. If it’s still bothering you, add famotidine (Pepcid) and apply 1% hydrocortisone cream to the worst spots. That’s it. No need for steroids or hospital visits. The rash will fade on its own.
If it’s hives, swelling, or trouble breathing: Stop the antibiotic immediately. Call 911 or go to the ER. If you have an epinephrine auto-injector (EpiPen), use it right away. Don’t wait. Anaphylaxis can kill in minutes. Even if it seems mild at first, it can get worse fast.
If you have fever over 38.5°C, blistering, or sores in your mouth or eyes: Stop the drug. Go to the hospital. This could be DRESS syndrome or SJS/TEN. These need specialist care-burn units, IV fluids, and monitoring. Don’t try to manage this at home.
Why So Many People Get It Wrong
Parents are told to watch for rashes. Doctors say, “If you see a rash, call us.” But no one explains what kind of rash. So people assume: rash = allergy = stop the medicine. That’s how 79% of parents mislabel their child’s reaction.On parenting forums, you’ll see hundreds of stories like this: “Stopped amoxicillin after day 3 because of rash. Infection came back worse. Had to switch to clindamycin. Diarrhea lasted two weeks.” That’s not an allergy story. That’s a treatment failure story.
Meanwhile, nurses and pediatricians who’ve seen dozens of cases say the same thing: “When parents keep going, the rash fades, the infection clears, and everyone’s fine.”
What Your Doctor Should Do
A good doctor won’t just say “allergy” and move on. They should ask: When did the rash start? What does it look like? Is there fever? Swelling? Trouble breathing? Did you have a virus before starting the antibiotic?If it’s a non-allergic rash, they should document it as: “Maculopapular rash on trunk, non-pruritic, day 7 of amoxicillin.” Not “penicillin allergy.” That label sticks forever-even if you never get tested. And it follows you into every hospital, every pharmacy, every emergency room.
There’s a simple test now called PENtest. It takes 15 minutes. It’s safe. It’s accurate. And if you’ve been told you’re allergic to penicillin because of a childhood rash, you’re probably not. Studies show 92% of people with a rash-only history pass the test. That means you could safely take penicillin again if you ever need it.

What You Can Do Now
If you or your child has had a rash on an antibiotic:- Don’t assume it’s an allergy.
- Don’t stop the drug unless you have hives, swelling, or trouble breathing.
- Take a photo of the rash. Note the date and symptoms.
- Call your doctor before stopping anything.
- If you’ve been labeled allergic because of a rash, ask about penicillin allergy testing.
Antibiotics save lives. But we’re wasting them-because we’re scared of rashes that aren’t dangerous. The real danger isn’t the rash. It’s the wrong choice you make because you don’t know the difference.
When in Doubt, Call the Doctor
You don’t need to be a doctor to know when to act. If you’re unsure, call. But don’t stop the antibiotic unless you’re certain it’s an allergic reaction. Most rashes aren’t. And stopping the drug when you shouldn’t is the real risk.Is a rash from antibiotics always an allergy?
No. In fact, most antibiotic rashes are not allergic. About 90% of rashes in children on amoxicillin are non-allergic, especially if they appear after day 5 and aren’t itchy or raised. They’re often caused by a virus, not the drug.
Should I stop amoxicillin if my child gets a rash?
Only if the rash is raised, itchy (hives), or accompanied by swelling, trouble breathing, or fever. If it’s flat, pink, non-itchy, and appears after day 5, keep giving the antibiotic. Stopping it increases the chance the infection returns worse.
Can I give my child antihistamines for an antibiotic rash?
Yes, for comfort. If the rash is itchy, cetirizine (Zyrtec) or loratadine (Claritin) can help. For more persistent itching, adding famotidine (Pepcid) and applying 1% hydrocortisone cream to the affected areas is safe and effective. But these won’t make the rash go away faster-they just reduce discomfort.
What’s the risk of continuing an antibiotic with a non-allergic rash?
There’s no added risk. Studies show that continuing the antibiotic when the rash is non-allergic leads to better outcomes: faster recovery, fewer repeat infections, and less need for stronger, riskier antibiotics. Stopping it unnecessarily increases treatment failure by 37%.
Can I get tested to see if I’m really allergic to penicillin?
Yes. A simple skin test or blood test called PENtest can be done in 15 minutes. It’s safe and accurate. If you were told you’re allergic because of a childhood rash, there’s a 92% chance you’re not. Getting tested removes a lifelong label that puts you at higher risk for dangerous infections and limits your treatment options.
What’s the difference between a rash and anaphylaxis?
A rash is just skin changes. Anaphylaxis involves multiple body systems: hives + swelling of the throat, trouble breathing, vomiting, dizziness, or a drop in blood pressure. If you have any of these symptoms together, it’s an emergency. Use an EpiPen if you have one and call 911 immediately.
10 Comments
Lorena Druetta
February 4, 2026 at 07:33 AM
Thank you for sharing this vital information. Many families are unnecessarily terrified by rashes that are, in fact, benign. Your clarity may save lives-and prevent unnecessary antibiotic resistance. I hope every parent reads this.
Keith Harris
February 5, 2026 at 17:47 PM
Oh please. This is Big Pharma’s way of keeping you hooked on their $400 antibiotics. They don’t want you to know the truth: most rashes are caused by toxins in the drugs, not viruses. And who’s funding these ‘PENtest’ studies? Hmm? 🤔
Daz Leonheart
February 7, 2026 at 10:15 AM
Just wanted to say: if you’re unsure, call your doc. Don’t guess. I’ve seen too many parents stop meds out of fear-and then the fever comes back harder. You’re not alone. Keep going, even if the rash looks weird. It’s usually fine.
Coy Huffman
February 8, 2026 at 00:53 AM
It’s wild how we’ve turned medical intuition into a fear-based checklist. We’re trained to see danger in every skin change, but biology doesn’t work that way. The body’s just… reacting. Not rebelling. Maybe we need to stop pathologizing normal immune responses. 🤔
Mandy Vodak-Marotta
February 9, 2026 at 22:43 PM
Okay but like-my sister’s kid got this exact rash on day 6, we kept giving the antibiotic, it faded by day 9, and the ear infection? Gone. Meanwhile, my cousin stopped the same drug because her friend on Facebook said ‘rash = allergy’ and now her kid had to go on clindamycin and got diarrhea for a MONTH. Like… why are we trusting random strangers over doctors? 🙄
Nathan King
February 11, 2026 at 13:39 PM
The empirical data presented here is both compelling and clinically significant. The conflation of maculopapular eruptions with IgE-mediated hypersensitivity represents a persistent diagnostic error in primary care, with measurable public health consequences. The PENtest, while underutilized, offers a parsimonious solution to this iatrogenic problem.
Sherman Lee
February 12, 2026 at 12:00 PM
lol i knew it. they’re hiding the truth. why do you think the rash always shows up on day 5? because that’s when the poison from the drug hits your liver. they don’t want you to know about the real cause. #AntibioticPoison #StopTheCoverUp 😈
Harriot Rockey
February 13, 2026 at 17:41 PM
My daughter had the same rash last year. We kept the antibiotic, used Zyrtec, and it faded. I wish I’d known this sooner-I cried for days thinking I’d hurt her. To every parent reading this: you’re not failing. You’re learning. And you’re not alone. 💙
Zachary French
February 15, 2026 at 03:45 AM
So let me get this straight… you’re telling me that 90% of parents are dumb enough to think a rash = allergy… and the doctors just let them walk out with a lifelong label? That’s not negligence, that’s a national fucking scandal. Someone’s getting paid to keep this myth alive. And guess what? It’s not the parents. It’s the system. 🤬






Kunal Kaushik
February 2, 2026 at 18:24 PM
Been there. Kid got rash on amoxicillin, we panicked, stopped it. Infection came back worse. Turned out it was just a virus. Lesson learned: don’t assume it’s the drug. 🤷♂️