Anticoagulant Bleeding Risk Calculator
Personalize your risk assessment
Answer these questions to calculate your bleeding risk while on anticoagulants
Why Blood Thinners Can Be Dangerous - And How to Stay Safe
If you’re on a blood thinner, you’re not just taking a pill to prevent a stroke or clot. You’re walking a tightrope. One wrong move - a fall, a drug interaction, a missed lab test - and you could bleed internally without warning. Anticoagulants save lives, but they also cause over 150,000 emergency room visits in the U.S. every year, according to the American College of Cardiology. The goal isn’t just to take them. It’s to take them safely.
What Are Blood Thinners, Really?
Anticoagulants don’t actually thin your blood. They slow down the clotting process. That’s why they work for conditions like atrial fibrillation, deep vein thrombosis, and mechanical heart valves. But that same mechanism is what makes bleeding so dangerous.
There are three main types:
- Warfarin - The old-school option. Works by blocking vitamin K. Needs regular INR blood tests to keep your level between 2.0 and 3.0. Too low? Risk of clot. Too high? Risk of bleeding.
- DOACs - Dabigatran, rivaroxaban, apixaban, edoxaban. Newer, easier to use. No daily INR checks. But they’re harder to reverse if you bleed.
- Heparins - Used in hospitals or for short-term treatment. Enoxaparin (Lovenox) is common for home use. Can cause a rare but serious condition called heparin-induced thrombocytopenia (HIT).
Apixaban stands out. In the ARISTOTLE trial, it caused 31% fewer major bleeds than warfarin. That’s why it’s now the most prescribed DOAC in the U.S.
Who’s at Highest Risk for Bleeding?
Not everyone on blood thinners bleeds. But some people are far more vulnerable.
- People over 75 - Bleeding risk doubles or triples after age 75.
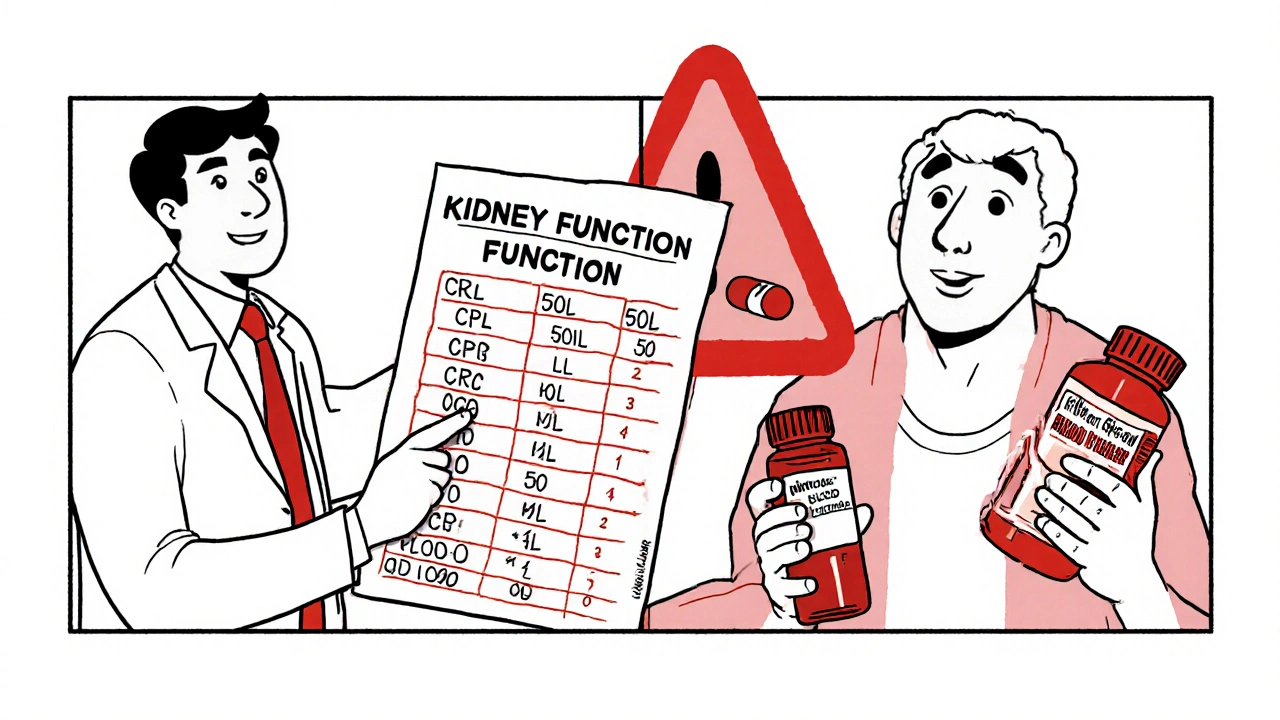
- Those with kidney problems - CrCl below 50 mL/min doubles major bleeding risk. DOACs are cleared by the kidneys. If your kidneys are weak, the drug builds up.
- People on other blood-thinning meds - Taking aspirin, clopidogrel, or NSAIDs like ibuprofen with a blood thinner? Your bleeding risk jumps 50-70%.
- Those with a history of bleeding - If you’ve had a GI bleed or brain bleed before, you’re more likely to have another.
Renal function matters more than you think. Apixaban requires a lower dose if your CrCl is below 25 mL/min. Rivaroxaban needs adjustment below 50 mL/min. If your doctor didn’t check your kidney function before prescribing, ask for it.
How to Prevent Bleeding - Practical Steps
Preventing hemorrhage isn’t about avoiding all risk. It’s about reducing avoidable mistakes.
- Know your INR (if on warfarin) - Keep your INR between 2.0 and 3.0. If it’s below 2.0, you’re not protected from clots. Above 3.0? Bleeding risk climbs fast. Aim for a Time in Therapeutic Range (TTR) above 70%. Each 10% drop in TTR raises bleeding risk by 15%.
- Check kidney function every 3-6 months - Even if you feel fine. DOACs aren’t harmless just because they don’t need daily blood tests. Kidney function declines slowly. By the time you feel symptoms, it’s too late.
- Avoid NSAIDs like ibuprofen and naproxen - Use acetaminophen (Tylenol) for pain instead. NSAIDs irritate your stomach lining and make bleeding more likely.
- Don’t combine with other anticoagulants or antiplatelets - No aspirin unless your doctor specifically says so. No clopidogrel unless you’ve had a stent and your cardiologist says it’s necessary.
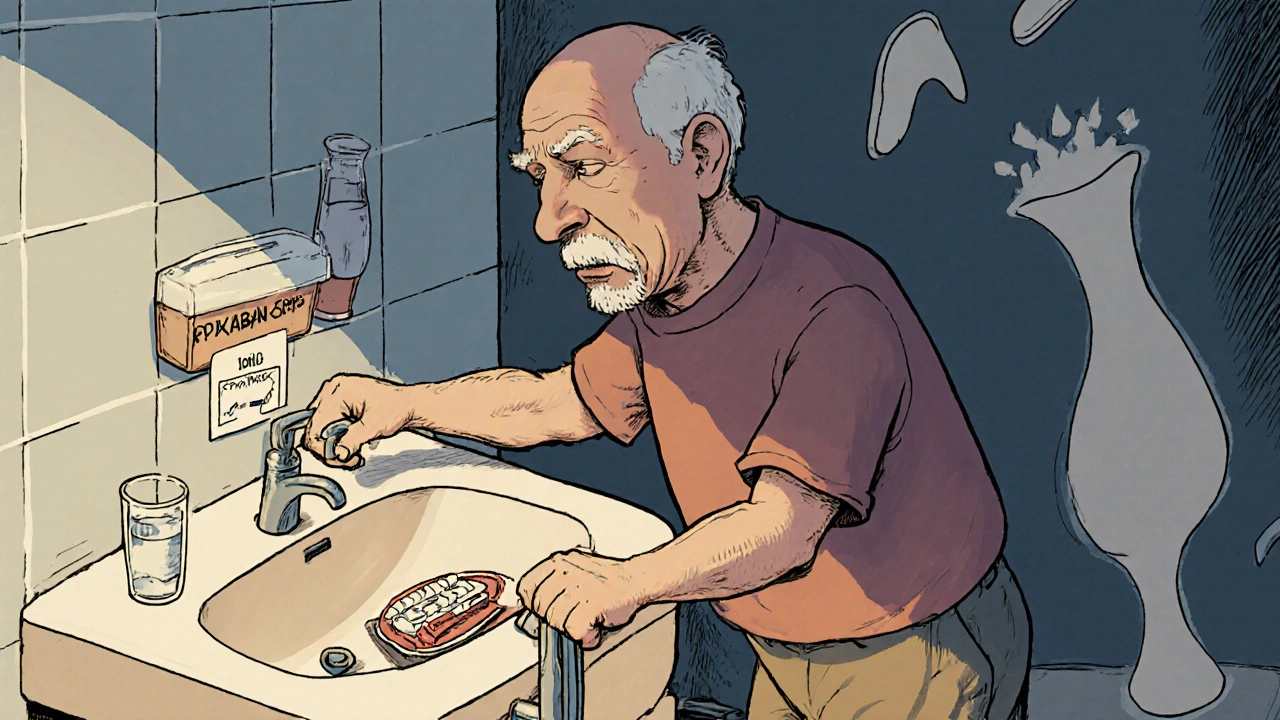
- Use a pill organizer - Dosing errors are common in older adults. Missing a dose increases clot risk. Taking two doses by accident? That’s a bleeding emergency.
- Be careful with falls - Use grab bars in the shower. Remove throw rugs. Wear non-slip shoes. A simple fall can cause a brain bleed or internal bleeding you won’t feel until it’s too late.
What to Do If You Bleed
Minor bleeding - like a nosebleed or small cut - usually stops on its own. But major bleeding needs immediate action.
Signs of major bleeding:
- Bleeding that won’t stop after 10 minutes of pressure
- Bright red or black, tarry stools
- Vomiting blood or material that looks like coffee grounds
- Sudden severe headache, dizziness, confusion - could be brain bleed
- Unexplained swelling or pain in joints or muscles
- Unusual bruising, especially without injury
If you suspect major bleeding, call emergency services. Don’t wait. Time matters.
Here’s what doctors do:
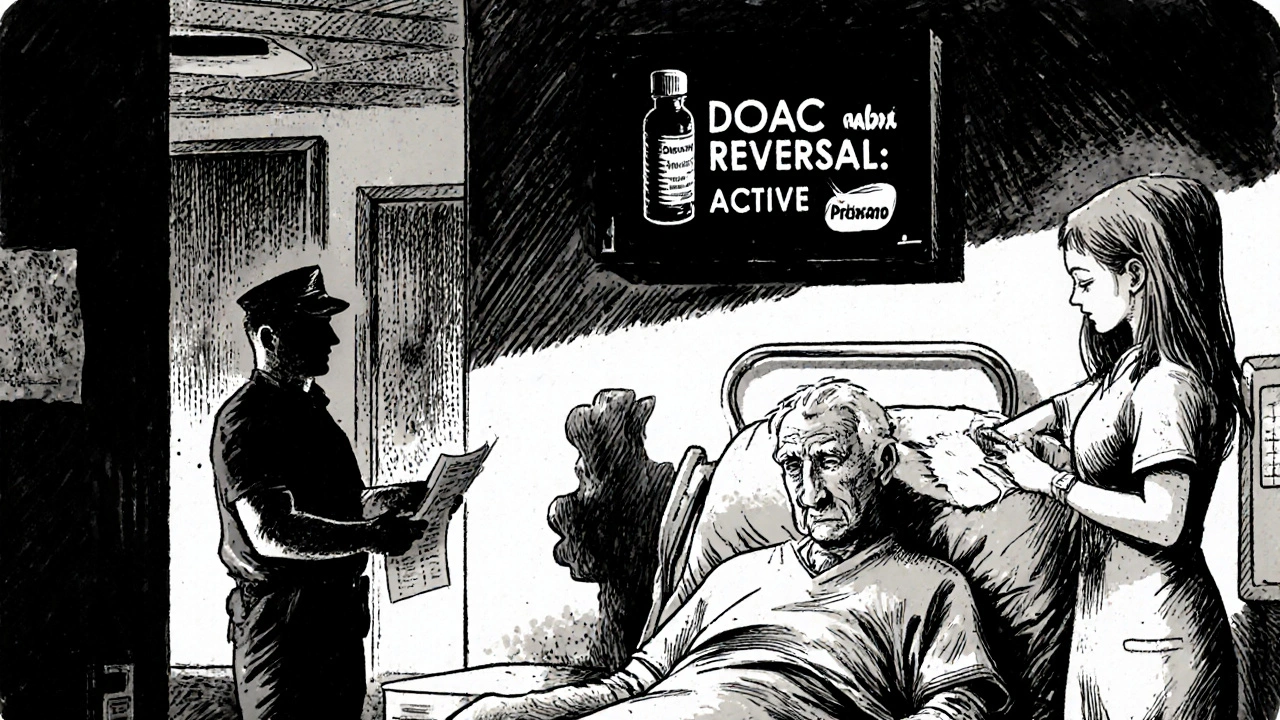
- For warfarin - Give 4f-PCC (four-factor prothrombin complex concentrate). It fixes your INR in 15 minutes. Vitamin K helps too, but it takes hours.
- For dabigatran - Idarucizumab (Praxbind). It’s a specific antidote. Works in minutes.
- For apixaban, rivaroxaban, edoxaban - Andexanet alfa (Andexxa). It reverses factor Xa inhibitors. But it costs around $13,000 per dose and isn’t available everywhere.
- For heparin - Protamine sulfate. Only works on unfractionated heparin, not Lovenox.
Most hospitals now have reversal kits ready. But if you’re on a DOAC, make sure your doctor knows which one you’re taking - and has the contact info for the nearest hospital that carries the antidote.
When to Restart After a Bleed
Many people stop their blood thinner after a bleed - and that’s often the wrong choice.
The American College of Cardiology says: restart as soon as it’s safe. Stopping increases your risk of stroke or pulmonary embolism more than continuing does.
Here’s the rule:
- Low risk of clot - If you have atrial fibrillation with a CHA₂DS₂-VASc score under 2-3, or a provoked DVT that happened more than 3 months ago - you might stop permanently.
- High risk of clot - If you have a mechanical heart valve, antiphospholipid syndrome, or unprovoked DVT - restart within days to weeks, even after a serious bleed.
Studies show that restarting anticoagulation after a GI bleed, for example, cuts the risk of death by nearly 50% compared to stopping.
The Future: Better Tools, Fewer Bleeds
There’s progress on the horizon.
- Ciraparantag - A universal reversal agent in trials. Could reverse all DOACs and heparins with one drug.
- Point-of-care DOAC tests - Like an INR machine for apixaban or rivaroxaban. Doctors could check levels in minutes, not days.
- AI risk predictors - New algorithms combine age, kidney function, medications, and history to predict bleeding risk better than old scoring systems.
These tools won’t eliminate risk - but they’ll make it easier to manage.
Bottom Line: You Can Be Safe on Blood Thinners
Anticoagulants are powerful. They’re not just pills. They’re tools that require attention, monitoring, and respect.
Don’t assume your doctor knows everything. Ask:
- “What’s my bleeding risk based on my kidneys and age?”
- “Do I really need this drug, or is there a safer option?”
- “What do I do if I fall or start bleeding?”
- “When should I come back for a blood test?”
Most people on blood thinners live long, healthy lives. But only if they treat the medication like the high-risk tool it is - not like a simple daily pill.
Can I take ibuprofen while on a blood thinner?
No. Ibuprofen, naproxen, and other NSAIDs increase your risk of stomach bleeding by 50-70% when taken with anticoagulants. Use acetaminophen (Tylenol) instead for pain or fever. Always check with your doctor before taking any new medication, even over-the-counter ones.
Do DOACs require blood tests like warfarin?
No, DOACs don’t need daily or weekly INR tests. But you still need kidney function tests (CrCl) every 3-6 months. If your kidneys weaken, the drug can build up and increase bleeding risk. Some doctors check kidney function more often in older adults or those with existing kidney disease.
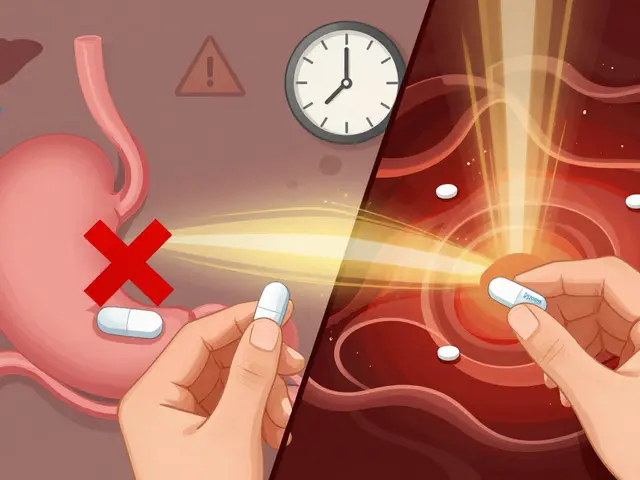
What if I miss a dose of my blood thinner?
If you miss one dose, take it as soon as you remember - but only if it’s within 6-12 hours of your usual time. If it’s been longer, skip the missed dose and take your next one at the regular time. Never double up. Missing doses increases clot risk. Taking two doses at once increases bleeding risk.
Can I drink alcohol while on anticoagulants?
Moderate alcohol is usually okay - one drink a day for women, two for men. But heavy drinking increases bleeding risk and can interfere with warfarin’s effectiveness. If you drink regularly, tell your doctor. Alcohol can also worsen liver and kidney function, which affects how your body processes blood thinners.
Is apixaban safer than warfarin?
Yes, for most people. Apixaban causes 31% fewer major bleeds than warfarin, based on the ARISTOTLE trial. It also has fewer food and drug interactions. But it’s not safer for everyone. If you have a mechanical mitral valve or antiphospholipid syndrome, warfarin is still the best choice. DOACs can increase clot risk in these cases.
What should I do if I need surgery or a dental procedure?
Never stop your blood thinner without talking to your doctor. For minor procedures like tooth extractions, you usually don’t need to stop. For major surgery, your doctor may pause it for a few days and use a short-acting heparin bridge. The decision depends on your clot risk, the type of procedure, and which anticoagulant you’re on.
Can I get a flu shot or other vaccines while on anticoagulants?
Yes. Vaccines are safe. Use a fine needle and apply pressure for 5-10 minutes after the shot to prevent bruising. Avoid intramuscular shots if possible - subcutaneous or intradermal routes are preferred. Always tell the provider you’re on a blood thinner.
Why is warfarin still used if DOACs are safer?
Warfarin is still first-line for three conditions: mechanical heart valves (especially mitral), antiphospholipid syndrome, and severe kidney failure (CrCl <15 mL/min). DOACs have been shown to cause more clots in these cases. Warfarin is also much cheaper - about $4 a month versus $550 for apixaban - making it necessary for people without good insurance.
Next Steps: What You Should Do Today
- Check your latest kidney function test (CrCl). If it’s over 6 months old, call your doctor to schedule one.
- Review your medication list. Are you taking NSAIDs, aspirin, or other blood thinners? Talk to your doctor about removing them.
- Make a bleeding emergency plan. Know your reversal agents. Keep a list of your medications and doses in your wallet or phone.
- Ask your doctor: “Based on my age, kidneys, and history, am I on the safest blood thinner for me?”
Anticoagulants don’t have to be a gamble. With the right knowledge and habits, you can live safely with them - and avoid the bleeding that so many others fear.
15 Comments
Jessica Healey
November 18, 2025 at 15:18 PM
I'm on apixaban and honestly? I forgot my dose last week and just skipped it. My doctor said not to double up but I was like...eh. Now I'm paranoid every time I sneeze. Why does this feel like playing Russian roulette with my organs?
Holli Yancey
November 19, 2025 at 15:54 PM
I appreciate the depth here. As someone with CKD stage 3, I've had to adjust my meds twice because my CrCl dropped. It's scary how slowly kidney function declines. I didn't feel different until my INR spiked. Now I get labs every 90 days like clockwork. Small steps save lives.
Gordon Mcdonough
November 20, 2025 at 01:25 AM
I'm a veteran and I've been on warfarin since 2018 after a PE. The VA doesn't give a damn about TTR. I've had INRs of 1.8 and 4.2 in the same month. They don't even call you back. I had to learn this stuff on my own. I'm tired of being treated like a number. And don't get me started on the cost of Andexxa-my VA pharmacy says "it's not in stock" like it's a damn luxury perfume.
saurabh lamba
November 21, 2025 at 03:06 AM
We are all just meat bags with blood inside... and the pharmaceutical industry sells us fear wrapped in pills. Why do we trust chemicals more than our own bodies? Maybe the real bleeding disorder is our faith in modern medicine. 🤔
Kelsey Robertson
November 21, 2025 at 04:10 AM
Let me just say-this post is dangerously oversimplified. Apixaban isn't "safer" for everyone. It's just cheaper for insurers. And who says kidney function is the real issue? What about gut microbiome? Liver metabolism? The fact that we ignore epigenetics in anticoagulant management is criminal. This is basic biochemistry 101, not cutting-edge medicine.
Eric Healy
November 22, 2025 at 12:02 PM
I'm a nurse and I see this every day. People think DOACs are magic. They're not. One guy took 2 doses of rivaroxaban because he "forgot if he already took it." Blew out his spleen. No joke. And no one ever asks about alcohol. One glass of wine? Fine. Two? You're asking for a bleed. And don't even get me started on turmeric supplements. "It's natural!" Yeah, and cyanide is natural too.
Joseph Townsend
November 24, 2025 at 10:33 AM
I just got diagnosed with AFib and my cardiologist handed me a script for apixaban like it was a Starbucks gift card. I Googled "what happens if I fall on my head?" and ended up in a Reddit thread that made me cry. I'm 68. I don't want to die because I slipped in the shower. I just want to live. Someone please tell me what to do.
Sridhar Suvarna
November 24, 2025 at 10:45 AM
In India, we don't have access to reversal agents like Praxbind or Andexxa. Many patients stop their anticoagulants after minor bleeding because hospitals can't afford the antidote. We need low-cost, scalable solutions. Telemedicine for INR monitoring? Mobile labs? This isn't just a medical problem-it's a global equity issue.
Deb McLachlin
November 24, 2025 at 13:36 PM
The emphasis on renal function is spot-on. I had a patient last month-82, on rivaroxaban, no recent labs. CrCl was 28. She was having epistaxis daily. We switched to apixaban 2.5mg BID and her bleeding stopped within a week. The system fails when we assume "no INR monitoring = no monitoring." We need proactive kidney tracking, not reactive crisis management.
Joseph Peel
November 26, 2025 at 04:25 AM
I'm a retired pharmacist from Texas. I've seen it all. Warfarin patients with kale smoothies, DOAC users taking St. John's Wort, people mixing Tylenol with alcohol like it's a cocktail. The real tragedy isn't the bleeding-it's the ignorance. Knowledge is the only true anticoagulant.
Bill Machi
November 26, 2025 at 04:37 AM
This is why America's healthcare system is broken. You need a PhD to understand your own meds. A 70-year-old widow on warfarin gets a letter saying "INR is 4.1, call your doctor." She doesn't know what INR means. She can't afford the copay. She doesn't have transportation. And now she's bleeding internally while waiting for a callback. This isn't medicine-it's a lottery.
Levi Hobbs
November 26, 2025 at 13:06 PM
I just want to say thank you for writing this. My mom was on warfarin for 12 years. We had a color-coded pill organizer, weekly INR logs, and a binder with all her meds. It was exhausting. But she lived to 89. This isn't just about pills-it's about systems, habits, and love. Don't underestimate the power of a checklist.
henry mariono
November 27, 2025 at 11:13 AM
I'm on apixaban. I take it at 8pm. I don't miss a day. I don't take NSAIDs. I use a cane. I got a fall alarm for my shower. I don't need to shout about it. I just live quietly, carefully. And that's enough.
Bill Machi
November 28, 2025 at 12:43 PM
And yet, here we are. People still think "natural remedies" are safer. Garlic. Ginger. Ginkgo. You're not being holistic-you're being reckless. If you're on a blood thinner, your kitchen is now a minefield. Stop pretending you're a wellness influencer and start treating your meds like your life depends on it-because it does.





Shannon Hale
November 18, 2025 at 04:29 AM
This is the most terrifyingly accurate breakdown of anticoagulant risks I've ever read. I'm not even on blood thinners and I'm sweating. NSAIDs? Don't even think about it. I had a cousin who took ibuprofen with warfarin and ended up in the ICU with a GI bleed. No one told him. No one. And now he's on a feeding tube. This isn't just medical advice-it's a survival guide.