Sub-potent Drugs: What They Are, Why They Matter, and Which Medications Fall Into This Category
When a drug doesn’t deliver the expected effect, it’s not always because you’re resistant to it—it might be sub-potent drugs, medications that fall below the minimum strength needed to produce a reliable therapeutic effect. Also known as under-dosed or subtherapeutic drugs, these are pills or injections that, for reasons ranging from manufacturing errors to poor storage, simply don’t contain enough active ingredient to do their job. This isn’t rare. In fact, the FDA has flagged dozens of generic drugs over the past decade for potency issues, especially in narrow therapeutic index drugs, medications where even tiny changes in dosage can lead to treatment failure or serious toxicity. Think lithium, warfarin, or thyroid meds. If these drugs are sub-potent, you’re not just wasting your time—you’re risking your life.
Why does this happen? Sometimes it’s supply chain problems—raw materials degrade during transport. Other times, it’s cost-cutting at factories that skip proper quality checks. And because generic drugs are allowed to vary by ±10% in potency compared to brand-name versions, a sub-potent version can slip through unnoticed until someone gets sick. Patients on anticoagulants, blood thinners that require precise dosing to prevent clots without causing bleeding or DMARDs, disease-modifying drugs used for autoimmune conditions like rheumatoid arthritis, are especially vulnerable. A slight drop in potency can mean your immune system starts attacking your joints again, or a clot forms in your heart. You won’t feel it right away. But over weeks or months, the damage adds up.
It’s not just about strength. Sub-potent drugs often come with hidden risks—like when a weak version of a drug causes your body to adapt, making it harder to respond later when you get a properly dosed pill. That’s why regulators like the FDA and EMA require tighter bioequivalence standards for these drugs. But not every country enforces them equally. If you’re buying meds online or from unfamiliar pharmacies, you’re playing Russian roulette with your health. The good news? You can protect yourself. Check your pill’s appearance, track how you feel after switching brands, and ask your pharmacist if your generic is from a trusted manufacturer. If your blood pressure stays high despite taking your meds, or your mood swings return on lithium, potency could be the issue—not your body.
What you’ll find below is a collection of real cases where drug potency made the difference between healing and harm. From lithium toxicity caused by interactions to statins that failed to lower cholesterol, these stories aren’t hypothetical—they’re happening to people right now. You’ll learn which drugs are most at risk, how to spot a weak pill, and what steps to take before your next refill. This isn’t about fear. It’s about control. Your medicine should work. It should be strong enough. And you deserve to know when it’s not.

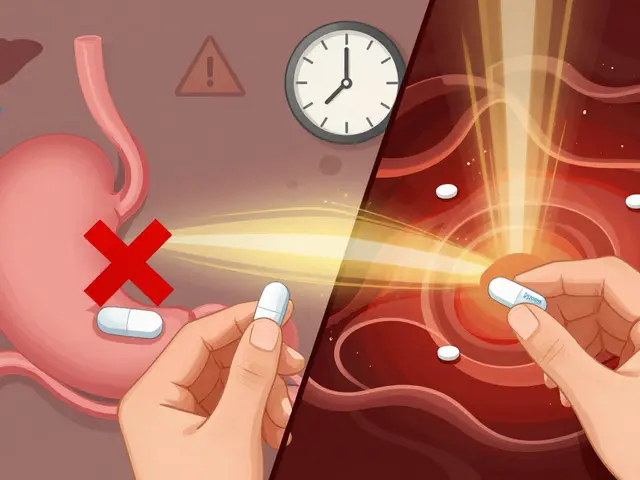
Emergency Use of Sub-Potent Expired Medications: When It’s Safe and When It’s Not
Most expired medications are still safe and effective years past their date-but not all. Learn which drugs you can use in an emergency, which ones to avoid, and how to tell if they’re still good.
View More