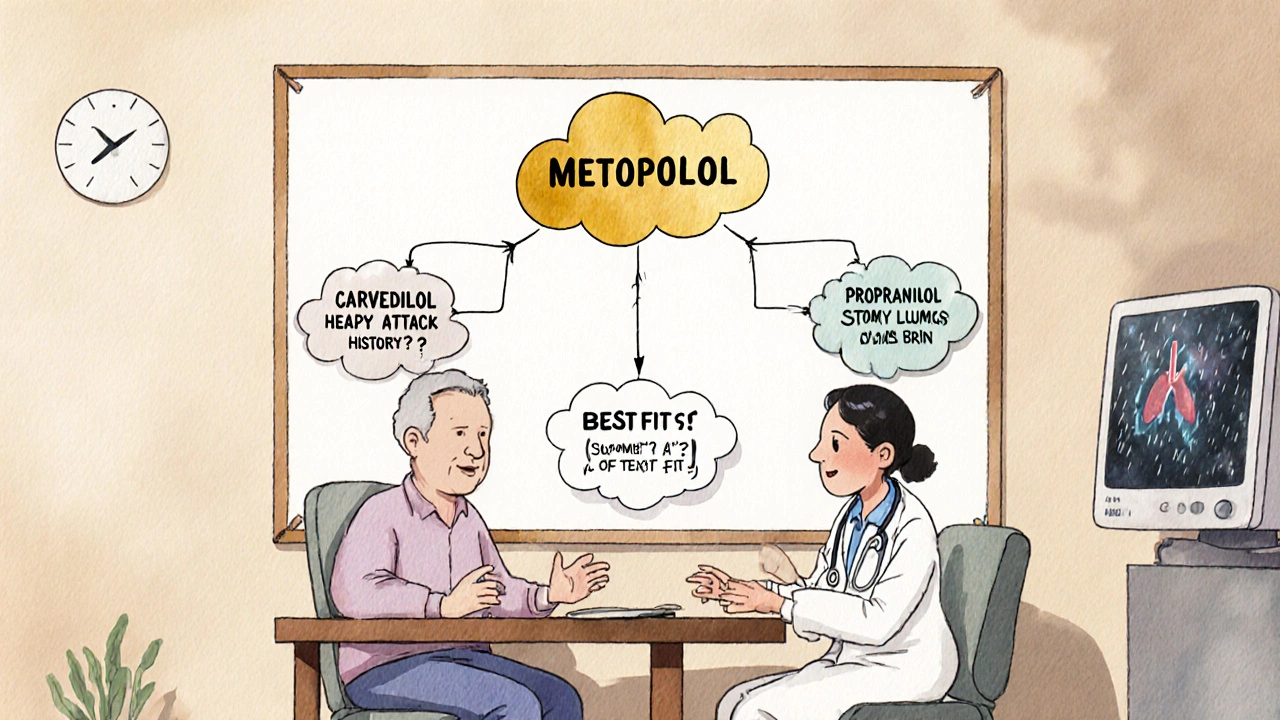
When your doctor says you need a beta blocker, you might hear names like metoprolol, atenolol, propranolol, or carvedilol. They all do similar things-lower blood pressure, slow your heart rate, reduce chest pain-but they’re not the same. If you’ve been prescribed metoprolol, you’re probably wondering: why this one and not another? What’s special about it? The answer isn’t just about chemistry. It’s about how your body uses it, what side effects you’re likely to get, and whether it fits your specific heart condition.
What Metoprolol Actually Does
Metoprolol is a beta blocker that targets beta-1 receptors, mostly found in the heart. That’s its main job: to calm down your heart without messing too much with your lungs or blood vessels. Think of it like a volume knob for your heartbeat. When you have high blood pressure, angina, or a history of heart attack, your heart is working too hard. Metoprolol turns the volume down, letting your heart rest and recover.
It comes in two forms: metoprolol tartrate (short-acting) and metoprolol succinate (long-acting). The tartrate version is taken two or three times a day. The succinate version is usually once daily, which is why many doctors prefer it for long-term use. It’s not just about convenience-steady levels in your blood mean fewer spikes and dips in heart rate, which helps prevent sudden stress on your heart.
How It Compares to Atenolol
Atenolol is another beta blocker often used for high blood pressure. It’s cheap, widely available, and works well. But here’s the difference: atenolol doesn’t cross the blood-brain barrier. That sounds technical, but it means it’s less likely to cause things like fatigue, depression, or sleep problems. Metoprolol, on the other hand, can enter the brain. For some people, that leads to more tiredness or mood changes. For others, it doesn’t matter at all.
Studies show both drugs lower blood pressure equally well. But metoprolol has more evidence for reducing death after a heart attack. A 2023 meta-analysis of over 12,000 patients found that metoprolol reduced the risk of cardiac death by 23% compared to placebo, while atenolol showed only a 14% reduction. That’s not a huge gap, but in heart disease, even small differences matter.
Why Metoprolol Beats Propranolol for Heart Conditions
Propranolol is the original beta blocker. It’s been around since the 1960s and is still used for migraines, anxiety, and tremors. But it blocks both beta-1 and beta-2 receptors. That means it affects your heart and your lungs, blood vessels, and even your metabolism. If you have asthma or COPD, propranolol can make breathing harder. That’s why it’s avoided in people with lung issues.
Metoprolol is more selective. It leaves beta-2 receptors mostly alone. That makes it safer for people with mild lung disease. If you’re on metoprolol and still have wheezing or shortness of breath, your doctor might still be cautious-but they’re less likely to pull the plug on the medication.
Metoprolol also doesn’t affect blood sugar as much as propranolol. For people with diabetes, that’s a big deal. Propranolol can hide the warning signs of low blood sugar-like shaking or a fast heartbeat-because it blocks the body’s natural stress response. Metoprolol doesn’t do that as much. You’re still at risk, but you’re more likely to feel the warning signs before things get dangerous.
Carvedilol: The All-Rounder
Carvedilol is different. It’s not just a beta blocker-it’s also an alpha blocker. That means it relaxes blood vessels too. That’s why it’s often used for heart failure. Studies like the COPERNICUS trial showed carvedilol reduced death in heart failure patients by 35%. Metoprolol didn’t do as well in those same trials.
But here’s the catch: carvedilol is harder on your blood pressure. It can drop it too low, especially when you first start. You might feel dizzy, lightheaded, or faint. Metoprolol is gentler on the way down. If you’re older or have low blood pressure to begin with, metoprolol might be the safer pick.
Carvedilol also causes more weight gain and swelling in the legs. Metoprolol? Less likely. If you’re trying to manage fluid retention, metoprolol might be the better fit.

Who Gets Prescribed Metoprolol?
Metoprolol isn’t the best for everyone. But it’s often the first choice for:
- People who’ve had a heart attack-especially if they’re still recovering
- Those with high blood pressure who also have diabetes
- Patients with angina (chest pain) who need steady heart rate control
- People with mild lung disease who can’t take propranolol
- Anyone who needs once-daily dosing without the side effects of carvedilol
If you’re young and have anxiety-related palpitations, your doctor might pick propranolol instead. If you have severe heart failure, carvedilol is probably the go-to. But for most middle-aged or older adults with high blood pressure and a history of heart trouble, metoprolol hits the sweet spot: effective, safe, and easy to take.
Side Effects You Should Watch For
All beta blockers can cause dizziness, tiredness, cold hands or feet, and slow heart rate. But metoprolol has some unique risks:
- Masking low blood sugar symptoms (especially if you’re diabetic)
- Worsening depression or sleep issues in sensitive people
- Getting worse chest pain if you stop it suddenly
Never quit metoprolol on your own. If you stop suddenly, your heart can go into overdrive. That’s called rebound hypertension or tachycardia. It can trigger a heart attack. If you need to stop, your doctor will slowly reduce your dose over weeks.
Some people report vivid dreams or nightmares. That’s more common with metoprolol than with atenolol. If this happens, talk to your doctor. Switching to the succinate form (once daily) often helps-it gives more stable levels and reduces brain exposure at night.
What About Cost and Availability?
Metoprolol is generic. So is atenolol. Both cost less than $10 a month in Australia with a PBS subsidy. Carvedilol and propranolol are also cheap. Price isn’t usually the deciding factor. What matters is how your body responds.
Insurance plans sometimes prefer one over the other. If your plan covers metoprolol but not carvedilol, that might steer your doctor’s choice. But if you’re paying out of pocket, it’s still about fit-not cost.
What If Metoprolol Doesn’t Work?
Not everyone responds the same. About 1 in 5 people don’t get enough blood pressure control from metoprolol alone. That doesn’t mean it’s failing-it might just need help. Your doctor might add a diuretic, an ACE inhibitor, or a calcium channel blocker. You don’t have to switch beta blockers right away.
If you’re still having chest pain, or your heart rate stays too high, your doctor might switch you to carvedilol. If you’re having side effects like fatigue or depression, they might try atenolol instead. It’s trial and error, but you’re not stuck.
Final Takeaway: It’s About Fit, Not Just Function
Metoprolol isn’t the strongest beta blocker. It’s not the cheapest. But it’s the most balanced. It protects the heart without wrecking your lungs. It helps after a heart attack without crashing your blood pressure. It’s gentle enough for diabetics and simple enough for once-daily use.
Choosing between beta blockers isn’t about which one is ‘best.’ It’s about which one fits you. Your age. Your other conditions. Your lifestyle. Your side effect tolerance. If metoprolol works for you-no major side effects, steady heart rate, no chest pain-stick with it. If it’s not working, your doctor has other options. But don’t assume another beta blocker is better just because it’s different. Sometimes, the best choice is the one you’re already on.
Is metoprolol better than atenolol for high blood pressure?
Both lower blood pressure equally well. But metoprolol has stronger evidence for reducing death after a heart attack. Atenolol is less likely to cause fatigue or sleep issues because it doesn’t cross into the brain. If you’re young and healthy with just high blood pressure, atenolol might be simpler. If you’ve had heart damage, metoprolol is usually preferred.
Can I take metoprolol if I have asthma?
Metoprolol is safer than propranolol for people with mild asthma because it’s more selective for the heart. But it’s not risk-free. If you have active wheezing or severe COPD, your doctor will be cautious. They might start with a low dose and monitor you closely. Never take it without medical supervision if you have lung disease.
Does metoprolol cause weight gain?
Some people gain a little weight on beta blockers, but metoprolol is less likely to cause this than carvedilol or propranolol. Weight gain is usually mild-under 2 kg-and often linked to fluid retention or reduced activity due to fatigue. If you notice sudden swelling or rapid weight gain, tell your doctor-it could be a sign your heart isn’t pumping well enough.
Why does my doctor want me to take metoprolol succinate instead of tartrate?
Metoprolol succinate is a slow-release version. It gives steady levels in your blood over 24 hours, so you only need one pill a day. That means fewer peaks and drops in heart rate, which reduces stress on your heart. It’s also linked to better outcomes in heart failure and after heart attacks. Tartrate is cheaper and works fine for some, but succinate is the preferred form for long-term use.
Can I drink alcohol while taking metoprolol?
Alcohol can lower your blood pressure even more than metoprolol already does. That increases your risk of dizziness, fainting, or falls. It can also make you feel more tired. If you drink, do it in small amounts and avoid it when you first start the medication. If you feel lightheaded after drinking, stop and talk to your doctor.
What to Do Next
If you’re on metoprolol and feeling fine-no dizziness, steady energy, no chest pain-you’re probably on the right track. Keep taking it as prescribed. Don’t skip doses, even if you feel good.
If you’re not sure why you’re on it, ask your doctor. Write down your symptoms: Do you feel more tired? Is your heart racing sometimes? Are you dizzy when you stand up? Bring that list to your next appointment. That’s how you get the best care-not by guessing which beta blocker is ‘best,’ but by seeing which one works best for you.
10 Comments
Brad Seymour
November 8, 2025 at 05:44 AM
Okay but let’s be real-atenolol is the real MVP for simple high BP. Cheap, clean, no brain fog. Metoprolol’s just fancy marketing wrapped in a fancy name. I’ve seen patients on metoprolol come in with nightmares and depression, then switch to atenolol and suddenly they’re laughing again. Why are we overcomplicating this? If you don’t have heart damage, why risk the brain side effects? Just sayin’.
Malia Blom
November 8, 2025 at 08:25 AM
Wow. So metoprolol is ‘balanced’? That’s the best you got? 😂 Like, what does ‘balanced’ even mean in medicine? It’s just a molecule. It doesn’t care about your ‘fit.’ You’re anthropomorphizing a beta receptor blocker. Also, ‘gentler on blood pressure’? Bro, ALL beta blockers lower BP. Carvedilol just does it better for heart failure. And don’t get me started on that ‘23% vs 14%’ stat-absolute risk reduction is like 0.8%. You’re selling a placebo effect wrapped in a meta-analysis. 🤡
Erika Puhan
November 9, 2025 at 17:25 PM
Metoprolol succinate is the gold standard, period. The pharmacokinetics are superior: Cmax lower, Tmax delayed, AUC more consistent. Unlike tartrate, which induces fluctuating beta-blockade, succinate maintains therapeutic plasma concentrations for 24 hours, reducing sympathetic rebound. Also, the MERIT-HF trial demonstrated 34% mortality reduction in HFrEF-this isn’t anecdotal, it’s evidence-based. If you’re prescribing tartrate for chronic conditions, you’re practicing outdated medicine. #Pharmacoepidemiology
Edward Weaver
November 11, 2025 at 10:01 AM
Y’all are overthinking this. Metoprolol’s American-made. Atenolol? British. Carvedilol? German. Propranolol? British again. We make the best meds here. If you’re not on metoprolol, you’re just letting foreign pharma companies profit off your heart. Also, if you’re diabetic and on propranolol, you’re asking for trouble. We know this. The FDA didn’t approve metoprolol for post-MI because it’s trendy-it’s because it works. End of story. 🇺🇸
Lexi Brinkley
November 12, 2025 at 00:29 AM
my doctor put me on metoprolol succinate and i swear i feel like a new person 🥹 no more dizzy spells, no more 3am heart palpitations… also i can finally drink coffee again 😭 thank u science 💖
Kelsey Veg
November 13, 2025 at 18:35 PM
metoprolol made me so tired i couldnt even walk to my car. switched to atenolol and now i run 5k every morning. also no weird dreams. the whole ‘crosses blood brain barrier’ thing is real. why are docs still pushing this? 😴
Alex Harrison
November 13, 2025 at 20:47 PM
Just wanted to say I’ve been on metoprolol for 8 years. Had a stent in 2016. I used to think it was just a pill. Now I realize it’s what keeps me alive. I don’t feel it working, but I feel the difference in my life. No chest pain. No ER visits. I’m 62 and still hiking. Don’t underestimate the quiet power of this med. Also, never stop it cold. I saw a guy do that and he ended up in the ICU. Don’t be that guy.
Jay Wallace
November 14, 2025 at 14:50 PM
Let’s be clear: metoprolol succinate is not ‘better’-it’s just more expensive. The tartrate formulation is bioequivalent in 80% of patients. The ‘once-daily’ advantage? Mostly marketing. The FDA even says so. And that ‘23% reduction’? You’re citing relative risk. Absolute risk reduction? 0.8%. That’s 125 patients treated to save one life. That’s not medicine-that’s pharmaceutical economics. And don’t get me started on the ‘gentle’ claim-beta-blockers are blunt instruments. Period.
Alyssa Fisher
November 15, 2025 at 16:07 PM
I think the real takeaway here isn’t about chemistry or trials-it’s about listening. The body doesn’t care about drug names. It cares about how it feels. I had a patient once who couldn’t sleep, was depressed, and had cold hands on metoprolol. Switched to atenolol-she cried because she could finally sleep through the night. Medicine isn’t about which drug is ‘best.’ It’s about which one lets you live. And sometimes, that’s not the one with the most studies. It’s the one that lets you hold your grandkid without feeling like you’re running a marathon just to breathe.






Cris Ceceris
November 6, 2025 at 14:59 PM
Man, I’ve been on metoprolol for three years now after my mini-heart-attack scare. What nobody talks about is how it quietly saves your life without you even noticing. No more racing heart when you climb stairs. No more panic when your pulse hits 90. It’s like your heart finally got a vacation. I switched from tartrate to succinate last year and it’s night and day-no more 3pm crashes. Seriously, if you’re on this med and feel fine? Don’t touch it. Let it do its quiet work.