
Every year, millions of people in the U.S. receive the wrong medication, wrong dose, or wrong instructions - not because of malice, but because of simple, preventable mistakes. These aren’t rare glitches. They’re systemic issues, and they look very different depending on whether the error happens in a hospital or your local pharmacy.
How Often Do Errors Happen?
In hospitals, medication errors are shockingly common. One major study found that nearly 1 in 5 doses given to patients contained some kind of mistake. That’s 20%. Think about it: if you’re in the hospital and get 10 medications in a day, chances are one of them is wrong. These errors show up during prescribing, transcribing, dispensing, and especially during administration - when nurses give you the drug. In retail pharmacies, the numbers are much lower. Research shows about 1.5% of all prescriptions filled have a dispensing error. That sounds small, but when you consider that U.S. pharmacies fill over 3 billion prescriptions a year, that’s more than 45 million mistakes annually. A typical community pharmacy filling 250 prescriptions a day might make four errors every single day. Here’s the catch: hospital errors are more frequent, but they’re often caught before they hurt you. Pharmacy errors are rarer - but they’re more likely to reach you undetected.What Kind of Errors Happen Where?
In hospitals, the biggest problems happen when drugs are given to patients. Nurses might give the right drug but at the wrong time. Or they might give the right dose, but to the wrong person. Timing errors, wrong dosages, and mix-ups between look-alike drugs like morphine and hydromorphone are common. These mistakes often happen because staff are rushed, understaffed, or overwhelmed by complex patient cases. In retail pharmacies, the errors are different. Most are transcription mistakes - when the pharmacist misreads or miskeys what the doctor wrote. One famous case involved a patient given estradiol 1 tablet twice per day instead of twice per week. That’s a 14-fold overdose. Another common error is giving the wrong strength - like 10 mg instead of 1 mg. Sometimes, the directions are wrong: “take with food” becomes “take on an empty stomach.” The NIH found that in community pharmacies, about half of all errors were clinical (like wrong dose or drug interaction) and half were administrative (like labeling or data entry mistakes). Most of these errors were caught during pharmacy quality checks - but not all.Why Are Hospital Errors More Likely to Be Caught?
Hospitals have layers of safety nets. A doctor writes the order. A pharmacist reviews it. A nurse checks the label before giving it. Many hospitals now use barcode scanners that scan your wristband and the drug - if they don’t match, the system won’t allow it. One study showed barcode systems cut errors by up to 86%. Retail pharmacies don’t have that. Once the pharmacist fills the prescription, it goes straight to you. There’s no nurse to double-check. No scanner to verify. You’re the last line of defense. And most people don’t know what their medication is supposed to look like, or what the correct dose should be. Dr. David Bates from Harvard put it simply: “Hospital errors are more frequent but have more safety nets. Community pharmacy errors are less frequent but more likely to reach the patient unchecked.”
Who Pays the Price?
When a hospital error causes harm, the patient is often already in a critical condition. The injury might be severe - kidney failure, internal bleeding, cardiac arrest - but it’s usually caught quickly, and treatment starts fast. The cost to treat these injuries in hospitals alone is at least $3.5 billion a year. In retail pharmacies, the harm is quieter but just as dangerous. A patient takes the wrong dose of warfarin or insulin and ends up in the ER. Or they develop a bad reaction because a drug interaction was missed. These errors lead to emergency room visits, hospitalizations, and sometimes death. The total economic cost of all medication errors - in hospitals and pharmacies - is estimated at $177 billion per year in the U.S. A 2007 study found that for every 10,000 prescriptions filled in a community pharmacy, about three led to hospitalization. That’s not a small number. It’s happening in your neighborhood pharmacy.Why Do These Mistakes Keep Happening?
In hospitals, the root causes are staffing shortages, poor communication between teams, and high patient complexity. A nurse might be juggling five patients. A doctor’s handwriting might be unclear. An electronic system might auto-fill the wrong drug. In pharmacies, the problem is mostly human cognitive overload. Pharmacists are under pressure to fill prescriptions fast. They’re interrupted constantly - by phone calls, customers, other staff. A 2023 AHRQ report found that about 80% of pharmacy errors are caused by mental lapses tied to workload, environment, or technology glitches. Automated dispensing machines can help - but they can also create new errors if staff don’t understand them. Both settings suffer from underreporting. In hospitals, errors are logged, but many go unreported because staff fear blame. In pharmacies, reporting is even worse. Until recently, most states didn’t require pharmacies to report errors at all. Now, places like California demand logs - but compliance is still inconsistent.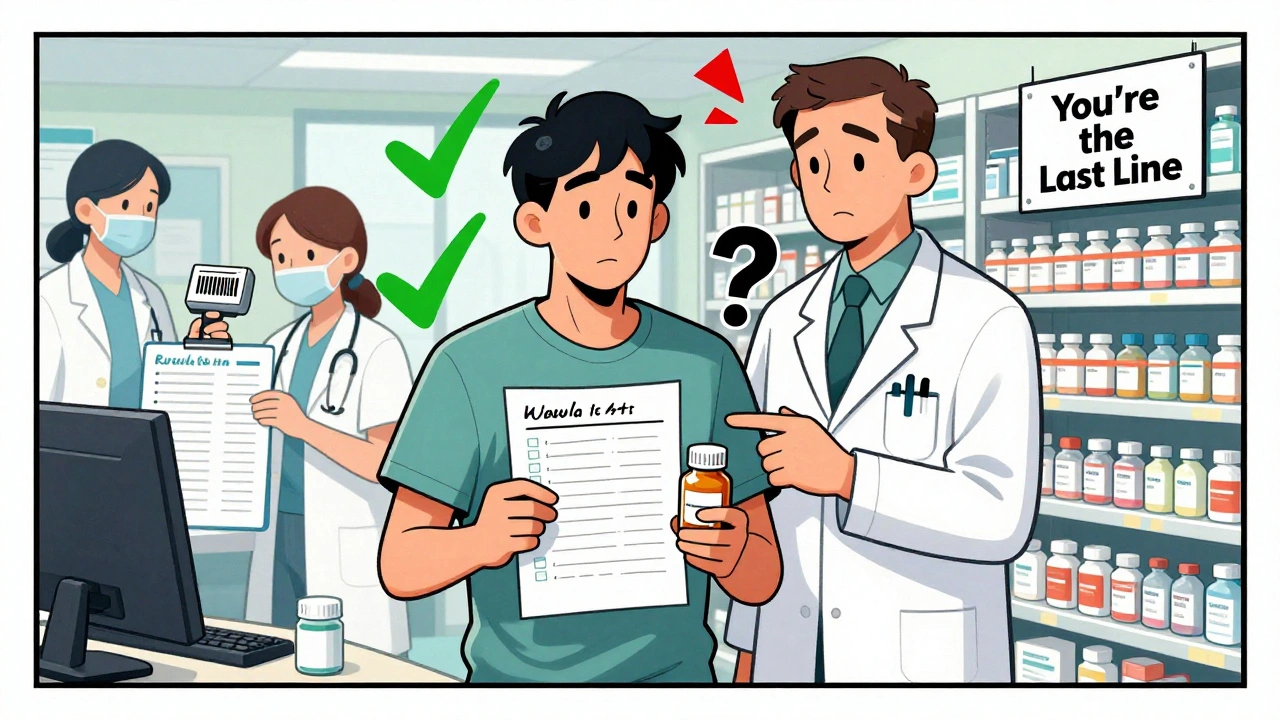
What’s Being Done to Fix This?
Hospitals are investing in technology. Mayo Clinic reduced errors by 52% after linking their electronic health records directly to the pharmacy system. CVS Health cut dispensing errors by 37% using AI-powered verification tools that flag mismatches before the drug leaves the counter. Community pharmacies are catching up. Clinical Decision Support Systems (CDSS) now warn pharmacists if a dose is too high, if a drug interacts with another, or if the prescription doesn’t match the patient’s history. These tools aren’t perfect - but they’re better than nothing. The CDC and FDA are pushing for standardized error reporting across all pharmacy settings. Without consistent data, we can’t fix what we don’t measure.What Can You Do?
You’re not powerless. Here’s what works:- Always ask: “What is this medicine for? How should I take it? What side effects should I watch for?”
- Compare the pill in the bottle to the description on the label. If it looks different from your last refill, ask.
- Keep a list of all your medications - including over-the-counter drugs and supplements - and bring it to every appointment.
- If you’re given a new prescription, call your pharmacy to confirm the dose and instructions before you take it.
- Don’t be afraid to say: “I think this might be wrong.”
Is One Setting Safer Than the Other?
No. Neither is “safe.” Hospitals have more errors, but more checks. Pharmacies have fewer errors - but fewer safeguards. The real danger isn’t the setting. It’s the assumption that someone else is watching out for you. The truth is, medication safety isn’t just about technology or training. It’s about culture. In hospitals, teams are trained to speak up. In pharmacies, the pressure to move quickly often silences caution. The future of safety lies in combining the best of both worlds: better tech in pharmacies, and better communication in hospitals. But until then, your vigilance is the most reliable safety net you’ve got.How common are medication errors in hospitals?
Medication errors in hospitals are very common. Studies show that about 20% of all medication doses administered in hospitals contain some kind of mistake - whether it’s the wrong drug, wrong dose, wrong timing, or wrong patient. These errors most often happen during the administration phase, when nurses give the medication.
What’s the error rate in retail pharmacies?
Retail pharmacies have a lower error rate - around 1.5% of all prescriptions dispensed. That sounds small, but with over 3 billion prescriptions filled annually in the U.S., that translates to roughly 45 million errors per year. Most are caught during pharmacy quality checks, but some still reach patients.
What are the most common types of pharmacy errors?
The most common pharmacy errors are incorrect medication, incorrect dose, and incorrect directions. Transcription errors - where the pharmacist misreads or miskeys the doctor’s order - are the biggest culprit. For example, writing “twice per day” instead of “twice per week” for a powerful drug like estradiol can lead to dangerous overdose.
Why are hospital errors more likely to be caught?
Hospitals have multiple safety checks: pharmacists review orders, nurses verify before giving drugs, and many use barcode scanning systems that match the patient, drug, and dose. If anything doesn’t line up, the system alerts staff. In retail pharmacies, once the prescription is filled, there’s no one else to check - you’re the last line of defense.
Can medication errors lead to death?
Yes. In the U.S., between 7,000 and 9,000 people die each year due to medication errors. Many of these deaths occur because of errors in hospitals, but a significant number come from pharmacy mistakes - especially with high-risk drugs like insulin, blood thinners, or opioids. Even a small dosing mistake can be fatal if the patient is elderly or has kidney or liver problems.
What’s the biggest factor causing errors in pharmacies?
The biggest factor is cognitive overload. Pharmacists are often juggling dozens of prescriptions, phone calls, insurance issues, and customer questions - all while working under time pressure. About 80% of pharmacy errors are linked to mental lapses caused by stress, interruptions, or poorly designed technology. It’s not laziness or incompetence - it’s a system that doesn’t account for how humans actually work.
Are there tools to prevent pharmacy errors?
Yes. Clinical Decision Support Systems (CDSS) flag dangerous doses, drug interactions, and allergies before the prescription is filled. AI-powered verification tools now scan prescriptions for mismatches between the doctor’s order and the dispensed drug. CVS and other major chains have cut errors by 30-40% using these tools. But they’re not everywhere yet - and they’re not foolproof.
What should I do if I think I got the wrong medicine?
Don’t take it. Call your pharmacy immediately and ask to speak to the pharmacist. Compare the pill to your previous prescription - color, shape, size, imprint code. Check the label against your doctor’s instructions. If anything seems off, ask for clarification. It’s better to be safe than sorry. Many people don’t speak up because they’re afraid of sounding foolish - but pharmacists expect these questions.
15 Comments
Laura Weemering
December 13, 2025 at 01:32 AM
Let’s be real: the system is designed to fail. Hospitals? Overworked staff. Pharmacies? Underpaid, over-stressed pharmacists doing 300 scripts a day while fielding insurance calls. It’s not malice-it’s structural collapse. And we’re supposed to trust this? 🤡
sandeep sanigarapu
December 14, 2025 at 02:28 AM
In India, we have fewer resources but more human checks. Elders often double-check prescriptions with family. Maybe we need more of that-human connection over automation.
Ashley Skipp
December 15, 2025 at 05:13 AM
People don’t read labels and then blame the system. If you can’t tell the difference between a blue pill and a white one you probably shouldn’t be taking meds at all
Robert Webb
December 16, 2025 at 02:41 AM
I’ve worked in both hospital pharmacy and retail, and the difference isn’t just tech-it’s culture. In hospitals, if you’re wrong, 10 people will stop you before you give the med. In retail? You’re alone with a screen and a screaming customer asking why their blood pressure med looks different. No one teaches you how to manage that pressure. The tech helps, but it doesn’t fix the exhaustion. And exhaustion is what kills.
nikki yamashita
December 16, 2025 at 17:37 PM
Y’all need to ask more questions!! It’s not rude-it’s radical self-care. I ask my pharmacist every time. She thinks I’m weird. I think she’s awesome.
Adam Everitt
December 17, 2025 at 14:11 PM
the system is broke. not just broken-broke. like, financially. pharmacists get paid peanuts to do brain surgery under pressure. no wonder mistakes happen. and yeah, barcodes help but they dont fix a culture that rewards speed over safety
wendy b
December 18, 2025 at 14:56 PM
Let me be clear: the average American is too lazy to read a medication label. This isn't a systemic failure-it's a failure of personal responsibility. If you can't spell 'ibuprofen' you shouldn't be allowed to take it.
Rob Purvis
December 18, 2025 at 15:44 PM
Barcodes aren’t magic. I saw a nurse scan the wrong wristband-twice-and the system didn’t flag it because the barcode was slightly smudged. Tech is only as good as the person using it. We need better training, better lighting, better breaks. Not just more scanners.
Donna Anderson
December 18, 2025 at 23:59 PM
My mom got the wrong blood thinner and ended up in the ER. I didn’t know what to look for. Now I take a pic of every new pill and google it. You don’t have to be a doctor to be smart about this.
Levi Cooper
December 20, 2025 at 05:09 AM
Why are we letting foreign-trained pharmacists fill our prescriptions? In America, we used to have standards. Now? Anyone with a visa and a degree can hand you a vial of death. This is why our healthcare is failing.
Nathan Fatal
December 20, 2025 at 11:39 AM
The real issue isn’t the error rate-it’s the normalization of risk. We accept 1 in 5 hospital dosing errors like it’s traffic noise. We treat pharmacy mistakes as ‘oops’ moments. But when you’re the one getting the wrong drug, it’s not noise. It’s trauma. We need to stop calling them ‘errors’ and start calling them ‘preventable harms.’ Language shapes action.
Stacy Foster
December 21, 2025 at 11:41 AM
Did you know the FDA gets less than 1% of all pharmacy errors reported? That’s because the companies bury them. Big Pharma and CVS know this. They profit from your confusion. Your insulin price went up 300%? The dose you got? Probably wrong. It’s all connected. Wake up.
Reshma Sinha
December 22, 2025 at 15:35 PM
At my hospital in Mumbai, we use a color-coded system for high-risk meds. Red for insulin, blue for opioids. No barcodes, no tech-just visual cues. Simple. Effective. Maybe we don’t need AI. Maybe we just need to slow down and see.
Lawrence Armstrong
December 23, 2025 at 18:43 PM
My cousin works at a pharmacy. She told me they get 12 minutes per script during peak hours. Twelve minutes to check allergies, drug interactions, dosage, patient history, insurance, and answer three questions. And if they take longer? They get written up. No wonder mistakes happen. It’s not the pharmacist’s fault. It’s the schedule. 🤕






Audrey Crothers
December 12, 2025 at 01:11 AM
Just had my grandma almost get the wrong insulin dose last month. Thank god the pharmacist double-checked the script. We all need to speak up - it’s not being annoying, it’s saving lives. 🙏