Most people think shortness of breath is just part of getting older. Maybe you’ve noticed you can’t walk to the mailbox without stopping. Or you cough every morning and assume it’s from last night’s smoke or a lingering cold. But if you’re over 40 and have smoked - or lived around smoke - this could be more than aging. It could be COPD.
What COPD Really Is (And Why It’s Not Just a Bad Cough)
COPD stands for Chronic Obstructive Pulmonary Disease. It’s not one disease. It’s a group of lung conditions - mostly emphysema and chronic bronchitis - that slowly destroy your ability to breathe. The damage is permanent. But here’s the thing: it doesn’t have to get worse fast. If caught early, you can slow it down, sometimes even stop it. The key is understanding the stages. COPD doesn’t jump from mild to severe overnight. It creeps up. And most people don’t realize they’re in Stage 1 until it’s already Stage 2. That’s because symptoms start small. You think you’re just out of shape. You’re not. The gold standard for diagnosing and staging COPD is the GOLD system - developed by global lung experts and updated every year. It’s not just about how bad you feel. It’s about what your lungs can actually do. And that’s measured by a simple test called spirometry.Stage 1: Mild COPD - The Silent Start
If your FEV1 (the amount of air you can forcefully blow out in one second) is 80% or higher of what’s expected for someone your age, height, and sex, you’re in Stage 1. Sounds fine, right? But here’s what’s happening inside your lungs: the tiny air sacs are breaking down. The airways are thickening with mucus. Your body is trying to compensate. Symptoms? Maybe just a nagging cough in the morning. A little breathlessness when you climb stairs or walk fast. You might blame it on being out of shape. You might even think, “I’m not that old.” But 65% of people in Stage 1 report breathlessness only during hard activity - and they still don’t get tested. The good news? At this stage, quitting smoking can cut the rate of lung decline in half. Studies show smokers who quit reduce their FEV1 loss from 60 mL per year to just 30 mL. That’s huge. Pulmonary rehab isn’t always needed yet, but breathing exercises and light walking can make a real difference. Many never get diagnosed here. That’s the problem. By the time they feel it, it’s already worse.Stage 2: Moderate COPD - The Wake-Up Call
FEV1 drops to between 50% and 79%. This is where most people finally go to the doctor. You’re not just short of breath on hills anymore. You stop to catch your breath every few minutes on flat ground. You’re coughing more. Mucus is thicker. You’re tired all the time. About 83% of Stage 2 patients say they have to pause while walking on level ground. That’s not normal. That’s your lungs screaming for help. Treatment changes here. You’ll likely start on a long-acting inhaler - either a LABA or LAMA. These open your airways for 12 to 24 hours. In clinical trials, they improve FEV1 by 100-150 mL on average. That’s the difference between needing to rest after walking to the kitchen and being able to walk around your house without stopping. Pulmonary rehab becomes critical. It’s not just exercise. It’s education, breathing techniques, and emotional support. People who do it increase how far they can walk in six minutes by 45 to 75 meters. That’s the distance from your front door to your mailbox - and suddenly, you can make it without panic. Vaccines matter too. Flu shots cut exacerbation risk by 32%. Pneumonia shots? They’re not optional anymore. Here’s the twist: 38% of people classified as “high risk” in the GOLD Group D system - meaning they have lots of symptoms and frequent flare-ups - actually have only Stage 2 COPD based on their FEV1. Your symptoms don’t always match your number. That’s why doctors now look at both.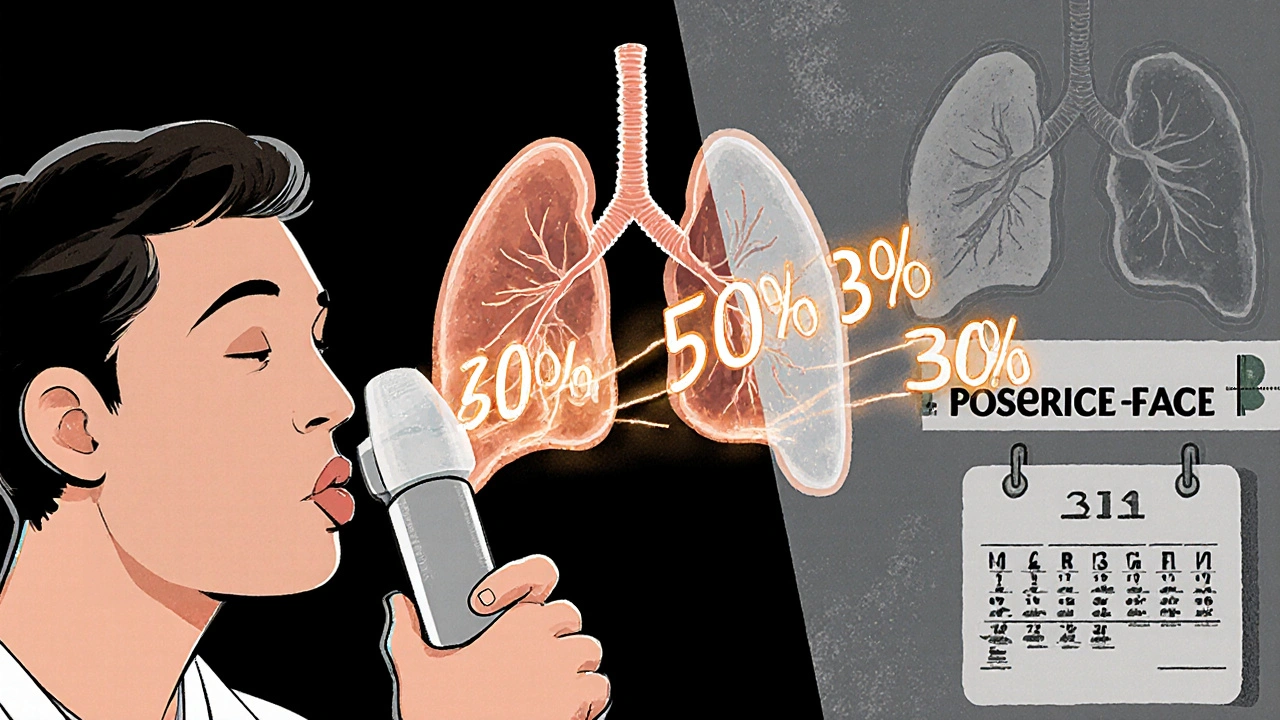
Stage 3: Severe COPD - Life Changes
FEV1 is now 30% to 49%. You’re not just tired. You’re struggling to do basic things. Buttoning a shirt. Taking a shower. Walking to the fridge. You might need to sit down to put on your socks. Ninety-two percent of Stage 3 patients report breathlessness during self-care tasks. Oxygen levels drop below 90% during normal activities. You’re not exaggerating. You’re surviving. Treatment gets more intense. You’ll likely be on a combo inhaler - LAMA plus LABA. That reduces flare-ups by 14% compared to one inhaler alone. If your blood test shows high eosinophils (over 300 cells/μL), you might add an inhaled steroid. It cuts flare-ups by 25%. You’ll be referred to a lung specialist. Annual 6-minute walk tests become standard. You might start using oxygen on and off during the day. Some people need it just to sleep. This is the stage where many patients feel isolated. One Reddit user wrote: “I can’t walk to my mailbox (20 feet) without stopping. My doctors say I’m ‘only’ Stage 3, so I must be exaggerating.” That’s the cruel gap between numbers and reality. Your FEV1 is 38%. That’s severe. Your struggle is real.Stage 4: Very Severe COPD - The Fight for Air
FEV1 is below 30%. Your lungs are working at less than a third of their original capacity. You’re on oxygen - 15 hours a day or more. You’re not just breathless. You’re fighting for every breath. Eighty-nine percent of Stage 4 patients need daily oxygen therapy. Without it, survival drops. The NOTT trial showed long-term oxygen use boosts one-year survival from 73% to 90%. That’s life-changing. Flare-ups become dangerous. Each one carries a 22% risk of death within the year. Hospitalizations are common. You might need non-invasive ventilation - a mask that helps you breathe while you sleep. Medications become more complex. You might be on multiple inhalers, oral steroids, or even antibiotics at the first sign of infection. Nutrition matters. Many lose weight because breathing burns so many calories. But here’s what no one tells you: quality of life isn’t just about oxygen levels. It’s about connection. 44% of Stage 4 patients say social isolation is their biggest struggle. You stop going out because you’re afraid of getting winded. You cancel plans. You feel like a burden. Financial stress is real too. Oxygen equipment costs $287 a month out-of-pocket - even with Medicare. That’s not just a bill. It’s a choice between medicine and groceries.Why Stage Matters More Than You Think
The biggest mistake? Waiting. Dr. Fernando J. Martinez says early treatment can slow progression by 50%. That’s not a guess. That’s from real data. If you’re in Stage 1 or 2 and get the right care, you might never reach Stage 3. But here’s the hard truth: only 12.3% of people over 40 with breathing problems get spirometry tested. Primary care doctors miss it 42% of the time because they don’t do the test right. They rely on symptoms alone. But symptoms lie. You need a spirometry test. Not a chest X-ray. Not a pulse oximeter. Not a guess. A real breathing test with a machine that measures how fast and how much air you can push out - after you use a bronchodilator. If you’ve smoked, even if you quit 20 years ago, and you’re over 40 - get tested. If you’re coughing every morning. If you get winded faster than your friends. If you’re tired all the time - get tested.What You Can Do Right Now
- If you smoke - quit today. No delay. No “next month.”
- Ask your doctor for a spirometry test. Say: “I’m over 40, I’ve smoked, and I’m having trouble breathing. I want a lung function test.”
- If you’re diagnosed, don’t wait. Start treatment now. Pulmonary rehab, inhalers, vaccines - they work.
- Track your symptoms. Keep a log: when you get breathless, what you were doing, how long it lasted.
- Join a support group. You’re not alone. People on Reddit, HealthUnlocked, and COPD Foundation forums share what works.
- Ask about oxygen therapy if you’re in Stage 3 or 4. It’s not a last resort. It’s a lifeline.
What’s Coming Next
Researchers are working on blood tests that can predict how fast COPD will worsen. One marker - fibrinogen - shows people with levels above 3.5 g/L lose lung function 2.3 times faster. That could mean earlier, smarter treatment. AI is helping too. At Massachusetts General Hospital, AI that reads spirometry results cuts misdiagnosis by 35%. That’s huge for people in small towns or rural areas where specialists are scarce. But none of this matters if you don’t get tested. The WHO warns that without better early detection, COPD deaths will rise 30% by 2030. Most of those deaths are preventable. Your lungs don’t ask for much. They just need you to listen. Before it’s too late.Can COPD be reversed?
No, COPD cannot be reversed. The damage to the lungs is permanent. But it can be slowed - sometimes stopped - with early treatment. Quitting smoking, using prescribed inhalers, doing pulmonary rehab, and avoiding triggers like smoke and pollution can prevent further decline. Many people in Stage 1 or 2 live for decades without progressing to severe stages if they act quickly.
Is COPD the same as asthma?
No. Asthma is usually reversible with medication and often starts in childhood. COPD is progressive, caused mostly by smoking or long-term exposure to lung irritants, and typically appears after age 40. Asthma symptoms come and go. COPD symptoms get worse over time. Some people have both - called asthma-COPD overlap syndrome - which requires a different treatment plan.
Do I need oxygen if I have COPD?
Not everyone with COPD needs oxygen. It’s usually prescribed for Stage 3 or 4, especially if your blood oxygen levels are low during activity or sleep. Long-term oxygen therapy (15+ hours a day) has been proven to extend life in severe cases. But if you’re in Stage 1 or 2, oxygen won’t help - and could even be harmful if used unnecessarily. Your doctor will test your oxygen levels before prescribing it.
Can I still exercise with COPD?
Yes - and you should. Exercise doesn’t hurt your lungs; it helps them work better. Walking, cycling, or even seated exercises improve muscle strength and breathing efficiency. Pulmonary rehab programs are designed for people with COPD. You’ll learn how to breathe while moving, pace yourself, and avoid panic. Many people say exercise gives them back their independence.
Why do I feel more breathless in cold weather?
Cold, dry air irritates your airways and causes them to tighten. This makes breathing harder, especially with COPD. Wind and humidity can also trigger symptoms. To manage it, cover your nose and mouth with a scarf when outside. Use a humidifier indoors. Avoid going out during extreme cold. Many people with COPD find they feel better indoors during winter months.
How often should I get my lungs checked?
If you’re diagnosed with COPD, you should have a spirometry test at least once a year. If you’re in Stage 3 or 4, you’ll also need a 6-minute walk test annually to track your functional ability. If you’re in Stage 1 or 2 and stable, your doctor may check every 1-2 years. But if your symptoms change - you’re coughing more, needing more inhaler puffs, or getting winded easier - get tested sooner. Don’t wait for your annual appointment.
What’s the biggest mistake people with COPD make?
Waiting. Waiting to quit smoking. Waiting to get tested. Waiting to start treatment. Waiting to ask for help. The disease doesn’t wait. Every year you delay, you lose more lung function. The best time to act was yesterday. The next best time is now.
12 Comments
Bartholemy Tuite
November 25, 2025 at 13:48 PM
Man I remember when my old man was in Stage 3 and he'd just sit there after showering like he'd run a marathon. Doctors kept saying 'you're not that bad' but he could barely button his shirt. Turns out they were measuring numbers not life. Pulmonary rehab saved him. Not meds. Not oxygen. Just learning how to breathe again with people who got it. I wish someone told me that sooner. Now I run a local group. If you're in Stage 2 or higher and not doing rehab you're leaving half your life on the table. It's not gym class it's survival training.
Also stop ignoring the cold air. Scarf over your nose. No joke. My dad used to laugh till he couldn't breathe then he tried it and suddenly he could walk to the store without stopping. Small shit. Big difference.
Sam Jepsen
November 26, 2025 at 18:14 PM
Just got diagnosed Stage 2 last month. Was convinced it was just 'getting old'. Nope. Spirometry test was a wake up call. Started rehab 2 weeks ago. Can now walk to the end of my driveway without gasping. That’s 30 feet. Used to be 10.
Also stopped smoking cold turkey. No patches. No vaping. Just said no. My lungs are screaming thank you.
If you’re reading this and you smoke? Do it. Today. Not tomorrow. Today.
Yvonne Franklin
November 28, 2025 at 10:56 AM
Stage 3 and oxygen only at night? That’s still manageable. Don’t let the numbers scare you. Focus on what you can do. Walk. Breathe. Eat. Connect.
And yes oxygen therapy isn’t a death sentence. It’s a tool. Like glasses for your lungs.
Rahul Kanakarajan
November 29, 2025 at 16:09 PM
Why are people still smoking at 50? You know what this is. You’ve read this exact post before. You’re just lazy. And now your kids are gonna pay for it.
Also why do you think COPD is 'just a smoker’s disease'? My neighbor never smoked. Worked in a sawmill 40 years. No one warned him. System failed him. And now he’s on 24/7 oxygen. This isn’t a personal failure. It’s a public health disaster.
Stop blaming the patient. Fix the system.
Melvina Zelee
November 29, 2025 at 22:14 PM
My grandma had COPD and she used to say 'I don't want to die, I just want to breathe without fighting for it'.
That hit me harder than any medical study.
She did rehab. She walked every day with her cane. She laughed till she cried. She didn't wait for perfect. She just showed up.
You don't need to be a hero. Just show up.
And if you smoke? Put it down. Not tomorrow. Right now.
Love you. You got this.
ann smith
November 30, 2025 at 07:21 AM
Just wanted to say thank you for this post. My husband was diagnosed Stage 2 last year. We thought it was just 'a cough'. Now he’s on LAMA, does rehab twice a week, and got his flu shot yesterday. We’re not fixed. But we’re fighting. And that’s enough for today. 💪❤️
Julie Pulvino
December 2, 2025 at 02:32 AM
My dad’s in Stage 4. He’s on oxygen 20 hours a day. Costs $300/month out of pocket. We’re choosing between his meds and groceries every month.
Why is this not a national emergency?
People talk about 'quality of life' like it’s a buzzword. But when you’re sitting there watching your dad struggle to sip water because his hands shake from the effort of breathing - quality of life isn’t a concept. It’s a daily battle.
We need better policy. Not just better inhalers.
Patrick Marsh
December 2, 2025 at 13:01 PM
Important: Spirometry must be done after bronchodilator. Not before. Many clinics skip this. Invalid results. Don’t accept it. Insist on the full protocol.
Also: FEV1/FVC ratio <0.7 confirms obstruction. If your doctor doesn’t mention this, ask for a second opinion.
Details matter.
David Cunningham
December 4, 2025 at 04:53 AM
Just got back from my 6-minute walk test. Did 420 meters. Last year it was 310. Pulmonary rehab is magic. Not a cure. But magic.
Also, I started walking my dog 10 minutes a day. That’s it. No fancy gear. Just boots and a leash.
My dog doesn’t care if I’m wheezing. He just wants to go. And now I do too.
Small steps. Big wins.
luke young
December 4, 2025 at 18:28 PM
My cousin in Australia got diagnosed at 48. He quit smoking, started rehab, and now he’s kayaking. Yeah. Kayaking. With oxygen tank strapped to the boat.
He says, 'I’m not waiting for the storm to pass. I’m learning to sail in it.'
That’s the spirit.
Don’t let COPD write your story. You still hold the pen.
Justin Daniel
December 6, 2025 at 01:30 AM
So… you’re telling me that if I smoked for 20 years and quit yesterday, my lungs might still have 80% function? And that’s called ‘Stage 1’? Wow. So the real villain isn’t the smoke. It’s the system that lets you ignore it for 20 years. And then acts shocked when you’re diagnosed.
Also… why is this post so well-researched? Who wrote this? I need to follow them.
Also also… I’m gonna go get tested. Right after this comment.
Thanks.






Neoma Geoghegan
November 23, 2025 at 23:01 PM
Stage 1 and you're already wheezing after the mailbox? Quit smoking today. No excuses. Your lungs don't care about your 'next month'.
FEV1 is your new BFF. Get tested. Now.