Medicaid Tiered Drug List: What It Means for Your Prescriptions
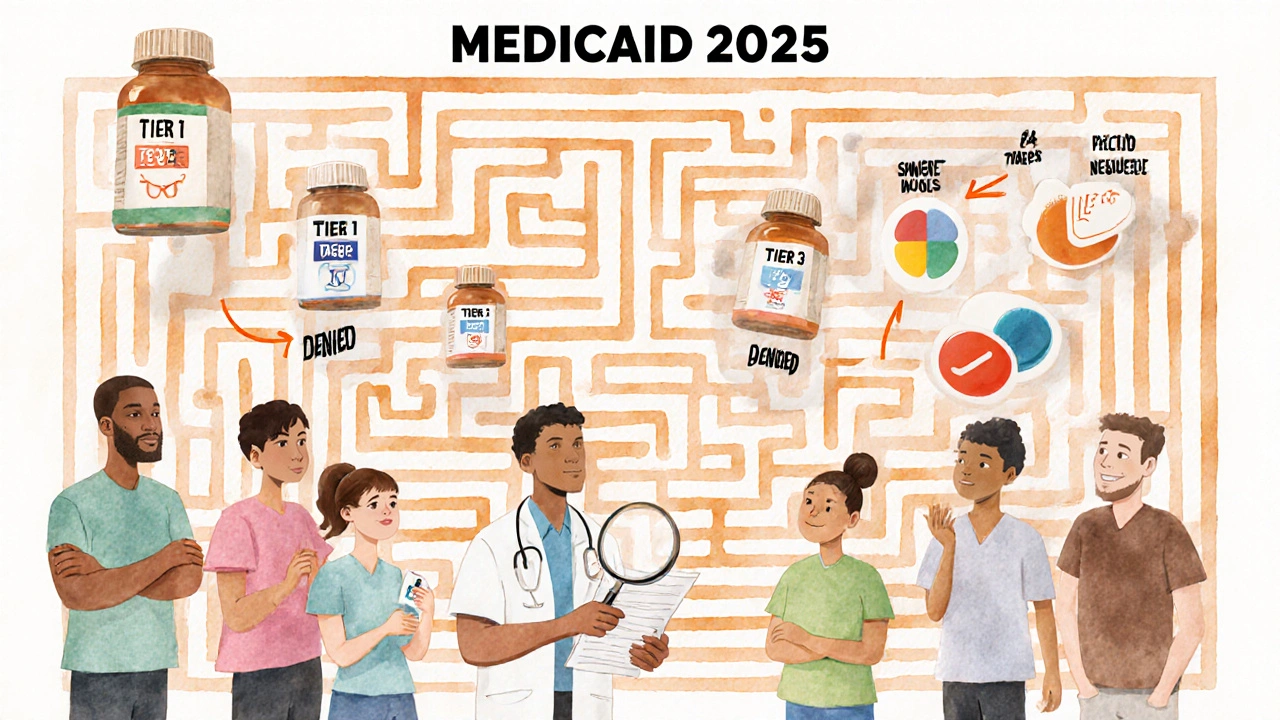
When you’re on Medicaid tiered drug list, a system that organizes prescription drugs into cost-based categories to control spending and encourage use of lower-cost options. Also known as a formulary, it determines how much you pay out-of-pocket for each medicine. This isn’t just paperwork—it directly impacts whether you can afford your pills, how often you refill them, and if your doctor needs to jump through extra hoops to get you the right treatment.
The formulary tiers, the levels that group medications by cost and clinical preference. Also known as drug tiers, it usually has five levels. Tier 1 is for generic drugs—often under $5. Tier 2 includes preferred brand-name meds. Tier 3 is for non-preferred brands, which cost more. Tier 4 is for high-cost specialty drugs, like those for cancer or autoimmune diseases. And Tier 5? That’s where you’ll find the most expensive treatments, often requiring prior authorization. If your drug is on Tier 3 or higher, you might pay $50, $100, or even more per prescription. That’s why knowing your plan’s list matters—many people don’t realize a cheaper, equally effective alternative might be just one tier down.
Drug prior authorization, a process where your doctor must prove to Medicaid that a higher-tier drug is necessary before they’ll cover it. Also known as pre-approval, it isn’t a delay tactic—it’s a safety net. For example, if you’re on a blood thinner like apixaban, Medicaid might require you to try warfarin first because it’s cheaper and well-studied. But if you’ve had bad reactions or can’t manage regular blood tests, your doctor can appeal. Same goes for drugs like omalizumab for chronic hives or acamprosate for alcohol dependence—these aren’t over-the-counter, and Medicaid needs proof they’re truly needed.
These rules aren’t random. They’re built from real-world data on what works, what costs less, and what’s safest. The Medicaid pharmacy benefits, the set of rules and covered medications under state-run Medicaid programs. Also known as state formularies, it varies by state. Some cover more generics. Some have stricter rules for antipsychotics or beta blockers like metoprolol. That’s why you can’t assume your friend’s coverage is yours. Always check your state’s current list—many have online tools to search by drug name.
If you’re paying too much, you’re not alone. People on Medicaid often don’t know they can switch to a generic version of a drug like Atacand or Pravachol without losing effectiveness. Or that a drug like promethazine might be replaced with a safer alternative like ondansetron, which isn’t just better—it’s often cheaper and covered at a lower tier. The narrow therapeutic index drugs, medications where small dosage differences can cause serious harm. Also known as NTI drugs, it like warfarin or levetiracetam get extra scrutiny because safety matters more than cost. But for most other drugs, the system is designed to push you toward what’s proven, affordable, and safe.
You’ll find real examples of this in the articles below. From how apixaban reduces stroke risk without the hassle of blood tests, to why metoprolol is often the first choice for heart patients, to how biosimilars are changing the game for expensive biologics—each post shows how these rules play out in real life. You’ll also see how people navigate prior authorization, avoid dangerous interactions, and find affordable alternatives without sacrificing care. This isn’t about bureaucracy—it’s about making sure you get the right medicine at a price you can live with. Let’s break it down.
Medicaid Coverage for Prescription Medications: What’s Included in 2025
Medicaid covers most prescription drugs, but coverage varies by state. Learn how formularies, step therapy, prior authorization, and Extra Help affect your out-of-pocket costs in 2025.
View More




