Medication Timing Converter
Understanding Medication Timings
This tool converts common medication timing instructions into the Universal Medication Schedule (UMS) system, making it easier to understand when to take your medications. UMS uses clear labels like morning, noon, evening, and bedtime instead of confusing abbreviations.
Universal Medication Schedule (UMS)
Select an option above to see your medication timing converted to UMS.
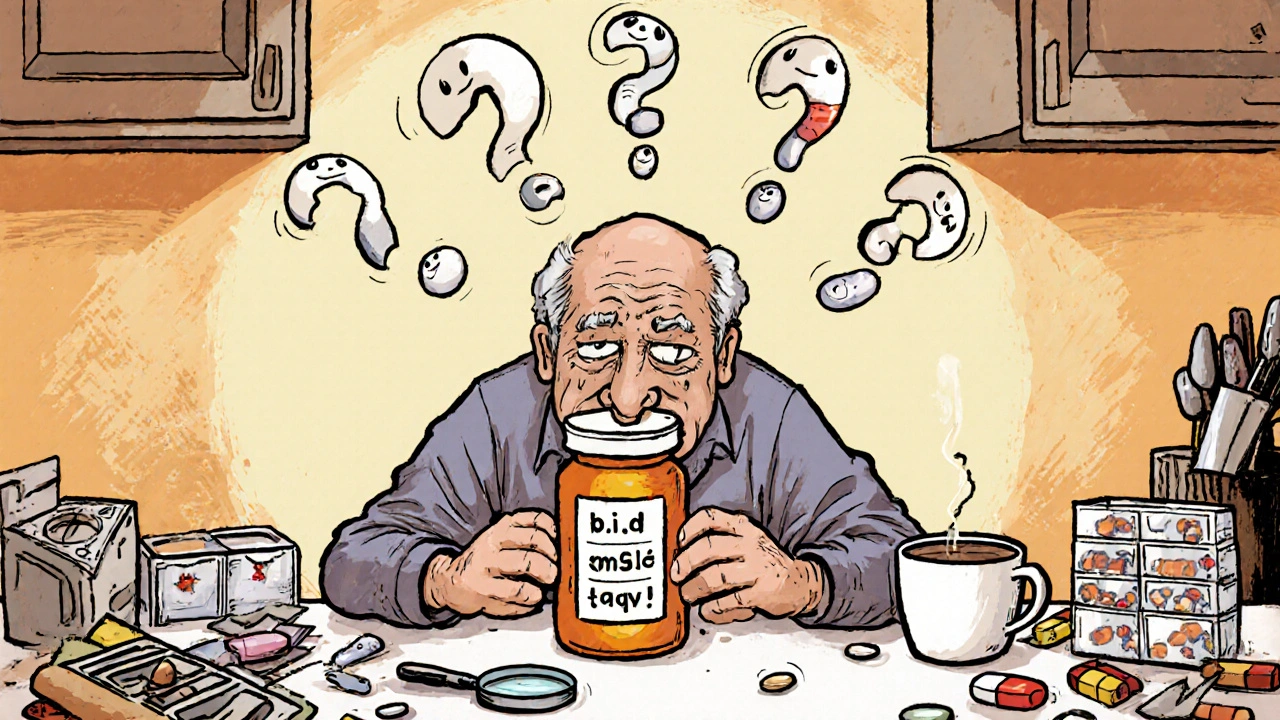
Every year, over 1.3 million people in the U.S. suffer medication errors because they didn’t understand their prescription label. It’s not because they’re careless. It’s because the labels are written in a language most people can’t easily read or understand. You might think you know what "take twice daily" means. But do you know if that means 8 a.m. and 8 p.m.? Or 12 hours apart? What if you’re on five different pills? What if you’re tired, stressed, or just not a native English speaker? This isn’t rare. It’s happening in homes, nursing homes, and emergency rooms every single day.
Why Medication Labels Are So Confusing
Most prescription labels still use medical jargon like "q.d.", "b.i.d.", or "take on an empty stomach." Even when they’re written out in plain English, they’re often too long, too vague, or too complex. A 2009 study found that 47% of patients misunderstood standard instructions like "Take 1 tablet by mouth twice daily." That’s nearly half of all people reading their own medicine labels. The problem gets worse for older adults, people with low literacy, or those managing multiple conditions. One patient told researchers she thought "take every 4-6 hours" meant she could take 4 to 6 pills at once. Another confused "mg" with "ml" and ended up overdosing on liquid medicine.What Health Literacy Actually Means
Health literacy isn’t about how many degrees you have. It’s about whether you can understand, use, and act on health information. The U.S. Department of Education found that only 12% of adults have proficient health literacy. That means 88% struggle with basic health tasks - like reading a pill bottle. The Institute of Medicine calls this a public health crisis. And it’s not just about reading. It’s about math. It’s about memory. It’s about knowing when to ask for help. A parent might misread "5 mL twice daily" as "5 mL total," not realizing they’re supposed to give 5 mL each time. A senior might mix up morning and evening pills because the label doesn’t say "morning" and "evening" - it says "b.i.d."The Universal Medication Schedule (UMS)
One of the most effective fixes is the Universal Medication Schedule, or UMS. Instead of saying "twice daily," labels now say: morning, noon, evening, bedtime. That’s it. No Latin. No abbreviations. Just four clear times tied to daily routines. A 2022 study in Wisconsin showed that when health systems switched to UMS, dosing confusion dropped by 47% among elderly patients on multiple medications. One 72-year-old patient said, "I finally understood when to take my pills after they switched to morning/noon/evening/bedtime labels." Simple. Human. Effective.Pictograms Save Lives
Words aren’t enough. Pictures help. A 2023 study from the U.S. Pharmacopeia found that labels with simple pictograms - like a sun for morning, a moon for bedtime, or a glass of water next to a pill - improved correct interpretation by 28% among people with low health literacy. One common pictogram shows a hand holding a pill next to a clock with 8 and 8 - meaning take at 8 a.m. and 8 p.m. Another shows a stomach with a line through it, meaning "take on an empty stomach." These aren’t decorations. They’re safety tools. The FDA is moving toward requiring standardized pictograms on all prescription labels by 2024. Why? Because a patient once drank albuterol from a plastic bottle thinking it was a syringe. That’s not a mistake. That’s a system failure.How to Read Your Own Labels
You don’t have to wait for the system to fix itself. Here’s how to protect yourself right now:- Check the active ingredient. If you’re taking two different pills, make sure they don’t contain the same drug - like acetaminophen. Taking too much can damage your liver.
- Ask for the time. If it says "take twice daily," ask: "What times?" Write it down. Use your phone alarm.
- Measure carefully. Use the dosing cup or syringe that came with the medicine. Never use a kitchen spoon. A teaspoon is not 5 mL - it’s often closer to 4 mL. That adds up fast.
- Know the difference between "every 12 hours" and "twice daily." "Every 12 hours" means exactly 12 hours apart - even if you’re awake at 3 a.m. "Twice daily" usually means with meals - morning and evening.
- Ask the pharmacist to explain. Don’t be shy. Pharmacists are trained to help. Say: "Can you show me how to take this?"
The Teach-Back Method
One of the most powerful tools in healthcare is called the teach-back method. After a doctor or pharmacist explains your medication, they ask you: "Can you tell me in your own words how you’ll take this?" This isn’t a test. It’s a safety net. If you say, "I take one when I feel sick," but the medicine is meant for daily use, they catch it right then. UW Health found that using teach-back reduced misunderstandings by 33%. It takes just 1-2 minutes. And it works. If your provider doesn’t use it, ask for it. You have the right to understand your care.What’s Changing in 2025
The rules are finally catching up. The U.S. Pharmacopeia’s General Chapter <17> became official in May 2023, and full compliance is required by May 2025. That means every prescription label must be written at a fifth-grade reading level, use clear fonts, avoid abbreviations, and include pictograms. The FDA is also pushing drug makers to test labels with real patients - not just doctors - before they hit the market. Hospitals that fail to improve medication safety could lose up to 2% of their Medicare payments. That’s not a fine. That’s real money. And it’s forcing change.
Why This Matters for Families
Parents are especially vulnerable. A 2012 study of 200 top-selling children’s medicines found that 63% used confusing charts or tables to show dosing by weight or age. One parent said: "I thought the chart meant I should give 10 mL if my child weighed 40 pounds - but it was actually 10 mL for 40 to 50 pounds." That’s not your fault. That’s bad design. The 2023 JAMA trial at Children’s Hospital of Philadelphia showed that using a simple, visual discharge bundle - with pictograms, plain language, and teach-back - cut pediatric dosing errors by 34%. That’s hundreds of kids avoided from being rushed to the ER because their mom gave them the wrong dose.What You Can Do Today
You don’t need to wait for a system overhaul. Start now:- Keep a list of all your medications - including vitamins and OTC drugs - and update it every time something changes.
- Use a pill organizer with morning, noon, evening, and bedtime compartments.
- Take a photo of your pill bottle and the instructions with your phone. Save it in a folder called "Medications."
- Ask your pharmacist to print out a simplified version of your label in plain English.
- If you’re helping someone else - a parent, a child - sit down with them and go over each pill. Use the teach-back method: "Can you show me how you’ll take this?"
Medication safety isn’t about being perfect. It’s about being aware. It’s about asking questions. It’s about not assuming you understand. And it’s about demanding better - from your doctor, your pharmacist, your pharmacy, and your government.
What does "take twice daily" really mean?
"Take twice daily" usually means two times a day, spaced roughly 12 hours apart - like 8 a.m. and 8 p.m. But it doesn’t always mean that. Some doctors mean "with meals" - so breakfast and dinner. Always ask: "What times should I take it?" Write it down. Don’t guess.
Can I use a kitchen spoon to measure liquid medicine?
No. A kitchen teaspoon holds about 4 mL, but most doses are 5 mL. That small difference adds up. Always use the dosing cup, syringe, or dropper that came with the medicine. If you lost it, ask your pharmacy for a new one - they’ll give it to you free.
Why do some labels say "take on an empty stomach" and others say "take with food"?
Some medicines work better or cause fewer side effects depending on whether your stomach is full or empty. "Empty stomach" usually means 1 hour before or 2 hours after eating. "With food" means during or right after a meal. If you’re unsure, ask your pharmacist. Taking a pill the wrong way can make it less effective or cause nausea.
What should I do if I miss a dose?
Don’t double up unless your provider says to. If you miss a dose and it’s close to the next one (within 2-3 hours), skip it. If it’s been longer, take it as soon as you remember. Always check the label or call your pharmacist. Taking too much can be dangerous - especially with painkillers like acetaminophen or blood pressure pills.
Are there tools to help me understand my labels better?
Yes. Many pharmacies now offer simplified labels with pictograms and plain language. Ask for them. You can also use free apps like Medisafe or MyTherapy that send reminders and explain your meds in simple terms. Some hospitals offer free health literacy workshops. Check with your local clinic or library.
What Comes Next
The good news? Change is happening. More pharmacies are switching to UMS. More hospitals are using teach-back. More labels are adding pictures. But progress isn’t automatic. It needs people like you to ask for better. To speak up when something doesn’t make sense. To teach others. To keep asking: "Can you explain that again?" Because when it comes to your health - or your child’s - understanding isn’t optional. It’s the difference between healing and harm.12 Comments
Amber O'Sullivan
November 7, 2025 at 01:30 AM
Why is this even a problem in 2025 The labels are literally designed to confuse people
Jim Oliver
November 7, 2025 at 14:19 PM
Of course people don’t understand labels-most can’t even read a thermostat. This isn’t a design flaw, it’s a human flaw.
William Priest
November 8, 2025 at 16:58 PM
lol at the "fifth grade reading level" requirement. So now we dumb down meds because half the country thinks "b.i.d." means "buy it daily"?
Alyssa Salazar
November 10, 2025 at 16:46 PM
As a clinical pharmacist, I’ve seen this first hand. The term "q.d." still shows up on 30% of scripts I review. And yes, patients DO think it means "quit daily". We need mandatory plain language training for prescribers-not just labels. Also, pictograms should be standardized globally. Why does the US use a sun for morning while Europe uses a rising arrow? Confusing. We’re literally risking lives over typography.
Brierly Davis
November 11, 2025 at 17:49 PM
YES!! I use a pill organizer with AM/NOON/PM/BED and it changed my life. Also, I take a pic of every new script and save it in a folder called "My Meds". So simple, so helpful. 😊
Ryan Masuga
November 12, 2025 at 13:40 PM
My mom’s got 7 meds and she’s 78. She used to mix up the times until we switched to UMS labels. Now she says she feels like she’s finally in control. I wish every pharmacy did this automatically. No one should have to be a detective just to stay alive.
Jennifer Bedrosian
November 12, 2025 at 17:53 PM
I cried reading this. My cousin died because she took too much Tylenol thinking "take as needed" meant "take whenever it hurts". She was 29. This isn’t just about labels-it’s about how we treat people who are scared, tired, or just trying to survive
Lashonda Rene
November 14, 2025 at 15:51 PM
you know what i think is the real issue is that no one ever sits down with you and actually explains it like you’re a person not a chart or a number. i had a friend who was on warfarin and the pharmacist just handed her a bottle with a tiny print sheet and said "take one every day". she didn’t know what it did or why or what to watch for. she almost had a stroke because she didn’t know to avoid kale. it’s not that people are dumb it’s that the system treats them like they are. if you just took 5 minutes to say hey this is what this does and here’s what to look out for it changes everything. i’ve seen it. it’s not magic. it’s just kindness and time
Rashmi Mohapatra
November 15, 2025 at 21:34 PM
why are we even talking about this its basic common sense if you cant read a label dont take the medicine
Abigail Chrisma
November 17, 2025 at 19:48 PM
As a mom of two kids with chronic conditions, I’ve learned to ask for simplified labels, pictograms, and teach-back every single time. My daughter’s school nurse now uses the same system we do. It’s not just about safety-it’s about dignity. People deserve to understand their own bodies. And if you’re a provider who doesn’t do this? You’re not just lazy-you’re dangerous.
Andy Slack
November 19, 2025 at 18:33 PM
Change is coming. I work at a community clinic. We started using UMS + pictograms last year. ER visits for med errors dropped 40%. We’re not waiting for the FDA to catch up-we’re fixing it now. If your pharmacy doesn’t offer this? Ask for it. Demand it. Your life depends on it.




Beth Banham
November 5, 2025 at 21:26 PM
So many people just swallow pills without thinking. I saw my grandma mix up her blood pressure meds and end up in the ER. Simple labels could’ve saved her.