
Emergency Medication List Generator
Your Emergency Medication Checklist
This tool will help you create a complete emergency medication list to ensure medical professionals have the information they need in an emergency.
Your Emergency Medication List
Your list contains 0 items
Medications:
[No medications added]
Allergies:
[No allergies added]
Emergency Contacts:
[No contacts added]
This is a placeholder. Add your information above.
Remember: Keep this list updated every time you change a medication or start a new supplement. If you don't update it, it becomes less useful in an emergency.
When you’re in an emergency and can’t speak, your medication list could save your life. Paramedics don’t have time to guess what you’re taking. They need clear, accurate info fast. A simple paper card in your wallet or a digital profile on your phone can cut emergency response time by 15 to 20 minutes. That’s not just helpful-it’s life-saving.
Why Your Medication List Matters
More than two in five American adults take two or more prescription drugs. Add in over-the-counter painkillers, vitamins, and herbal supplements, and the risk of dangerous interactions skyrockets. In the U.S., medication errors cause about 7,000 deaths each year. Many of these happen because doctors and paramedics don’t know what you’re taking. A 2020 study found that patients who brought an updated medication list to the hospital had 37% fewer medication mistakes during admission. That’s not a small number. That’s the difference between a smooth recovery and a second hospital stay.
It’s not just about prescriptions. Things like ibuprofen, fish oil, or St. John’s wort can interact with blood thinners, heart meds, or even antibiotics. One nurse shared a case where a patient’s wallet card listed warfarin 5mg daily. Without it, the ER team almost gave an antibiotic that would’ve caused a fatal bleed. That card? It was handwritten on a 3x5 index card. No app. No fancy tech. Just clear, updated info.
What to Include on Your Emergency Card
Your list doesn’t need to be fancy. It just needs to be complete. Here’s what every emergency medication card should have:
- Full name of each medication - both brand and generic. If you take Lisinopril, write that. But also write “Zestril” if that’s what the bottle says.
- Dosage - 5mg, 10mg, 500mg. Don’t say “one pill.” Say exactly how much.
- How often - “once daily,” “every 6 hours,” “as needed for pain.”
- Why you take it - “for high blood pressure,” “for arthritis,” “for sleep.” This helps providers understand your health history fast.
- Allergies and reactions - Not just “penicillin allergy.” Say “rash and swelling after penicillin,” or “anaphylaxis after sulfa drugs.” Be specific.
- Vitamins, supplements, and herbs - Even if you think they’re “natural,” they can interfere with meds. Ginkgo biloba? Garlic pills? Turmeric? Write them all.
- Emergency contacts - Name, relationship, phone number. At least two people who can answer questions about your care.
- Blood type (if known) - Some templates include this. It’s not required, but it helps in trauma situations.
For older adults or those with chronic conditions, add: your diagnosis (like “Type 2 diabetes,” “heart failure”), code status (Do Not Resuscitate? Yes or No?), and any discontinued meds (e.g., “Stopped simvastatin in 2023 due to muscle pain”).
Paper vs. Digital: Which One Works Better?
You have two main options: paper or digital. Both have pros and cons.
| Feature | Paper Card | Digital (Phone) |
|---|---|---|
| Accessibility | Works anytime, no battery needed | Accessible from lock screen on iPhone (Medical ID) and Android |
| Updates | Easy to rewrite with pencil | Update in app - but only if phone is charged and working |
| Portability | Fits in wallet, purse, or pocket | Always with you - if you carry your phone |
| Visibility | Only if someone finds it | Paramedics can access it even if phone is locked |
| Accuracy | Can become outdated if not updated | Can become outdated if not updated |
| Success rate in emergencies | 78% access rate when present | 32% access rate when phone is present |
Here’s the catch: 92% of adults own a smartphone. But only 18% of emergency patients have a paper card on them. So while paper is easier to access if you have it, most people don’t carry it. Digital is more likely to be there - but only if you set it up right.

How to Build Your Card - Step by Step
Creating your list doesn’t take long. Here’s how to do it right:
- Gather everything - Pull out all your pill bottles, supplement containers, and OTC boxes. Include creams, inhalers, patches. Don’t forget the ones you stopped taking.
- Write down each one - Use the template above. Don’t skip anything. If you’re unsure about a supplement, look up the generic name.
- Review with your pharmacist - Go to your pharmacy. Ask them to check for duplicates, interactions, or outdated meds. Most will do this for free. This step alone catches 45% of errors older adults make on their own.
- Choose your format - Print the FDA’s “My Medicines” template (free online) or use Apple Health’s Medical ID or Android’s Emergency Information feature.
- Update it religiously - Every time you get a new prescription, stop a med, or start a new supplement, update the list. Set a reminder on your phone: “Update meds - every 30 days.”
- Share it - Give a copy to your primary doctor, a family member, and your emergency contact. Keep one in your wallet. Keep one on your phone.
Where to Get Templates
You don’t need to design this from scratch. Use trusted sources:
- U.S. FDA - “My Medicines” template - Free, simple, clinically reviewed. Available at fda.gov/my-medicines.
- CDC - “My Medications List” - Designed for older adults and includes space for traditional remedies.
- Apple Health App - Go to Health → Medical ID → Edit. Add all meds, allergies, emergency contacts. Turn on “Show When Locked.”
- Android - Open Phone app → Emergency → Medical info → Add info. Works even if phone is locked.
- CVS Pharmacy - Offers a printable wallet card generator on their website.
Avoid Etsy templates unless they’re based on FDA or CDC standards. Many are pretty but missing critical fields like dosage or reason for use.
Common Mistakes (And How to Avoid Them)
People make the same mistakes over and over:
- Not updating - 67% of people forget to update their list. Solution: Link updates to your next doctor visit. If you see your doctor every 3 months, update the card the day after.
- Using vague terms - Saying “I take my blood pressure pill” instead of “Lisinopril 10mg daily.” Be specific.
- Leaving out supplements - “It’s just a vitamin.” No. Vitamin E can thin your blood. Ginkgo can cause bleeding. List them all.
- Keeping it in the wrong place - Don’t put it in your purse if you rarely carry it. Keep it in your wallet. Or use your phone.
- Assuming someone else knows - Your daughter might think she remembers your meds. She doesn’t. Write it down.
Dr. David Mendelson from JAMA says it best: “An outdated list is worse than no list.” If you haven’t updated it in 6 months, throw it away and start fresh.
What Happens in an Emergency?
Imagine you collapse in a grocery store. Paramedics arrive. They check your wallet. They find a card. It says:
- Warfarin 5mg daily - for atrial fibrillation
- Metformin 500mg twice daily - for diabetes
- Aspirin 81mg daily - for heart
- Allergy: Penicillin - rash and swelling
- Emergency contact: John Smith, 555-123-4567
They don’t need to call your family. They don’t need to wait for records. They know not to give you penicillin. They know to check your INR before giving fluids. They know you’re on blood thinners. They can treat you safely in minutes.
Without that card? They guess. They delay. They risk giving you something that kills you.
Final Thought: It’s Not About Technology. It’s About Responsibility.
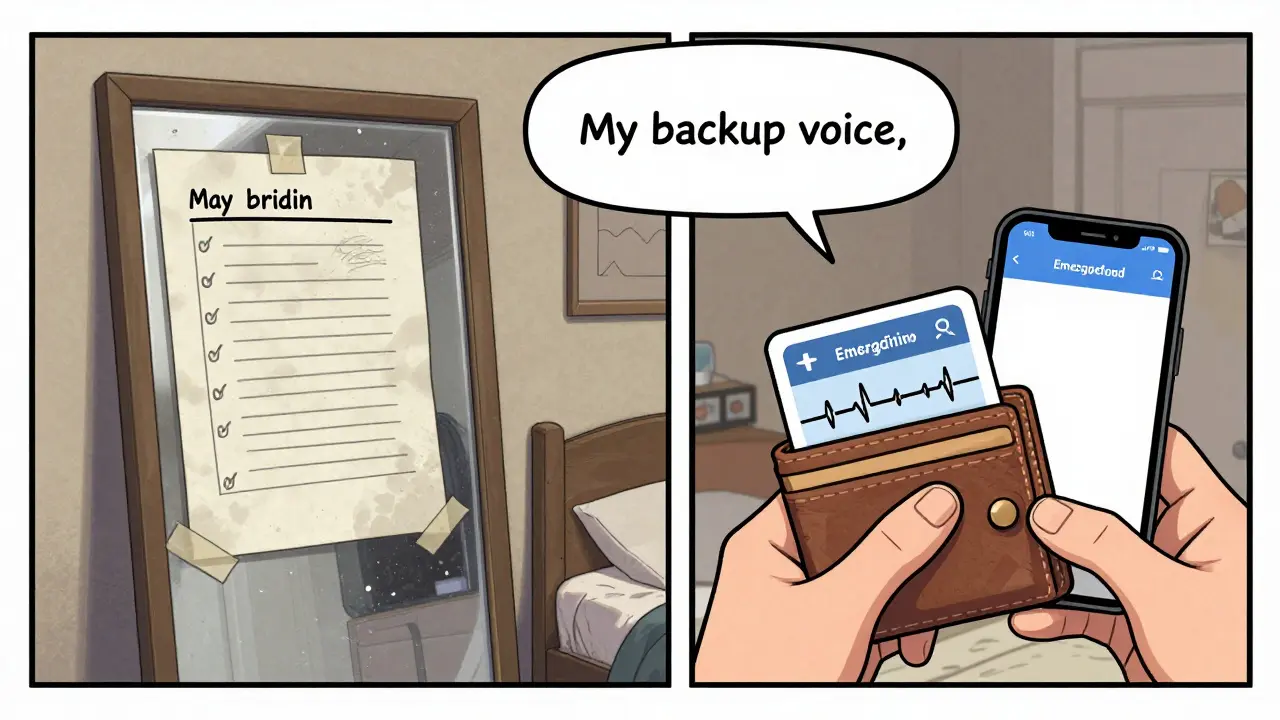
You don’t need a fancy app. You don’t need to be tech-savvy. You just need to write it down. Update it. Carry it. Share it.
This isn’t a suggestion. It’s a safety habit - like wearing a seatbelt or checking smoke detectors. If you take more than one medication, you’re at risk. Your list isn’t optional. It’s your backup voice.
What if I don’t know the generic name of my medication?
Check the bottle - it’s usually printed right under the brand name. If you’re unsure, take the bottle to your pharmacy. Pharmacists can tell you the generic name and confirm the dosage. You can also use free apps like Drugs.com or Medscape to look up the brand name and find the generic version.
Should I include over-the-counter meds and supplements?
Yes. Even if you think they’re harmless, they’re not. Common OTCs like ibuprofen, naproxen, or cold medicines can interfere with blood pressure drugs, blood thinners, or kidney function. Supplements like fish oil, ginkgo, or garlic pills can increase bleeding risk. Always list them.
How often should I update my medication list?
Update it every time you start, stop, or change a medication. That includes new prescriptions, OTC drugs, vitamins, or supplements. Set a monthly reminder on your phone: “Update meds.” Also, review it with your pharmacist or doctor at every visit - even if you think nothing changed.
Can I use a digital app instead of paper?
Yes - if you use your phone’s built-in Medical ID (iPhone) or Emergency Information (Android). These are designed for first responders to access even if the phone is locked. Third-party apps are less reliable because first responders can’t access them without unlocking your phone. Stick with Apple Health or Android’s system.
What if I don’t carry my phone or wallet?
Keep a copy in your car, purse, or next to your bed. Some people tape a small card inside their wallet or attach it to their keychain. Others use a medical alert bracelet that says “See wallet card for meds.” The goal is to have at least two places where someone can find it - and always carry one.
Don’t wait for an emergency to realize you didn’t prepare. Take 20 minutes today. Gather your meds. Write them down. Update it. Carry it. Your life depends on it.





