
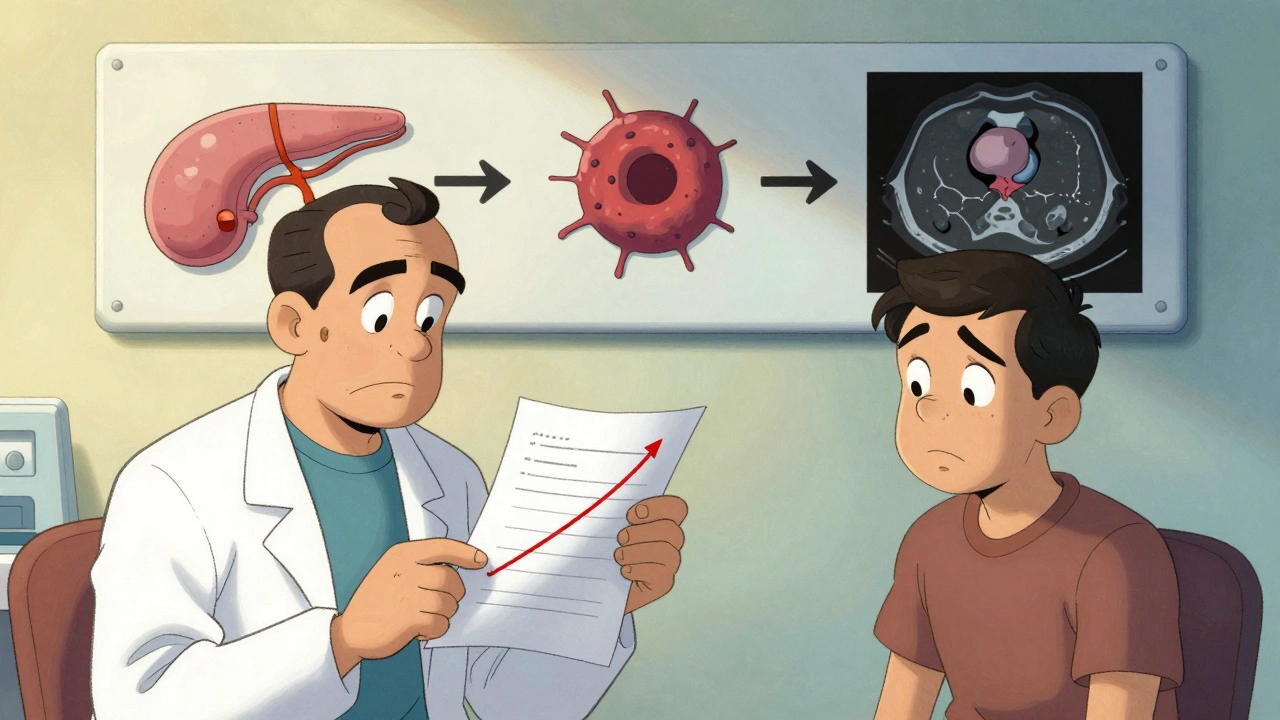
Most people don’t realize how sneaky pancreatic cancer can be. By the time symptoms show up, the cancer is often already advanced. That’s why it’s one of the deadliest cancers - only 12% of people survive five years after diagnosis. But here’s the thing: if caught early, that number jumps to 44%. The problem isn’t lack of progress. It’s lack of awareness. The signs are there, but they’re quiet. They look like something else. And too often, they’re ignored.
What Are the Early Signs You Can’t Afford to Ignore?
Pancreatic cancer doesn’t scream. It whispers. And those whispers are easy to dismiss. You’ve had a bad stomach, lost a few pounds, felt tired. Maybe you blamed stress, aging, or a bad diet. But when these symptoms stick around without a clear reason, it’s not normal.
Unexplained weight loss is one of the most common red flags. About 60% of patients lose significant weight without trying - even if they’re eating normally. It’s not just about appetite. The cancer interferes with digestion. Your body can’t absorb nutrients the way it should.
Then there’s jaundice. Yellow skin, yellow eyes, dark urine, pale stools. This happens when a tumor in the head of the pancreas blocks the bile duct. The bile backs up, turning your skin and eyes yellow. It’s not just a cosmetic issue - it’s a clear signal that something is wrong inside. And if you’re itching badly without a rash, that’s often part of it too. About 60% of people with jaundice from pancreatic cancer report severe itching.
Abdominal or back pain is another big one. It’s not sharp or sudden. It’s a dull, constant ache that wraps around your middle and goes into your back. It often gets worse after eating. Many patients are misdiagnosed with gallstones or IBS for months before the real cause is found.
Here’s one you might not expect: new-onset diabetes. If you’re over 50 and suddenly develop type 2 diabetes with no family history, no obesity, no clear reason - get checked. Research shows 80% of pancreatic cancer patients develop diabetes within 18 months before their diagnosis. Blood sugar levels that jump from normal (under 100 mg/dL) to diabetic (over 126 mg/dL) in just a few months are a major warning sign.
And then there’s the mental shift. Depression, anxiety, or a sudden loss of interest in life can appear months before physical symptoms. One study found that half of patients had psychiatric symptoms as their first sign. It’s not just "feeling down." It’s a deep, unexplained change in mood that doesn’t improve with usual support.
Why Is It So Hard to Catch Early?
The pancreas hides. It’s deep in your belly, behind the stomach. You can’t feel a tumor there with a physical exam. There’s no simple blood test like a mammogram or PSA. The only routine blood marker, CA 19-9, isn’t reliable for early stages. It’s only elevated in about 30-50% of early tumors.
Imaging helps, but only when the tumor is big enough. A CT scan can miss tumors smaller than 2 cm. That’s why most cases are found at stage III or IV - when the cancer has already spread to nearby organs or lymph nodes.
And here’s the catch: there’s no screening program for the general public. Unlike breast or colon cancer, you can’t just get a yearly test. Screening is only recommended for people with strong family history, inherited gene mutations like BRCA2, or chronic pancreatitis. That means most people are flying blind until symptoms become impossible to ignore.
What’s Changed in Treatment? Hope Is Growing
Twenty years ago, a diagnosis of advanced pancreatic cancer meant months to live. Today, some patients are surviving years - not just months. That’s thanks to smarter, more targeted treatments.
Surgery is still the only chance for a cure. The Whipple procedure removes part of the pancreas, the gallbladder, and part of the small intestine. It’s complex, but when the cancer hasn’t spread, it works. About 20-25% of patients who get this surgery live five years or longer.
But here’s the game-changer: neoadjuvant therapy. That means giving chemotherapy before surgery. In the past, doctors operated first, then treated. Now, they shrink the tumor with chemo first. The FOLFIRINOX combo - a mix of four drugs - has shown response rates of 58% in tumors that were once considered unsuitable for surgery. That means more people become candidates for removal.
For those with metastatic cancer, survival has doubled. The PRODIGE 24 trial showed patients on modified FOLFIRINOX lived nearly 4.5 years - more than double the 20 months seen with older treatments. That’s not a cure, but it’s a massive leap.
Targeted drugs are making a difference too. If your cancer has a BRCA gene mutation (about 5-7% of cases), olaparib - a drug originally for breast cancer - can keep the disease from spreading longer. And if your tumor has a rare mutation called MSI-H/dMMR (3-4% of cases), pembrolizumab, an immunotherapy, can shrink tumors in 40% of patients.
What’s on the Horizon? The Future Is in Detection
The real breakthrough won’t come from better chemo. It’ll come from catching the cancer before it spreads.
Researchers are working on blood tests that look for tumor DNA floating in the bloodstream. One test, called PancreaSeq, found 95% of early-stage cancers in high-risk people. Another, being tested in the DETECTA trial, uses protein markers and tumor DNA to spot cancer with 85% accuracy. These aren’t science fiction - they’re in clinical trials right now.
AI is helping too. Google’s LYNA algorithm can spot pancreatic cancer cells on tissue slides with 99.3% accuracy - better than many pathologists. Microbiome analysis is also showing promise. The bacteria in your gut change when pancreatic cancer develops. One 2023 study used stool samples to identify cancer with 80% accuracy.
And doctors are starting to pay attention to new-onset diabetes. If you’re over 50 and get diabetes out of nowhere, your doctor should consider a scan. Mayo Clinic and others are now testing protocols to screen these patients with MRI or ultrasound.

Who Should Be Screened?
You don’t need to be scared. But you should know if you’re at higher risk. Screening is recommended if you have:
- A first-degree relative (parent, sibling, child) with pancreatic cancer
- A known genetic mutation like BRCA1, BRCA2, Lynch syndrome, or PALB2
- Chronic pancreatitis that started young
- New-onset diabetes after age 50 with no other explanation
If any of these apply to you, talk to your doctor. You might qualify for annual MRI or endoscopic ultrasound. These aren’t perfect, but they’re the best tools we have right now.
What Can You Do Right Now?
Don’t wait for a diagnosis. Pay attention to your body.
- If you’ve lost weight without trying, get it checked - even if you feel fine.
- If your skin or eyes are yellowing, don’t assume it’s just fatigue. Get a bilirubin test.
- If you’re diabetic with no clear cause, ask about pancreatic screening.
- If you’ve been feeling depressed for months with no reason, mention it. It’s not "all in your head."
- If you have a family history, ask your doctor about genetic testing.
Early detection saves lives. It’s not about being paranoid. It’s about being informed. Pancreatic cancer is tough - but it’s not unbeatable. The tools to find it earlier are here. The treatments are better. What’s missing is the awareness to use them.
Can pancreatic cancer be cured?
Yes - but only if caught very early. Surgery to remove the tumor is the only potential cure, and it works best when the cancer hasn’t spread. About 20-25% of patients who undergo surgery for early-stage disease survive five years or longer. For those diagnosed after the cancer has spread, cure is rare, but treatment can extend life by years.
Is jaundice always a sign of pancreatic cancer?
No. Jaundice can be caused by liver disease, gallstones, or hepatitis. But when it appears with unexplained weight loss, new diabetes, or back pain, it becomes a major red flag for pancreatic cancer - especially in people over 50. If you have jaundice and no known liver condition, ask your doctor to rule out pancreatic cancer.
Can blood tests detect pancreatic cancer early?
The standard blood test, CA 19-9, is not reliable for early detection. It’s only elevated in about half of early-stage cases. New blood tests that look for tumor DNA and protein markers are in development and show promise - some with over 85% accuracy. But none are widely available yet. For now, imaging and symptoms guide diagnosis.
Does diet or lifestyle cause pancreatic cancer?
Not directly, but certain habits raise your risk. Smoking doubles your chances. Long-term obesity and heavy alcohol use are linked to higher risk. Chronic pancreatitis - often caused by alcohol - increases risk too. But most people who get pancreatic cancer have no clear lifestyle cause. Genetics and random mutations play a bigger role than most people think.
Why is survival so low compared to other cancers?
Because it’s usually found too late. The pancreas is hidden, symptoms are vague, and there’s no screening test for the general public. By the time most people are diagnosed, the cancer has already spread. Only 10-15% of cases are caught early enough for surgery. That’s why the overall survival rate is stuck at 12%. Improving early detection is the key to changing that.
Are new treatments available outside clinical trials?
Yes. FOLFIRINOX, olaparib, and pembrolizumab are FDA-approved and used in standard care for eligible patients. You don’t need to join a trial to get them. Your oncologist will test your tumor for specific mutations (like BRCA or MSI-H) to see if you qualify. These aren’t experimental anymore - they’re part of routine treatment planning.
If you or someone you know has been experiencing these symptoms, don’t wait. Talk to a doctor. Ask for a scan. Push for answers. Early detection isn’t just hopeful - it’s life-changing.
13 Comments
Kelly Essenpreis
December 3, 2025 at 05:31 AM
Yea sure and also the government is hiding the cure so they can sell chemo forever lol
Alexander Williams
December 4, 2025 at 10:49 AM
The pathophysiological cascade initiated by pancreatic neoplasms is uniquely insidious due to retroperitoneal anatomical concealment and the absence of a validated biomarker profile for premalignant detection. The current diagnostic paradigm remains fundamentally reactive rather than proactive, which explains the persistently low survival metrics despite therapeutic advances.
Suzanne Mollaneda Padin
December 5, 2025 at 11:58 AM
Just want to add that if you're over 50 and have unexplained weight loss + fatigue + mild jaundice-even if you think it’s ‘just stress’-ask for a CT or MRI. I work in primary care and I’ve seen too many patients dismissed for months because symptoms were ‘non-specific.’ Early detection isn’t paranoia. It’s prevention.
Erin Nemo
December 6, 2025 at 06:47 AM
My grandma had this. No warning. Just got tired, lost weight, then boom-stage 4. Please listen to this post. Don’t wait.
ariel nicholas
December 6, 2025 at 16:30 PM
...and yet, the medical-industrial complex thrives on late-stage intervention... while the true cure-detoxification, alkalinity, and spiritual alignment-is suppressed by Big Pharma... you're being manipulated into believing chemo is your only hope... when nature holds the answer...
Rachel Stanton
December 6, 2025 at 18:13 PM
For those with a family history: genetic counseling is free or low-cost through most hospitals. If you have a BRCA mutation or Lynch syndrome, you’re eligible for surveillance programs. Ask your doctor for a referral. It’s not scary-it’s empowering. Knowledge is your best tool.
Amber-Lynn Quinata
December 8, 2025 at 08:41 AM
I'm so glad you posted this. I've been depressed for 8 months and thought it was just burnout. But I've also lost 15 lbs and my eyes are yellowish. I'm going to the doctor tomorrow. Thank you for not making me feel crazy.
Lauryn Smith
December 9, 2025 at 07:43 AM
My mom was misdiagnosed with IBS for 11 months before they found the tumor. Please, if you feel off and nothing adds up-keep pushing. Doctors are busy, but your life isn’t a checklist. Say ‘I’m not okay’ even if they say it’s stress.
Bonnie Youn
December 10, 2025 at 09:31 AM
THIS IS SO IMPORTANT I CAN'T BELIEVE THIS ISN'T ON EVERY NEWS SITE. SHARE THIS. TELL YOUR PARENTS. TELL YOUR FRIENDS. IF YOU'RE OVER 50 AND JUST 'FEEL OFF'-GET CHECKED. YOU MIGHT SAVE A LIFE. I'M SO GRATEFUL THIS WAS POSTED.
Edward Hyde
December 11, 2025 at 08:01 AM
They’re all just trying to scare you into getting scanned so they can bill you $12k for a CT that probably shows nothing. Meanwhile, the real cause? Glyphosate. Gluten. The patriarchy. But sure, let’s just throw chemo at it like it’s 1998.
Charlotte Collins
December 12, 2025 at 11:34 AM
It’s ironic that the same system that ignores early symptoms is the one that profits from late-stage interventions. The data is clear: survival jumps from 12% to 44% with early detection. Yet funding for screening research remains negligible compared to palliative care. This isn’t a medical problem-it’s a moral one.
Margaret Stearns
December 14, 2025 at 00:12 AM
Just want to say thank you for sharing this. My dad passed from this last year. We didn't know anything. If I'd seen this sooner, I would've pushed harder. Please, if you're reading this, don't wait. Even if you think it's nothing. Just get checked.






Kenny Leow
December 1, 2025 at 23:18 PM
Thanks for laying this out so clearly. I had no idea new-onset diabetes could be such a big red flag-my uncle was diagnosed last year after his sugar spiked out of nowhere. He’s now in remission because he pushed for an MRI. Seriously, if you’re over 50 and suddenly diabetic with no family history? Don’t brush it off. Get scanned.