
When Autoimmune Disease Makes Everyday Tasks Hard
Imagine trying to open a jar, tie your shoes, or carry groceries - and your body says no. Not because you’re lazy, but because your immune system is attacking your own tissues. That’s the reality for millions living with autoimmune diseases like rheumatoid arthritis, lupus, Sjögren’s, or fibromyalgia. Functional impairment isn’t just about pain. It’s about losing the ability to do the things that make life feel normal. And it’s not something you just have to accept.
Rehabilitation and occupational therapy aren’t optional extras. They’re essential tools to keep you moving, working, and living independently. Studies show structured rehab programs can improve daily function by 35-42% in people with autoimmune conditions, especially when started early. That’s not a small win. That’s going from needing help to dress yourself to doing it on your own again.
Why Traditional Exercise Often Fails
Many people with autoimmune diseases try to push through fatigue and pain, thinking more activity equals better health. But that’s a trap. Pushing too hard during a flare can trigger a crash - sometimes lasting days or weeks. One Reddit user shared: “My therapist told me to ‘just keep going’ during a flare. I ended up bedridden for three weeks.” That’s not motivation. That’s harm.
The problem? Most fitness advice is designed for healthy people or those with simple joint wear-and-tear. Autoimmune disease is different. Your body isn’t just tired - it’s inflamed. Muscles weaken from disuse, nerves get hypersensitive, and your energy reserves drain faster than a phone on 5G. What works for a runner won’t work for someone with lupus.
Therapy isn’t about lifting heavier weights. It’s about dosing movement like medicine. Physical therapists now use specific guidelines: during flares, start with gentle isometric exercises at just 20-30% of your max effort. No jumping. No running. No pushing into pain. Just enough to keep muscles alive without fueling inflammation.
How Physical Therapy Helps You Move Again
Physical therapy (PT) focuses on restoring mobility, strength, and endurance. But it’s not one-size-fits-all. For someone with rheumatoid arthritis, PT might mean improving knee flexion so you can stand up from a chair without grabbing the armrests. For someone with scleroderma, it could be hand stretches to keep fingers from curling into fists.
Studies show PT improves lower-body function by 28% more than occupational therapy alone, measured by how quickly someone can stand up, walk three meters, and sit back down (the Timed Up and Go test). That’s the difference between needing help to get out of bed and doing it yourself.
Hydrotherapy is one of the most effective tools. Water at 92-96°F reduces joint stress while providing gentle resistance. People report 22% more pain relief in water than on land. But here’s the catch: only 32% of rural clinics have access to therapeutic pools. That’s why home-based programs are growing fast - especially since the pandemic.
Therapists also use tools like TENS units (delivering 50-100Hz pulses) to calm nerve pain, and goniometers to measure joint range precisely. Progress isn’t measured in pounds lifted, but in how many steps you can take before needing to rest - or whether you can brush your teeth without holding onto the sink.
Occupational Therapy: Reclaiming Your Daily Life
If PT helps you move, occupational therapy (OT) helps you live. OT doesn’t care if you can squat. It cares if you can pour coffee, button your shirt, or type an email without your hands going numb.
OT wins by 33% over PT when it comes to upper-body function and daily tasks, according to the Arthritis Hand Function Test. That’s because OT doesn’t just train your muscles - it rethinks your environment.
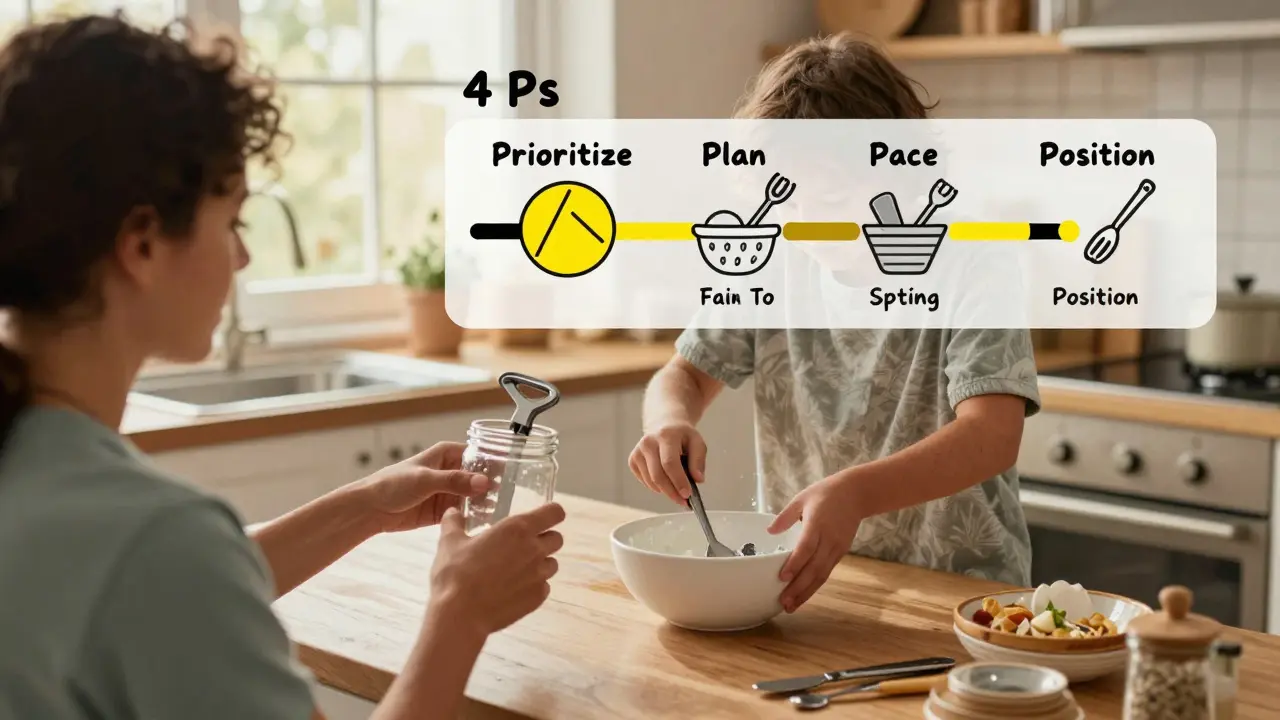
Therapists teach the 4 Ps: Prioritize, Plan, Pace, Position. That means:
- Prioritize: Do the most important tasks first - like taking meds - before fatigue hits.
- Plan: Break big tasks into small steps. Washing dishes? Do five, rest five minutes, then do five more.
- Pace: Never work longer than 15-20 minutes without a 5-10 minute break. This isn’t laziness. It’s science.
- Position: Use ergonomic tools - jar openers, reachers, keyboard stands - to reduce strain.
One patient, after six months of OT, reduced her HAQ-DI score from 2.1 to 0.8 - enough to return to part-time work. She didn’t get stronger. She got smarter about how she used her energy.
OT also introduces adaptive tech: voice-activated lights, smart thermostats, automated door openers. These aren’t luxuries. For someone with limited hand mobility, they’re lifelines. One study found these tools improved independence by 31%.
What Works - and What Doesn’t
Not all rehab programs are created equal. The biggest mistake? Ignoring disease flares.
When disease activity is high (measured by DAS28 scores over 5.1), aggressive therapy often backfires. Patients report crashes - days of exhaustion, increased pain, even worse inflammation. Rehab works best when disease is stable. That’s why therapists use tools like the Canadian Occupational Performance Measure (COPM) to track real-life progress, not just lab numbers.
Another pitfall: therapists who don’t understand central fatigue. This isn’t just muscle tiredness. It’s brain fog, overwhelming exhaustion, and a feeling that your body has no gas left - even if your joints feel okay. Dr. Alan Peterson warned in JAMA Internal Medicine that 19% of rehab programs miss this entirely, making symptoms worse.
Then there’s the insurance problem. Most plans cover only 12-15 sessions a year. But experts recommend 24-30 to see real change. That’s why many patients turn to telehealth. Since 2020, 68% now use home-based programs - up from just 22% before.
And let’s talk about intensity. The 70% rule is key: never push past 70% of your perceived maximum effort. If you feel like you’re giving 100%, you’re already overdoing it. Heart rate variability monitors are now being used to help patients find their personal threshold - no guesswork.

Who Should Do This - And How to Find the Right Therapist
This isn’t something you do with a general physical therapist. You need someone trained in autoimmune conditions. Look for therapists with certifications like the Academy of Pelvic Health Physical Therapy’s Autoimmune Specialty Certification - a 120-hour program that covers 87 different autoimmune diseases.
Ask questions before starting:
- Do you have experience with my specific condition?
- How do you adjust sessions during flares?
- Do you use the COPM or HAQ-DI to track progress?
- Will you teach me pacing - not pushing through pain?
Red flag: A therapist who says “no pain, no gain.” That’s dangerous here. You need someone who says, “Rest is part of the plan.”
Specialized centers like the Cleveland Clinic’s Autoimmune Rehabilitation Program treat over 1,200 patients a year. But you don’t need to travel there. Many telehealth providers now offer certified autoimmune rehab - and insurance is slowly catching up. Medicare’s 2024 reimbursement increase of 5.7% for chronic condition care is a sign things are moving in the right direction.
The Future: Smarter, Personalized Care
Rehab is getting smarter. The NIH launched the Autoimmune Rehabilitation Registry in January 2023, tracking outcomes for over 5,000 patients across 47 clinics. New research shows adjusting exercise intensity based on weekly blood markers like IL-6 improves outcomes by 39%.
Next up? AI-powered apps. The Lupus Foundation’s “PacePartner” - currently in Phase 3 trials - uses wearable sensors to predict flares with 82% accuracy. It doesn’t just tell you to rest. It tells you when to rest, based on your unique body signals.
The goal isn’t to cure autoimmune disease. It’s to help you live well despite it. And with the right rehab, that’s not just possible - it’s happening every day.
What You Can Do Today
- Track your energy levels for a week. Note when you feel best and worst.
- Start using the 4 Ps: Prioritize, Plan, Pace, Position - even in small tasks.
- Try 10 minutes of gentle movement daily - even if it’s just seated arm circles or ankle rolls.
- Ask your doctor for a referral to an occupational or physical therapist trained in autoimmune conditions.
- Don’t wait for a flare to pass. Start rehab during remission - it’s your best window for improvement.
Functional impairment doesn’t have to be your permanent story. With the right support, you can rebuild your independence - one small, smart step at a time.
15 Comments
Faith Edwards
January 12, 2026 at 20:29 PM
One is compelled to observe, with a degree of bemusement, that the modern rehabilitation paradigm has been so thoroughly colonized by the aesthetics of productivity culture-where even rest is weaponized into a metric-driven performance. One wonders whether the very notion of 'independence' has been co-opted by neoliberal imperatives, reducing the human experience of chronic illness to a series of KPIs measurable by goniometers and HAQ-DI scores. The soul is not a spreadsheet.
Jay Amparo
January 14, 2026 at 12:05 PM
I come from a small village in India where PT is a luxury, but my sister with lupus started doing water exercises in the village pond-warmed by the sun, no pool needed. We tied ropes to chairs for support, used bamboo sticks to reach things. She can now feed herself again. You don’t need fancy gear. You need someone who listens. The 4 Ps? We called it ‘smart living.’ Same thing, different language.
Lisa Cozad
January 15, 2026 at 18:11 PM
My OT taught me to use a weighted pen and a voice-to-text app. I went from typing 3 sentences before my hands locked up to writing 500 words a day. It wasn’t about strength-it was about redesigning the world around me. I didn’t fix my body. I fixed my environment. And now I’m back to editing manuscripts part-time. Small wins, huge impact.
Saumya Roy Chaudhuri
January 17, 2026 at 01:21 AM
Let me tell you something you won’t hear from these ‘experts’-most of these so-called therapies are just glorified yoga with a fancy label. I’ve seen patients spend $20,000 on ‘specialized’ rehab while ignoring the real issue: their diet, their stress levels, their sleep hygiene. No one talks about the gut-immune axis. No one. Just more gadgets and goniometers. The truth? Rest, clean food, and calm nerves do more than any TENS unit ever could.
Ian Cheung
January 17, 2026 at 02:13 AM
70% rule changed my life. I used to think if I wasn’t sweating I wasn’t doing anything. Then I tried moving at 70%-just 70%-and I didn’t crash for weeks. My heart rate monitor showed I was staying in the sweet spot. I started walking 10 minutes after breakfast. No more all-or-nothing. Just steady. Quiet. Sustainable. My body finally trusts me again
anthony martinez
January 18, 2026 at 12:33 PM
Oh great. Another article telling us to ‘listen to our bodies’ while charging $200/hour for a therapist who doesn’t even take insurance. Real helpful. Meanwhile, I’m on a 6-month waitlist for a PT who doesn’t say ‘just keep going.’ Thanks for the pep talk, doc. Can you also tell my landlord to lower the rent?
Mario Bros
January 19, 2026 at 08:21 AM
My PT told me to do 5 minutes of ankle rolls every morning. I thought it was stupid. Now I can walk to the mailbox without my knees screaming. It’s not magic. It’s consistency. And yeah, I still have bad days. But now I know when to stop. You don’t need to be a warrior. Just be a student of your own body. 💪
Jake Nunez
January 20, 2026 at 07:05 AM
In my community, we don’t have fancy rehab centers. But we have neighbors who bring soup, help with laundry, and sit quietly when you’re too tired to talk. Sometimes the best therapy isn’t a TENS unit-it’s someone who shows up and says, ‘I see you.’ That’s the real lifeline.
Christine Milne
January 21, 2026 at 19:36 PM
These so-called ‘specialized’ programs are a Western capitalist fraud. In countries with universal healthcare, patients receive holistic care without being marketed adaptive devices or telehealth subscriptions. This article glorifies consumerism disguised as medicine. The real solution? Abolish the profit motive in healthcare. Not another goniometer. Not another app. Justice.
Bradford Beardall
January 23, 2026 at 11:14 AM
Has anyone here tried combining hydrotherapy with mindfulness breathing? I started doing slow exhales while floating in the pool-4 seconds in, 6 seconds out. It cut my pain spikes by half. Not sure if it’s the water or the breath, but it’s the first time in years I’ve felt like my body and mind are on the same team.
McCarthy Halverson
January 23, 2026 at 20:38 PM
Use a reacher. Use a jar opener. Do 10 minutes. Rest. Repeat. That’s it. No magic. Just consistency.
Michael Marchio
January 25, 2026 at 07:13 AM
Let’s be real-most of these rehab programs are designed by people who’ve never spent a day with chronic pain. They talk about pacing like it’s a productivity hack, not a survival strategy. And don’t get me started on the insurance loophole that limits you to 12 sessions. You can’t retrain a nervous system in 12 visits. You need years. But no one wants to pay for that. So we’re left with bandaids and guilt trips. And the worst part? The therapists know it. They just can’t say it out loud.
Jake Kelly
January 25, 2026 at 20:38 PM
I used to feel guilty for resting. Now I see it as part of the treatment. Like taking insulin. You don’t shame someone for needing it. You honor it. Same here.
Ashlee Montgomery
January 26, 2026 at 18:07 PM
What if the goal isn’t to return to who we were before illness, but to become who we are now-slower, quieter, more intentional? Maybe independence isn’t about doing everything alone. Maybe it’s about choosing what matters, and letting go of the rest. The body doesn’t lie. It just asks us to listen differently.






Ted Conerly
January 11, 2026 at 00:02 AM
For years I thought pushing through pain was strength. Then I got diagnosed with RA and my PT finally said, 'Rest isn't failure, it's strategy.' That changed everything. I started doing seated arm circles while watching TV, used jar openers, and broke dishes into two-minute chunks. Now I cook dinner most nights without collapsing. It's not about how much you do-it's about how smart you do it.