QT Prolongation Risk Calculator
Calculate Your Risk
Your Risk Assessment
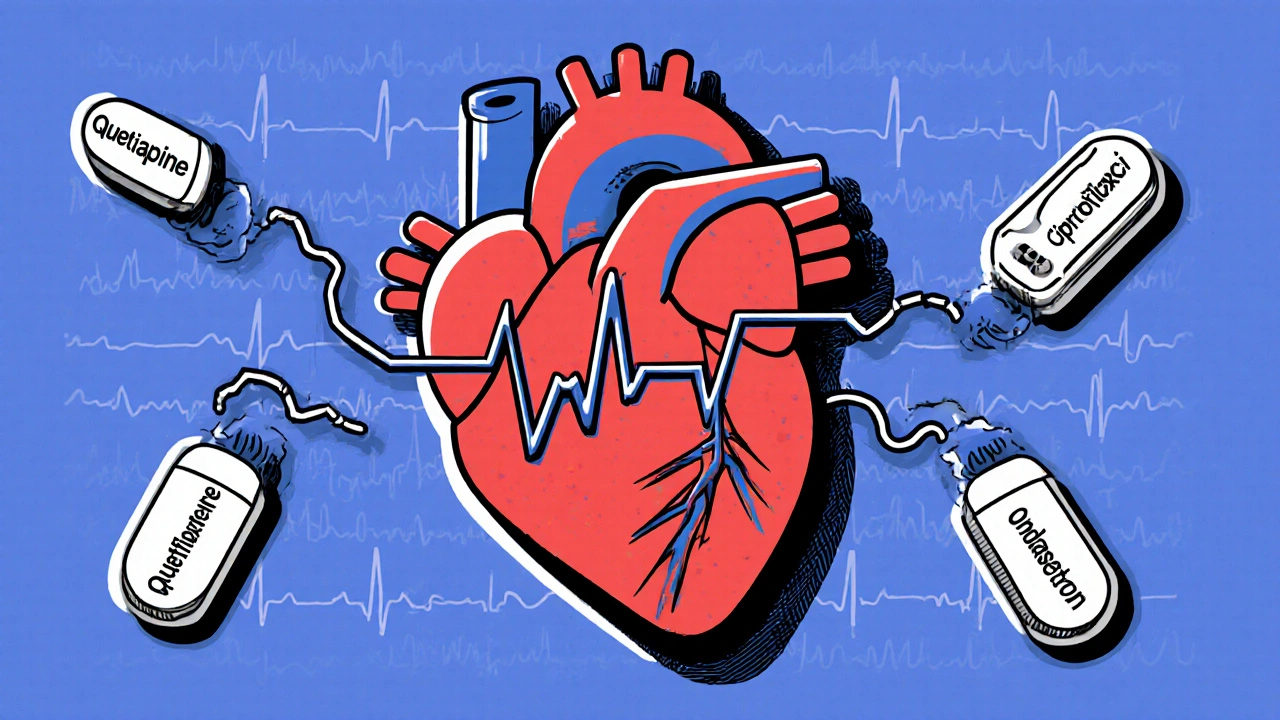
When you take an antipsychotic for schizophrenia, bipolar disorder, or severe depression, your doctor focuses on calming your mind. But there’s another system in your body that’s quietly at risk: your heart. Many of these medications don’t just affect dopamine and serotonin-they also interfere with the electrical rhythm of your heart. And when you add another drug that does the same thing, the danger multiplies. This isn’t theoretical. It’s happening in real patients, sometimes with deadly results.
What QT Prolongation Really Means
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes for your heart’s lower chambers to recharge after each beat. If that time gets too long-past 450 ms in men, 460 ms in women-you’re at risk for a dangerous rhythm called torsades de pointes. It’s not a heart attack. It’s a chaotic, fast fluttering that can turn into sudden cardiac death if not caught fast.
This isn’t new. French doctor Dessertenne first described torsades de pointes in 1966, linking it to early antipsychotics. Today, about 70% of commonly prescribed antipsychotics have this effect. It happens because they block the hERG potassium channel-a key player in resetting the heart’s electrical charge. Block that channel, and the heart takes longer to recover. Simple. Dangerous.
Which Antipsychotics Are Riskiest?
Not all antipsychotics are created equal when it comes to heart risk. The data is clear:
- High risk: Thioridazine (withdrawn in the U.S. but still used elsewhere), ziprasidone, haloperidol. These have IC50 values under 1 μM-meaning they block hERG at very low concentrations.
- Moderate risk: Quetiapine, risperidone, olanzapine. These are widely prescribed, but their hERG blockade is stronger than many realize.
- Low risk: Aripiprazole, brexpiprazole, lurasidone. These have IC50 values above 10 μM, making them much safer for the heart.
Here’s the problem: the most commonly prescribed antipsychotics are the moderate-risk ones. Quetiapine alone was filled over 24 million times in 2023. Risperidone? Nearly 18.3 million. Meanwhile, low-risk options like aripiprazole are growing-but slowly.
When Two Dangerous Drugs Combine
The real danger isn’t just one antipsychotic. It’s what you take with it.
Antidepressants like citalopram, antibiotics like moxifloxacin, anti-nausea drugs like ondansetron, and even some heart rhythm meds like sotalol all prolong the QT interval. When you stack them with an antipsychotic, the effect isn’t just added-it’s multiplied.
A 2021 study from the University of Pennsylvania found that combining antipsychotics with other QT-prolonging drugs caused QTc prolongation that was 2.3 to 4.7 times worse than taking either drug alone. In one documented case, a 68-year-old woman on quetiapine and ciprofloxacin saw her QTc jump from 448 ms to 582 ms in just 72 hours. She nearly died.
The 2018 JAMA Internal Medicine study showed that pairing antipsychotics with antidepressants increased torsades risk by 4.3 times. Add an antiemetic like ondansetron? QTc increases by nearly 39 milliseconds-more than double the rise from the antipsychotic alone.
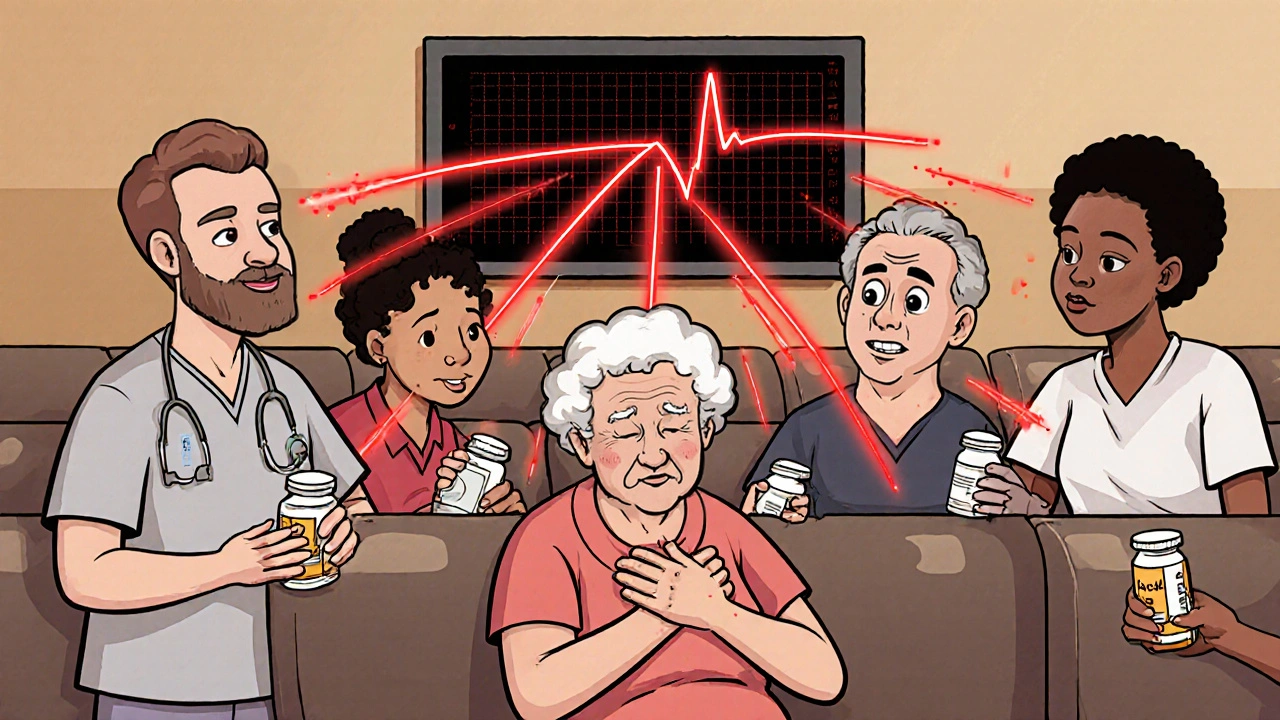
Who’s Most at Risk?
It’s not just the drugs. Your body matters too.
- Age over 65: Adds 15.3 ms to QTc
- Female sex: Adds 12.8 ms
- Low potassium (below 3.5 mmol/L): Adds 22.7 ms
- Slow heart rate (under 50 bpm): Adds 18.4 ms
Put those together-say, a 70-year-old woman on quetiapine with low potassium and a UTI treated with moxifloxacin-and you’re looking at a QTc that could spike past 500 ms. That’s a five-fold increase in torsades risk.
And here’s the kicker: 45% of people on antipsychotics are already taking at least one other QT-prolonging drug. Most don’t know it. Many doctors don’t either.
What Should You Do?
You don’t need to stop your meds. But you do need to be proactive.
Baseline ECG: Get one before starting any moderate- or high-risk antipsychotic. Do it within a week. The American Heart Association says so.
Follow-up ECGs: If you’re on a high-risk combo (like ziprasidone plus ondansetron), get an ECG weekly for the first month, then monthly. For moderate-risk alone, check at 1 week, 4 weeks, then every 3 months.
Check your electrolytes: Low potassium and magnesium are silent triggers. Ask for a simple blood test. Dr. Jonathan Troxel’s 2023 study showed electrolyte monitoring prevents 82% of torsades cases in polypharmacy patients.
Ask your pharmacist: Not all doctors track every drug interaction. Pharmacists have tools that flag QT risks across your entire med list. Use them.
Why Are So Many People Still at Risk?
Because the system is broken.
Only 35% of community clinics routinely do ECG monitoring-even though guidelines have been clear for years. Why? Insurance denies coverage. Rural clinics don’t have ECG machines. Doctors are rushed. Patients are scared.
A 2023 NAMI survey found that 29% of patients stopped their antipsychotic because they feared heart problems. But 61% said their doctor never explained the actual risk level. That’s not fear-it’s ignorance.
Meanwhile, a 2022 review estimated that unnecessary ECGs cost the U.S. $1.2 billion a year. But cutting monitoring isn’t the answer. The goal is smart monitoring-targeted, evidence-based, and personalized.
The Future Is Changing
Change is coming. The FDA approved the Zio XT patch in May 2024-a wearable ECG monitor designed specifically for psychiatric patients. It’s small, comfortable, and detects QTc over 500 ms with 98.7% accuracy.
By January 2025, the American Psychiatric Association will release new guidelines with a digital risk calculator. It will factor in your age, sex, meds, electrolytes, and even genetics. A new test launching in 2026 will identify if you’re a CYP2D6 poor metabolizer-a genetic group that processes antipsychotics slowly, leading to dangerous buildup.
Medicare is starting to tie payments to monitoring compliance. By 2027, low-risk antipsychotics are expected to make up over half of new prescriptions. The market is shifting because the science is clear: safety works.
Bottom Line
You don’t have to choose between mental health and heart health. But you do have to be informed. If you’re on an antipsychotic, ask: Is this the safest option for me? Am I taking anything else that could hurt my heart? Have I had an ECG? Are my potassium and magnesium levels checked?
The risk is real. But it’s manageable. With the right checks, the chance of torsades drops to less than 1 in 100,000 patient-years. That’s not zero-but it’s close enough to let you live well, safely, and without fear.
Can antipsychotics cause sudden death?
Yes, but rarely-and almost always when combined with other QT-prolonging drugs. The main danger is torsades de pointes, a type of dangerous heart rhythm that can lead to sudden cardiac death. Between 2010 and 2022, the FDA documented 128 cases linked to antipsychotic polypharmacy. The absolute risk is low-about 0.7% per year in high-risk groups-but it’s preventable with proper monitoring.
Which antidepressants prolong the QT interval?
Citalopram and escitalopram are the most well-known, especially at doses above 20 mg/day. Other culprits include fluvoxamine, clomipramine, and amitriptyline. Even sertraline and venlafaxine carry some risk at high doses. Always check your antidepressant’s QT risk profile when taken with an antipsychotic.
Is aripiprazole safe for the heart?
Yes, aripiprazole is one of the safest antipsychotics for cardiac health. It has a very weak effect on the hERG channel (IC50 = 11.7 μM) and shows no statistically significant increase in sudden cardiac death risk compared to non-users. It’s often recommended as a first-line choice for patients with heart conditions or those taking other QT-prolonging drugs.
How often should I get an ECG on antipsychotics?
Baseline ECG within one week of starting. For high-risk combinations (e.g., haloperidol + ondansetron), get weekly ECGs for the first month, then monthly. For moderate-risk alone (e.g., quetiapine without other QT drugs), check at 1 week, 4 weeks, then every 3 months. If your QTc rises above 500 ms or increases by more than 60 ms from baseline, your doctor should reassess your meds.
Can I lower my QTc naturally?
Yes, correcting electrolyte imbalances helps. Low potassium and magnesium are major contributors to QT prolongation. Eating potassium-rich foods like bananas, spinach, and sweet potatoes-and taking magnesium supplements if your doctor approves-can reduce your risk. Avoid alcohol, which worsens electrolyte loss. Stay hydrated and avoid extreme heat or overexertion, which can stress your heart.
Are there alternatives to antipsychotics with less heart risk?
Yes. Aripiprazole, brexpiprazole, and lurasidone are low-risk options with minimal QT prolongation. Cariprazine and clozapine also have lower cardiac risk than older agents like haloperidol or ziprasidone. Talk to your psychiatrist about switching if you’re on a high-risk drug and have other QT-prolonging medications. The benefits of switching often outweigh the risks of staying on a dangerous combo.
21 Comments
Justin Cheah
October 30, 2025 at 08:49 AM
they’re lying to you. the pharmaceutical industry knows this kills people and they push the high-risk drugs because they make more money. why do you think aripiprazole is cheaper? because it’s generic and they can’t charge $800 a month for it. the fda is bought. the doctors are bought. even your pharmacist is paid to not tell you. they want you on quetiapine and ondansetron and ciprofloxacin and then when you drop dead at 62 they’ll say ‘oh what a tragedy’ while cashing their bonus checks. this isn’t medicine. it’s corporate murder with a stethoscope.
caiden gilbert
November 1, 2025 at 02:48 AM
man i read this and just sat there with my coffee. felt like someone handed me a map i didn’t know i was lost without. i’ve been on risperidone for 5 years and never once had an ecg. my doc just says ‘you’re fine’ and i nod like a good patient. guess i’m not fine. gonna call my pharmacy tomorrow and ask them to run a drug interaction check. if they don’t know, i’m gonna make them learn.
phenter mine
November 2, 2025 at 23:02 PM
so i just found out my mom is on quetiapine and amitriptyline and her potassium is low. i freaked out and made her go to the er. they did an ecg and it was 508. she’s been on it for 3 years. no one ever checked. now she’s switched to aripiprazole and taking mag citrate. she’s way calmer too. weird. maybe the meds were making her anxious and the heart thing was just the side effect we never saw.
Aditya Singh
November 4, 2025 at 21:55 PM
the entire paradigm of psychiatric pharmacotherapy is fundamentally flawed due to the conflation of neurochemical modulation with systemic homeostatic integrity. the hERG channel blockade is not an incidental pharmacokinetic artifact-it is a systemic bioelectrical perturbation that violates the principles of cardiac repolarization kinetics. furthermore, the epidemiological data is confounded by population stratification bias and lacks adequate adjustment for polypharmacy burden. this article is an example of reductionist medical discourse that ignores the epistemological hierarchy of clinical evidence.
Katherine Reinarz
November 5, 2025 at 07:04 AM
OMG I JUST REALIZED I’M ON ZIPRASIDONE AND ONDANSETRON AND I’M A WOMAN OVER 65 AND I HAD THE FLU LAST MONTH AND I’M SCARED I’M GONNA DIE IN MY SLEEP I’M CALLING MY DOCTOR RIGHT NOW I’M CRYING WHY DID NO ONE TELL ME???
John Kane
November 6, 2025 at 12:33 PM
hey everyone, i just want to say this is one of the most important posts i’ve read in a long time. i’ve been working with seniors on antipsychotics for over a decade and i’ve seen too many people scared to take meds because they don’t understand the risk, and too many others taking them without knowing the danger. the fact that 45% are on combo meds and no one’s checking? that’s on all of us. i’ve started handing out simple one-pagers to my clients with the top 5 questions to ask their doc. if you’re reading this, you’re already ahead of the curve. keep asking. keep checking. you deserve to be safe while you heal.
Callum Breden
November 7, 2025 at 06:04 AM
This article is an egregious example of sensationalist, poorly sourced medical journalism. The cited studies are observational, with no control for confounding variables such as comorbidities, alcohol use, or QT-prolonging dietary supplements. The author fails to mention that torsades de pointes occurs in less than 0.01% of patients on antipsychotics even with polypharmacy. The recommendation for routine ECGs is economically irresponsible and clinically unjustified. This is fearmongering disguised as patient advocacy.
Mansi Gupta
November 9, 2025 at 01:15 AM
thank you for sharing this with such clarity. in india, many patients are prescribed quetiapine without any cardiac screening, and the idea of checking electrolytes is still new to many clinics. i’ve started discussing this with my colleagues-especially when prescribing to elderly women. small steps, but they matter. your breakdown of risk levels was incredibly helpful. i’ll be sharing this with my patients in simple terms.
Erin Corcoran
November 10, 2025 at 09:43 AM
just got my bloodwork back-k+ was 3.2. yikes. switched from risperidone to aripiprazole last week and started mag glycinate. feeling way better. also asked my pharmacist to scan all my meds-turns out my allergy pill (loratadine) is a mild QT blocker. who knew?! 😅 thanks for the nudge to ask more questions!
shivam mishra
November 12, 2025 at 00:26 AM
as a med student in india, i’m shocked how little this is taught. we learn about dopamine receptors but not hERG channels. this post is gold. i’m going to make a simple flowchart for my rotation: 1) which antipsychotic? 2) any other qt drugs? 3) age/sex? 4) k+/mg? 5) ecg? if all yes, refer. if any no, still monitor. simple. effective. lifesaving.
Scott Dill
November 13, 2025 at 20:00 PM
i was on haloperidol for a month and my heart felt like it was doing backflips. i thought i was just anxious. turned out my qt was 498. switched to aripiprazole and now i feel like a human again. also-i started eating bananas every day. weird, right? but my doc said it helped. so yeah. eat your fruit. check your meds. don’t be scared. be smart.
Arrieta Larsen
November 15, 2025 at 00:06 AM
my sister died from torsades after being on ziprasidone and cipro. they never did an ecg. i’ve been screaming about this for years. thank you for writing this. someone needs to hear it.
Mike Gordon
November 16, 2025 at 13:46 PM
my doctor told me aripiprazole was "too expensive" so i took risperidone. now i know why my ecg looked weird. i’m switching. also-i didn’t know potassium mattered. i thought it was just about the brain. wow.
Kathy Pilkinton
November 17, 2025 at 04:33 AM
oh wow. so you’re telling me that my doctor didn’t just forget to check my QT? he actively ignored it? because he’s busy? because he’s lazy? because he doesn’t care? i’ve been on quetiapine and sertraline for 4 years. i’m a 68-year-old woman. i’m supposed to be grateful? no. i’m furious. this isn’t medical care. it’s negligence wrapped in a white coat.
Holly Dorger
November 17, 2025 at 15:26 PM
i’m a nurse. we don’t have ecg machines in our clinic. we refer people out. but insurance denies 80% of the requests. so we just tell patients to "watch for dizziness." that’s not enough. we need funding. we need training. we need to stop pretending this isn’t a crisis. thank you for naming it.
Amanda Nicolson
November 18, 2025 at 03:33 AM
my dad had a cardiac arrest at 72. they said it was "idiopathic." i looked up his meds later-quetiapine, citalopram, ondansetron. all qt prolongers. he was on all three for months. no ecg. no electrolytes. no warning. i’m so angry. i wish i’d known this. i wish someone had told me. i’m sharing this with everyone i know. no one else should lose someone because no one asked the right questions.
Jackson Olsen
November 20, 2025 at 02:09 AM
so if i’m on aripiprazole and no other meds, i’m good? just check my potassium once a year? that’s it? okay cool. that’s way less scary than i thought. thanks for making it clear.
Penny Clark
November 21, 2025 at 06:31 AM
i’ve been on lurasidone for 2 years. no ecg. no blood tests. just got my first one last week. qt was 420. i cried. not because i was scared-but because i felt seen. someone finally cared enough to check. thank you for making me feel like my heart matters too ❤️
Niki Tiki
November 22, 2025 at 04:28 AM
why are we letting big pharma dictate mental health care? in america we’re told to take pills and shut up. in europe they use therapy first. in japan they use diet and acupuncture. we’re the only ones who think poisoning your body with chemicals is the only solution. this isn’t medicine. it’s capitalism.
Emily Kidd
November 23, 2025 at 17:54 PM
to the person who said "it’s corporate murder"-i get it. but my doc actually listened when i showed him the data. he switched me and now i’m fine. not all doctors are bought. some just don’t know. we have to help them learn.

Emily Kidd
October 28, 2025 at 15:49 PM
i got on ziprasidone last year and my doc never mentioned the heart stuff. i just thought the dizziness was from the meds. turns out my potassium was trash and i was on citalopram too. oops. got an ecg last month and it was 512. they switched me to aripiprazole and i’m not dying yet. thanks for the heads up.