Imagine breaking out in hundreds of tiny, itchy bumps within minutes of starting a workout, walking to the bus, or even eating a spicy meal. No allergens, no new soap, no insect bite-just heat. That’s cholinergic urticaria, or heat hives, for millions of people worldwide. It’s not just an annoyance. For many, it’s a daily battle against their own body’s response to temperature changes.
What Exactly Are Heat Hives?
Cholinergic urticaria (CU) is a type of physical urticaria triggered by a rise in body temperature. Unlike allergic hives that come from food or pollen, these hives are caused by sweat and the nerve signals that come with it. When your core temperature climbs-even just half a degree above normal-your body’s immune system overreacts. Mast cells in your skin release histamine, causing small red bumps (1-3 mm) surrounded by red flares. These aren’t big, swollen welts like from a bee sting. They’re pinpoint, prickly, and intensely itchy or tingling.
Most people notice them on the chest (78% of cases), face (65%), upper back (62%), and arms (58%). You won’t usually see them on your palms, soles, or inside your mouth. The timing is precise: hives show up 2-15 minutes after your body heats up, peak around 15-30 minutes, and fade completely within 90 minutes after cooling down. This predictability is both a blessing and a curse. You know what’s coming-but you can’t always avoid it.
Why Does Heat Trigger This Reaction?
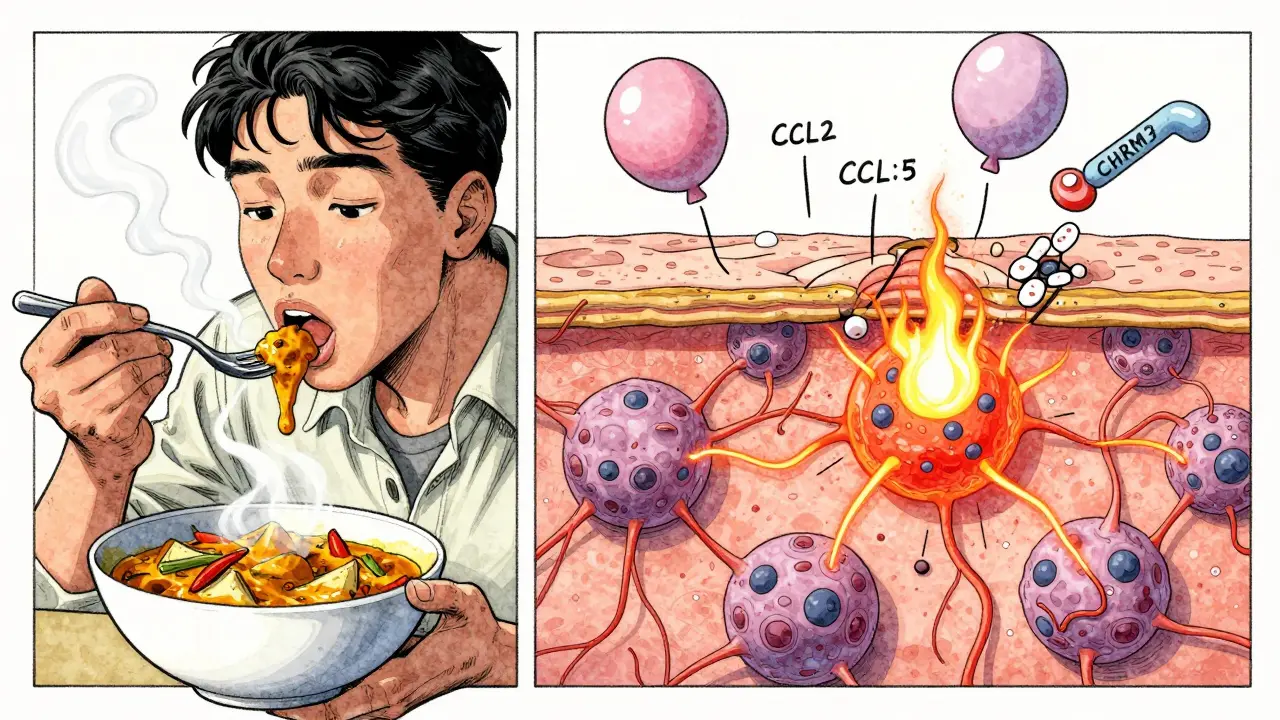
It’s not the sweat itself. It’s what happens when your sweat glands activate. Research shows that people with CU have lower levels of acetylcholinesterase (AchE) and a specific receptor called CHRM3 in their sweat gland cells. These normally help calm down nerve signals. When they’re underactive, the nerves overfire, telling your immune system to attack. This triggers inflammation and histamine release, even though there’s no foreign invader.
Studies also found elevated levels of chemokines like CCL2 and CCL5 in the skin of CU patients. These molecules act like alarm signals, pulling in immune cells to the area. It’s a neuroimmune misfire-your nerves and immune system are talking to each other in the wrong language.
How Is It Different From Other Hives?
Not all hives are the same. Here’s how CU stacks up:
- Cold urticaria: Happens when you’re exposed to cold air or water. Hives appear on exposed skin like hands or face. CU happens when you’re warm.
- Solar urticaria: Triggered by sunlight. Only affects areas hit by UV rays. CU appears anywhere you sweat-even under clothes.
- Dermatographism: You get raised lines where you scratch or rub your skin. CU’s bumps are scattered, not linear.
- Pressure urticaria: Takes hours to develop after tight clothing or sitting. CU hits within minutes.
The biggest difference? CU is tied to your body’s natural cooling system-sweating. That makes it harder to avoid than a food allergy. You can’t stop sweating without stopping life.
Who Gets Heat Hives?
Most people first notice CU between ages 15 and 25. It’s rare in children under 10 and uncommon after 50. Men and women are equally affected. It’s not inherited, but people with other types of hives or asthma are more likely to develop it.
Globally, CU affects about 0.04% to 0.07% of the population-that’s roughly 3.2 to 5.6 million people. It’s more common in warmer climates. In Southeast Asia, rates are nearly four times higher than in Scandinavia. As global temperatures rise, experts predict CU cases could increase by 15-25% in temperate regions by 2040.
What Triggers a Flare-Up?
Exercise is the #1 trigger-reported by nearly 90% of patients. But it’s not just the gym:
- Hot showers or baths
- Spicy foods (capsaicin raises body temp)
- Strong emotions (stress, anxiety, embarrassment)
- Wearing thick or non-breathable clothing
- Humid weather
- Fever or illness
One Reddit user described it perfectly: “Tiny pinprick hives that feel like hundreds of needles under my skin, starting on my chest within 5 minutes of beginning my morning run.” That’s classic CU. Even walking to your car on a 22°C day can set it off if you’re wearing a hoodie.
Can It Be Dangerous?
Most cases are mild-just itchy bumps. But for about 1 in 8 people, CU can trigger serious symptoms:
- Wheezing or trouble breathing
- Dizziness or lightheadedness
- Rapid heartbeat (over 100 bpm)
- Drop in blood pressure (below 90 mmHg)
- Feeling like you’re going to pass out
These are signs of systemic involvement-and in rare cases, anaphylaxis. About 8.7% of CU patients are prescribed epinephrine auto-injectors. That’s not because they’re likely to die, but because the risk is real enough to warrant a safety net. Misdiagnosis is common too. Around 22% of people who go to the ER with CU symptoms are wrongly told they’re having exercise-induced anaphylaxis. That leads to wrong treatments and unnecessary fear.
How Is It Diagnosed?
There’s no blood test. Diagnosis relies on history and a simple provocation test. The gold standard is the passive warming test: you sit in a warm room (usually 39-40°C) for 15-20 minutes while your core temperature is monitored. If you develop the classic pinpoint hives within 15 minutes, and your temperature rose just 0.5°C above baseline, you have CU. This test works in 94% of confirmed cases.
Some doctors may also use exercise testing-treadmill or cycling-until you sweat. But the passive test is safer and more controlled.

What Treatments Actually Work?
There’s no cure. But most people can manage symptoms effectively.
First-line treatment: Second-generation antihistamines like cetirizine (Zyrtec) or loratadine (Claritin). These block histamine without causing drowsiness. The standard dose is 10mg daily. But many patients need higher doses-up to 40mg of cetirizine daily. Studies show 68% of people get relief at standard doses, and 73% respond to higher doses.
If antihistamines aren’t enough: Doctors may add famotidine (Pepcid), an H2 blocker. It’s usually taken at 20mg twice daily. In one study, this combo helped 57% of patients who didn’t respond to antihistamines alone.
For severe, chronic cases: Omalizumab (Xolair), a biologic originally for asthma and chronic hives, was approved for refractory CU in Europe in June 2023. In trials, 78% of patients had complete symptom control with weekly 300mg injections. But it’s expensive-around $3,500 per month in the U.S.-and not widely used due to cost.
First-generation antihistamines like diphenhydramine (Benadryl) are avoided. They cause drowsiness, and 58% of CU patients on them say it interferes with work or school.
How to Prevent Flare-Ups
Prevention is about controlling heat and sweat-not avoiding life.
- Wear moisture-wicking clothing: Polyester or merino wool pulls sweat away from skin. Avoid cotton-it holds moisture and traps heat.
- Work out in cool environments: Air-conditioned gyms, early morning runs, or indoor swimming help. One user said switching to indoor workouts cut his flare-ups from daily to 1-2 times a month.
- Avoid spicy foods: Capsaicin in chili peppers raises core temperature. Even one meal can trigger a reaction.
- Take cool showers after activity: Don’t wait until you’re overheated. Cool water helps reset your body’s temperature.
- Use a fan or cold towel: Keep one handy during workouts or in hot weather.
- Track your triggers: Use a journal or app like the Urticaria Center’s free tracker. Log temperature, activity, food, and symptoms. Most people identify their personal trigger point at 38.1°C ± 0.7°C core temperature.
- Manage stress: Anxiety and embarrassment can trigger CU. Breathing exercises or mindfulness can help reduce emotional spikes.
What About Long-Term Outlook?
Good news: CU often improves with age. About 30% of people see their symptoms disappear completely within 7-10 years. For others, it becomes more manageable. The key is consistency with prevention and medication.
Research is moving forward. By 2026, scientists aim to identify at least two reliable biomarkers for CU-something blood tests can detect. Wearable tech is also advancing. ThermaCare and Mayo Clinic are testing smart garments that regulate skin temperature in real time. Early results show a 63% drop in flare frequency during exercise.
By 2028, you might wear a shirt that alerts you when your skin temperature hits your personal threshold-before the hives start.
Final Thoughts
Cholinergic urticaria isn’t just about skin. It’s about losing control of your body’s natural responses. It’s skipping weddings because you’re afraid of overheating in a suit. It’s avoiding the gym because you’d rather sit than suffer. But it doesn’t have to be that way.
With the right meds, smart clothing, and awareness of your personal triggers, you can live fully-even in the heat. You don’t need to quit exercise. You don’t need to hide. You just need to understand your body’s signals-and respond before they turn into hives.
Can cholinergic urticaria go away on its own?
Yes, about 30% of people experience complete resolution of symptoms within 7 to 10 years of onset. For many, flare-ups become less frequent and less severe with age, especially after the mid-30s. However, there’s no way to predict who will outgrow it, so management is still important.
Is cholinergic urticaria an allergy?
No, it’s not an allergy. Allergies happen when your immune system reacts to a foreign substance like peanuts or pollen. Cholinergic urticaria is a physical reaction to heat and sweat. Your body isn’t fighting an invader-it’s misfiring internally. That’s why antihistamines help, but allergy tests come back negative.
Can I still exercise with heat hives?
Absolutely-but you need to adjust how you do it. Work out in cooler environments, wear breathable clothing, stay hydrated, and cool down immediately after. Many people with CU train successfully using indoor treadmills, swimming pools, or early morning outdoor sessions. Start slow and monitor your body’s response. Some find that gradual exposure (like short, low-intensity workouts) helps build tolerance over time.
Why do spicy foods trigger heat hives?
Spicy foods contain capsaicin, which activates heat receptors in your mouth and skin. This tricks your body into thinking it’s overheating, triggering the same nerve pathways that cause sweating and histamine release. Even if you’re not physically hot, your body responds as if you are. Many patients report flare-ups after eating curry, hot sauce, or even spicy noodles.
Should I carry an epinephrine auto-injector?
If you’ve ever had symptoms like wheezing, dizziness, rapid heartbeat, or trouble breathing during a flare-up, yes. About 8.7% of CU patients are advised to carry one. It’s not for every case-but if you’ve had systemic reactions, it’s a safety measure. Talk to your allergist. They’ll help you decide based on your history.
Are there any new treatments on the horizon?
Yes. Omalizumab (Xolair) is now approved for severe CU in Europe and under review elsewhere. Three Phase II clinical trials are testing new drugs targeting mast cells and inflammatory pathways, including fevipiprant and PQ-12. Wearable tech that monitors skin temperature in real time is also in development and could help prevent flares before they start. These aren’t available yet, but the research is promising.
Can climate change make cholinergic urticaria worse?
Yes. Rising global temperatures and more frequent heatwaves are expected to increase CU prevalence, especially in temperate regions. Studies project a 15-25% rise in cases by 2040. If you live in a city with hotter summers, you may notice more frequent or severe flare-ups. Adapting your environment-using AC, avoiding peak heat hours, and choosing cooling fabrics-will become even more important.
15 Comments
Kasey Summerer
January 18, 2026 at 08:37 AM
So let me get this straight... my sweat is betraying me? 🤡 I thought my body was on my side. Now I gotta wear tech fabric and cry into my protein shake? 😭
kanchan tiwari
January 19, 2026 at 22:32 PM
THEY KNOW. THEY ALL KNOW. This isn't natural. Why are they making us sweat? Why now? The government is using heat waves to test our immune systems. I saw a drone above my yoga studio last week. They're watching. I can feel it.
Bobbi-Marie Nova
January 20, 2026 at 02:54 AM
I used to think I was just bad at exercise until I got diagnosed. Now I laugh when people say 'just push through' - like bro, I'm not trying to become a human pincushion. Cool showers post-workout? Game changer. Also, no more vindaloo before spin class.
Allen Davidson
January 20, 2026 at 15:35 PM
If you're having systemic reactions, get an EpiPen. Don't wait for your first near-death experience. This isn't a 'maybe' - it's a 'yes, you need this.' And if your doctor doesn't get it, find a new one. Your life isn't a suggestion.
Rob Deneke
January 21, 2026 at 17:08 PM
Cetirizine works but dont take benadryl its a trap youll be useless all day and still itchy
Riya Katyal
January 22, 2026 at 04:34 AM
You're all so naive. This isn't about heat. It's about your soul being overwhelmed. You're too connected to your phones, too stressed, too disconnected from nature. The hives are your spirit screaming. Go meditate in a forest. Or at least turn off TikTok.
waneta rozwan
January 23, 2026 at 00:14 AM
I can't believe people still believe in antihistamines. This is a spiritual imbalance. You're not 'allergic to heat' - you're allergic to modern life. My cousin's acupuncturist cured her by aligning her chakras with moon phases. Also, avoid the color red. It attracts heat energy.
Nicholas Gabriel
January 23, 2026 at 10:28 AM
I want to emphasize, please, and I cannot stress this enough: the passive warming test is the gold standard, and if your doctor doesn't offer it, you must insist. Also, tracking your core temperature with a wearable thermometer - like the Tempus Pro - is not optional, it's essential. Many people miss their personal threshold because they're guessing. Don't be one of them.
swarnima singh
January 23, 2026 at 17:18 PM
i think its not just the heat... its the weight of existence. we are all just sweating through life. the hives are the universe reminding us we are fragile. i cried after my first flare. not from the itch. from the loneliness. we are all just trying to cool down in a world that never stops burning.
Isabella Reid
January 24, 2026 at 20:04 PM
I used to think I was just 'sensitive' until I read this. Now I know it's a real condition. I started wearing merino wool tees and my flare-ups dropped 80%. Also, cool showers right after any activity - even a short walk. I wish I'd known this 5 years ago.
Jody Fahrenkrug
January 24, 2026 at 22:32 PM
I just got diagnosed last month. Took me 3 years to find someone who knew what CU was. Now I carry Zyrtec in my gym bag. I still run. I just do it at 6am. And I don't care if people think I'm weird for sitting with a cold towel on my neck after cardio.
john Mccoskey
January 25, 2026 at 05:50 AM
Let me break this down scientifically. You're attributing a neuroimmune dysregulation to lifestyle hacks and antihistamines, which are merely symptomatic palliatives. The real issue is the systemic breakdown of cholinergic signaling pathways exacerbated by environmental toxins, processed foods, and chronic low-grade inflammation. The fact that you're even considering 'cool showers' as a solution reveals a fundamental misunderstanding of pathophysiology. You're treating a symptom while ignoring the root: a civilization that has severed its biological contract with thermoregulation. Omalizumab is a band-aid on a severed artery. We need systemic reform, not better fabrics.
Ryan Hutchison
January 25, 2026 at 16:32 PM
America has the best doctors, the best meds, the best science. Why are people in India and Europe even talking about this? We solved this decades ago. You people need to stop whining and just get used to it. If you can't handle a little sweat, maybe you shouldn't be outside. We have AC for a reason. Stop blaming climate change - start building thicker skin.
Samyak Shertok
January 25, 2026 at 20:22 PM
Wait - so the whole medical community is just now realizing sweat can cause hives? I've had this since I was 12. I used to wear ice packs under my shirt during PE. Everyone thought I was faking. Now you're writing a 2000-word essay on it? The real story is that medicine moves slower than a snail on a treadmill.





Henry Ip
January 17, 2026 at 00:31 AM
I've had this for years and Zyrtec at 20mg daily is my lifeline. No drowsiness, just quiet days. Found my trigger temp is 38.2°C after tracking for 6 months. You don't need to quit running, just adapt.