By January 2026, there are still over 270 generic drugs in short supply across the United States. That’s not a number you hear often, but it’s one that every pharmacist, nurse, and patient feels. These aren’t rare specialty meds-they’re the everyday drugs that keep people alive: antibiotics like vancomycin, chemotherapy agents like cisplatin, IV fluids like saline, and even basic painkillers. When these drugs disappear from shelves, it’s not just an inconvenience. It’s a safety crisis.
Why Do Generic Drugs Keep Running Out?
Most people think drug shortages happen because of bad luck-like a factory fire or a hurricane. But the truth is deeper. The system is built to fail. Generic drugs make up 90% of all prescriptions filled in the U.S., yet they account for more than 70% of all shortages. Why? Because they’re cheap to make and even cheaper to sell.
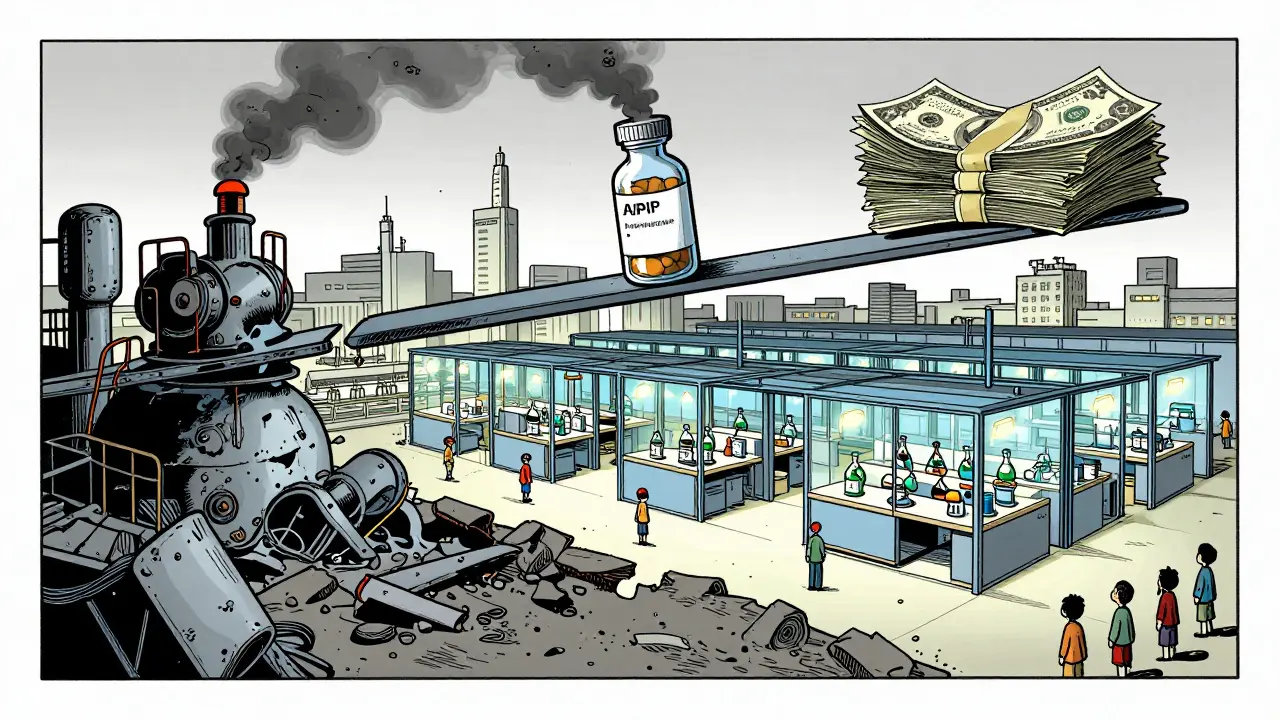
Manufacturers earn as little as 5-10% profit on generic injectables, compared to 30-40% on brand-name drugs. When margins are this thin, companies don’t invest in backup equipment, extra staff, or quality controls. They run their lines at full speed, with no room for error. One machine breakdown. One failed quality test. One delayed shipment of active ingredients from India or China-and the whole supply collapses.
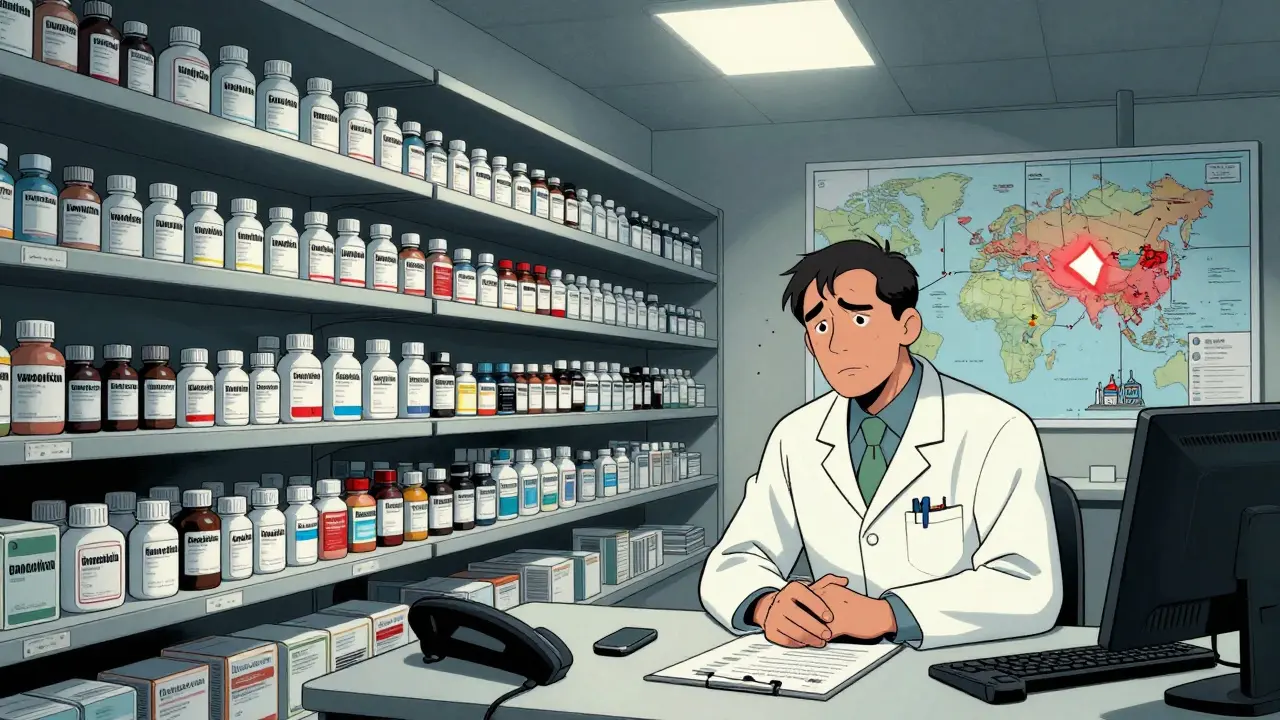
And here’s the kicker: about 70% of these critical generics have only one or two manufacturers approved by the FDA. That means if one plant shuts down, there’s no one else to pick up the slack. Even worse, over 80% of the raw ingredients (APIs) for these drugs come from just two countries: China and India. A regulatory inspection delay, a political dispute, or even a local power outage can ripple across the globe and leave U.S. hospitals empty-handed.
Who Gets Hurt the Most?
It’s not just hospitals. It’s the 67% of cancer centers that have had to change chemotherapy regimens because cisplatin wasn’t available. It’s the ER doctors who now see more patients with uncontrolled pain because opioids are out of stock. It’s the elderly patient who can’t get their blood pressure pill and ends up in the hospital.
Pharmacists spend 15-20 hours a week just trying to find alternatives. That’s not time spent counseling patients or checking for interactions. That’s time spent calling distributors, checking inventory across states, and convincing insurers to cover more expensive substitutes. Independent pharmacies report spending an average of 12.3 hours per week just managing shortages. Forty-three percent of patients walk away from their prescriptions because they can’t get them-or can’t afford the replacement.
And the replacements aren’t always better. Sometimes they’re less effective. Sometimes they cause more side effects. Sometimes they cost three times as much. One study found that when a generic drug goes missing, the price of the substitute can jump by 300%. That’s not a market response-it’s a patient penalty.
Why Are Generic Drugs More Vulnerable Than Brand-Name Drugs?
Brand-name drugs may have shortages too, but they’re different. They’re often protected by patents, so there’s less competition. Companies can charge more, invest in quality, and keep extra inventory on hand. If one batch fails, they can afford to make another.
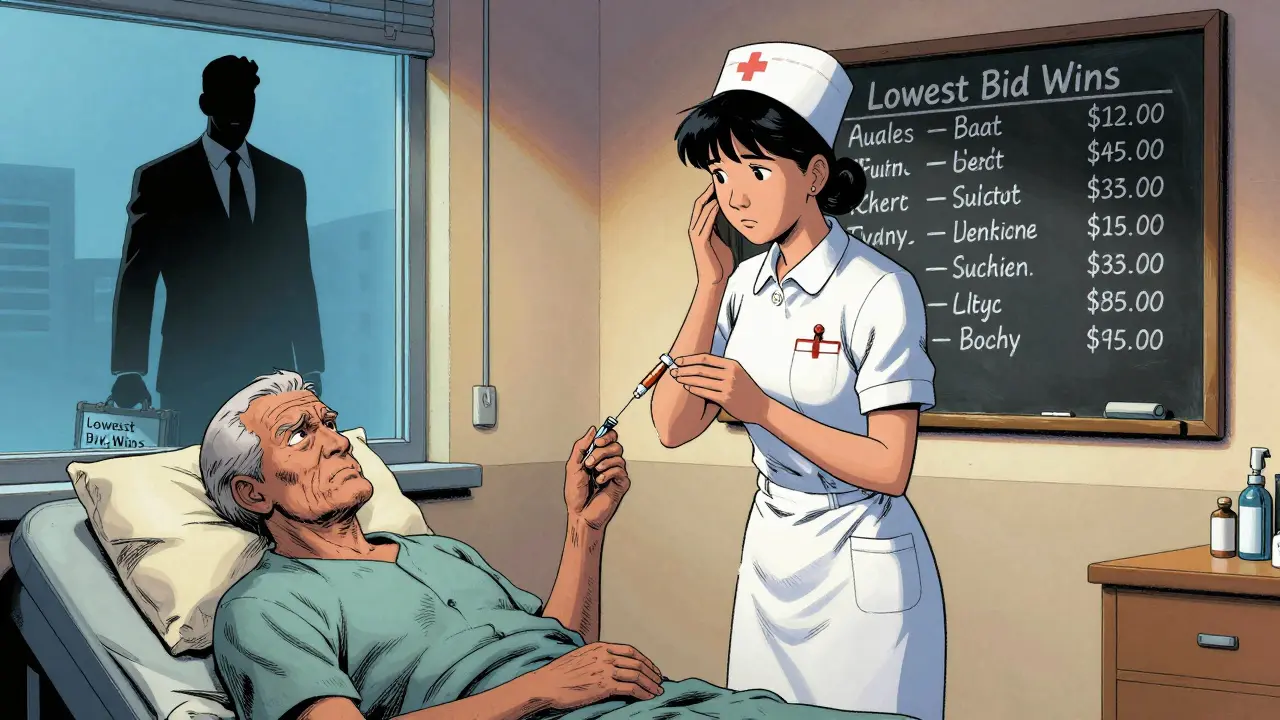
Generic manufacturers don’t have that luxury. They compete on price alone. The lowest bidder wins the contract. That means the company with the cheapest labor, the oldest equipment, and the tightest margins gets the deal. No one’s rewarded for reliability. No one’s penalized for cutting corners. And when a shortage hits, there’s rarely a therapeutic alternative. You can’t swap out insulin for a different insulin. You can’t replace heparin with something else and expect the same result.
Between 2018 and 2023, there were 1,391 shortages of generic drugs versus just 600 for brand-name drugs-even though generics are used far more often. That’s not a coincidence. It’s a design flaw.
What’s Being Done-and Why It’s Not Enough
The FDA has tried. They created a Drug Shortage Task Force. They’ve pushed for better early warning systems. They’ve encouraged manufacturers to diversify their supply chains. In 2020, an executive order helped reduce shortages of essential medicines by 32%. But that progress stalled.
Since 2023, shortages have been creeping back up. The number of FDA-registered manufacturing facilities in the U.S. has dropped by 22% since 2015. Meanwhile, citations for quality violations have gone up 35%. The market is consolidating: the top 10 generic makers now control 60% of the business. That sounds like efficiency-but it’s actually risk. Fewer players mean fewer backups. One failure can trigger a cascade.
Proposed tariffs on imported drugs could make things worse. If you slap a 50-200% tax on APIs from India or China, manufacturers can’t afford to make the drugs. They’ll stop. And patients will lose access even faster.
The Real Cost: More Than Just Money
Hospitals spend $213 million a year just managing drug shortages. That’s on staff overtime, emergency purchases, training, and paperwork. But that’s just the financial cost. The human cost is harder to measure.
Pharmacists report increased stress, burnout, and moral injury. Nurses worry they’re giving the wrong dose because the labeled vial doesn’t match what’s in the cabinet. Patients are terrified their treatment will be delayed. One hospital pharmacist on Reddit wrote: “We’ve been out of vancomycin powder for eight months. We’re using alternatives that are less effective-and we know it.”
And here’s the thing: no one’s talking about this enough. We hear about drug prices. We hear about insurance denials. But we rarely hear about the drugs that simply aren’t there. And when they’re gone, there’s no app to fix it. No website to order from. No substitute that works as well.
What Needs to Change
Fixing this isn’t about finding a miracle tech solution. It’s about fixing the market.
- Pay manufacturers more for reliable supply-not just the lowest bid.
- Incentivize companies to keep backup production lines running, even if they’re not at full capacity.
- Require multiple manufacturers for critical drugs-no more single-source approvals.
- Build domestic manufacturing capacity for essential injectables and APIs.
- Hold companies accountable for quality, not just price.
Right now, the system rewards the cheapest, not the safest. That has to change. Otherwise, by the end of 2026, we could see over 350 drugs in short supply-with two-thirds of them being life-saving injectables.
Patients shouldn’t have to gamble on whether their medicine will be there next week. The system should guarantee it.
Why are generic drug shortages so common compared to brand-name drugs?
Generic drugs are more vulnerable because they’re sold at razor-thin profit margins-often just 5-10%. Manufacturers compete on price, not reliability, so they cut corners on quality, maintenance, and backup capacity. Brand-name drugs have higher margins, so companies can afford to invest in quality control and inventory buffers. Plus, generics often have only one or two manufacturers, while brand drugs usually have multiple suppliers.
Which types of generic drugs are most likely to be in short supply?
Sterile injectables are the most vulnerable-about 60% of all shortages involve these drugs. Examples include vancomycin, cisplatin, saline, and heparin. They require complex, sterile manufacturing environments that are expensive to maintain. Small contamination issues shut down entire production lines. And because they’re often low-margin, companies don’t invest in redundancy.
How do drug shortages affect patient care?
Shortages force doctors to use less effective or more toxic alternatives. Cancer patients get delayed chemo. Diabetics can’t get insulin. Patients with infections get broader-spectrum antibiotics that increase resistance. In 2022, 63% of pharmacists reported that shortages led to serious adverse outcomes, including hospitalizations and deaths. Many patients abandon prescriptions altogether due to cost or unavailability.
Is the U.S. manufacturing base to blame for drug shortages?
It’s part of the problem. The number of FDA-registered generic drug manufacturing facilities in the U.S. has dropped 22% since 2015. Many companies moved production overseas to cut costs, especially for active pharmaceutical ingredients (APIs). Now, over 80% of APIs come from China and India. A single regulatory inspection, natural disaster, or political issue in those countries can disrupt supply to the entire U.S. healthcare system.
What’s being done to fix the problem?
The FDA has created a Drug Shortage Task Force and pushed for better early warning systems. Executive Order 14050 helped reduce shortages of essential medicines by 32% between 2020 and 2023. But progress has stalled. Experts say real change requires financial incentives for reliable production, requirements for multiple manufacturers per drug, and rebuilding domestic manufacturing capacity. Without policy changes, shortages are expected to rise to 350 by the end of 2026.
14 Comments
Beth Templeton
January 7, 2026 at 13:17 PM
Generic drugs are cheap because they’re cheap to make. Fix the pricing model or shut up.
Katie Schoen
January 8, 2026 at 20:17 PM
Bro the fact that we’re using alternatives we know are less effective and calling it ‘clinical judgment’ is insane. We’re not doctors-we’re triage artists with a side of guilt. 🤦♀️
Wesley Pereira
January 9, 2026 at 12:59 PM
Let’s be real-this is supply chain capitalism at its finest. We outsourced production to cut costs, now we’re outsourcing patient safety. The FDA’s ‘task force’ is just a PR stunt with a PowerPoint. We need policy, not posters.
Ryan Barr
January 10, 2026 at 14:28 PM
Capitalism doesn’t reward reliability. It rewards efficiency. You want safety? Pay more. Simple.
Amy Le
January 11, 2026 at 16:14 PM
China and India are the problem. We need to bring this back to America. National security. End of story.
Melanie Clark
January 12, 2026 at 22:05 PM
Of course this is happening the FDA is corrupt and the pharmaceutical industry owns Congress. They want us sick so they can keep selling expensive alternatives. You think they care about vancomycin? They care about stock prices. This isn’t a shortage-it’s a controlled collapse. Wake up.
They’ve been quietly removing safety checks for years. Every time a plant gets cited, they just pay a fine and keep going. The FDA is a rubber stamp for Big Pharma. And now we’re paying with our lives.
Did you know the same companies that make these generics also own the brand-name versions? They create the shortage so you’ll pay more for the ‘premium’ version. It’s not incompetence-it’s strategy.
They don’t want you healthy. They want you dependent. They want you scared. They want you to believe there’s no alternative. But there is. Vote. Protest. Demand transparency. Or keep pretending this is just bad luck.
I’ve seen nurses cry because they had to give a child a less effective antibiotic. I’ve seen elderly patients die because their blood pressure med wasn’t there. And the CEOs? They got bonuses. Again.
It’s not a system failure. It’s a design. And we’re all just living in it.
Tiffany Adjei - Opong
January 14, 2026 at 14:32 PM
Wow so the solution is to pay more? That’s it? You’re not even considering how this is a symptom of our entire healthcare system being a profit-driven horror show. We’re not fixing the drug shortage-we’re just putting a Band-Aid on a hemorrhage.
And why are we still letting single-source approvals exist? That’s like building a bridge with one support beam and calling it ‘efficient.’
Also, the fact that we’re importing 80% of APIs from two countries while our own manufacturing capacity dropped 22% since 2015? That’s not globalization-that’s national suicide.
And don’t even get me started on how the FDA approves plants with 30+ violations and calls it ‘compliance.’
Everyone’s blaming China. But the real villain is the American consumer who wants $5 antibiotics and doesn’t care how they’re made.
Dana Termini
January 16, 2026 at 06:57 AM
I’ve been a pharmacist for 18 years. I’ve seen this cycle repeat. Every time we get a little progress, the market shifts again. It’s not about blame-it’s about structure. We need mandatory multi-source approvals for critical drugs. No exceptions. And we need to fund domestic API production like we do for defense. This isn’t optional anymore.
Pavan Vora
January 16, 2026 at 18:53 PM
From India, I see this every day. Our factories are running flat out, but the quality inspections are so strict now, one tiny dust particle shuts everything down. We want to help, but the rules keep changing. And the prices? They’re so low, we can’t even pay our workers overtime. It’s not greed-it’s survival.
We’re not the enemy. We’re the middleman in a broken system. Please don’t hate us. We’re trying.
Isaac Jules
January 18, 2026 at 10:49 AM
Oh wow, someone finally said it. The system is rigged. But guess what? You’re not special. You’re just the 10,000th person to notice. Wake up. This is how capitalism works. You want medicine? Pay. Or die. No tears, no drama. Just math.
Stuart Shield
January 20, 2026 at 08:11 AM
This feels like watching a slow-motion car crash where everyone’s got their seatbelt on but no one’s got a steering wheel. We’ve got the brakes, we’ve got the lights, we’ve got the maps-but we’ve lost the will to drive anywhere but straight into the wall.
It’s not just about drugs. It’s about trust. When your pharmacist looks you in the eye and says, ‘I’m sorry, we don’t have it,’ you don’t just lose a medication-you lose faith in the whole damn system.
Molly McLane
January 21, 2026 at 01:59 AM
Hey everyone-I’m a nurse in Ohio. I just wanted to say thank you to the pharmacists. You’re the unsung heroes holding this together. I’ve watched you spend 18 hours a week on the phone just to get a vial of saline. You deserve a medal. Or at least a raise. We’re not asking for miracles. Just enough to keep people alive.
And to the people who say ‘just make more’-it’s not that simple. It takes 3 years to build a sterile facility. You can’t just flip a switch. We need investment. Now.
Let’s not wait for someone to die before we act. Let’s act before the next crisis hits.
Wesley Pereira
January 22, 2026 at 15:53 PM
^This. And to the person who said ‘China’s the problem’-no. The problem is that we let them become the only option by starving our own infrastructure. We didn’t lose manufacturing-we abandoned it. And now we’re mad when the house burns down.






Kelly Beck
January 5, 2026 at 17:55 PM
This is so real it hurts 😭 I work in a rural clinic and we’ve been out of saline for months. We’re diluting IV bags with distilled water just to keep people alive. No one’s talking about how this is a slow-motion massacre. We’re not just running low on meds-we’re running out of dignity.