
When you fill a prescription, do you ever wonder why two pills cost more than one? It’s not just you. Many people pay more for combination drugs-like asthma inhalers or blood pressure pills that pack two medicines in one-when they could be saving big by switching to separate generic versions. The truth? Generic combinations aren’t always the cheapest option. Sometimes, buying the individual generics separately saves you hundreds of dollars a year.
Why Some Generics Cost More Than Others
Not all generic drugs are created equal. Just because a drug is off-patent doesn’t mean it’s cheap. A 2022 study from JAMA Network Open looked at the top 1,000 generics used in Colorado and found something surprising: 45 of them were costing patients and insurers way more than they should. These weren’t brand-name drugs. They were generics. But they were priced 15.6 times higher than other generics with the same effect.
Take a common example: a generic version of a blood pressure medication might cost $120 for a 30-day supply. But a different generic, with the exact same active ingredient and dosage, might only cost $8. That’s a 93% difference. Why? It’s not about quality. It’s about competition. When multiple companies make the same drug, prices drop. But if only one company makes a particular generic, they can charge more. It’s like having a monopoly on a basic medicine.
The study found that replacing these overpriced generics with cheaper alternatives could cut total spending by 88.3%. That’s $7.5 million down to $873,711 in just one state. And it wasn’t because they switched to a different medicine. They just switched to a different version of the same medicine-different strength, different pill shape, different manufacturer. Same effect. Much lower cost.
Combination Drugs: The Hidden Cost Trap
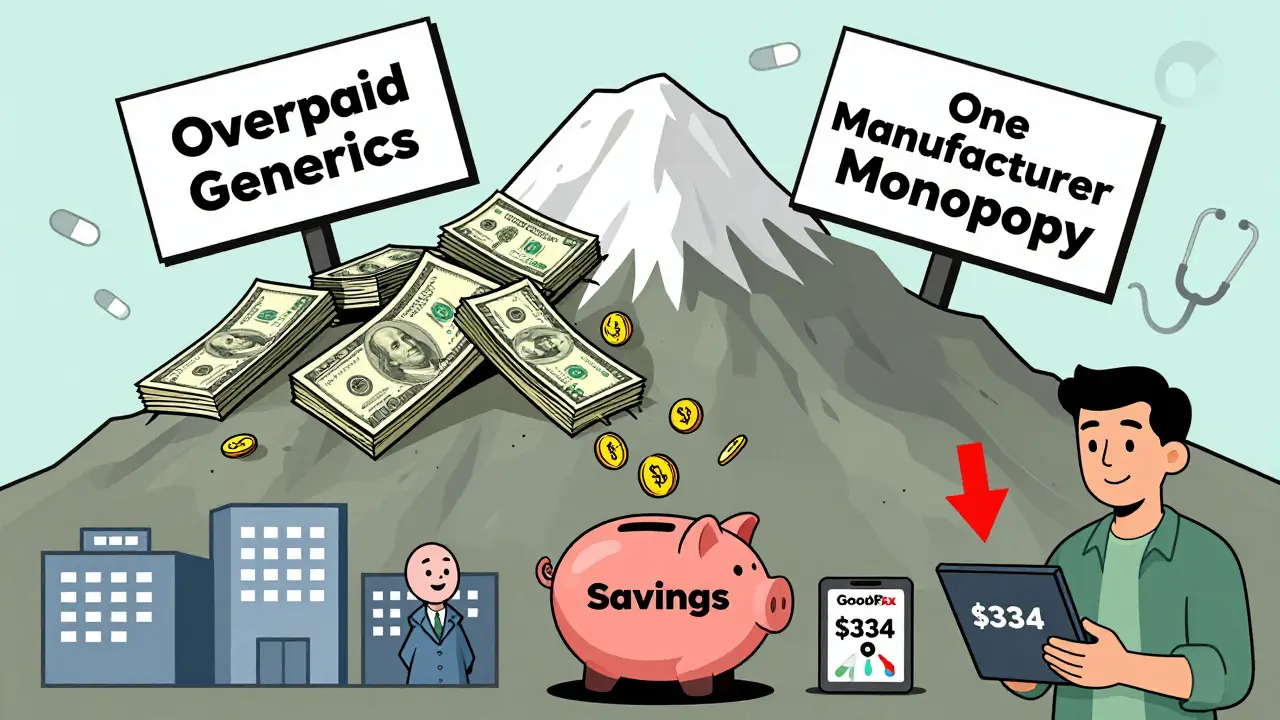
Combination drugs are designed to make life easier. One pill instead of two. Sounds smart, right? But when those combinations are brand-name products, they’re often priced way above the sum of their parts. Take Advair Diskus, a popular asthma inhaler that combines an inhaled corticosteroid and a long-acting beta agonist. Before generics hit the market, it cost about $334 per inhaler. Then Wixela Inhub, the first generic version, came out. It cost $115. That’s a 65.6% drop.
But here’s the twist: you didn’t need to buy Wixela Inhub to save that much. You could have bought the two individual generic inhalers separately-fluticasone and salmeterol-and combined them yourself. In many cases, the total cost of buying them separately was even lower than the generic combination. And you had more control over dosing. The same pattern shows up with diabetes drugs like Janumet (metformin + sitagliptin) and blood pressure combos like Amturnide (aliskiren + amlodipine + hydrochlorothiazide). The branded combo is expensive. The generic combo is cheaper. But the individual generics? Often the cheapest of all.
How Much Can You Actually Save?
The numbers speak for themselves. The Association for Accessible Medicines reported that the top 10 generic drugs saved $89.5 billion in 2023 alone. Crestor (rosuvastatin) went from $5.78 per pill to $0.08. Prilosec (omeprazole) dropped from $3.31 to $0.05. That’s 98% to 99% savings. And it wasn’t magic. It was competition. When five companies start making the same drug, prices crash.
Even better: a 2023 study from JAMA Health Forum looked at 843 million pharmacy fills and found that 11.8% of them had potential out-of-pocket savings. Uninsured patients saved the most-28.9% of their fills had lower-cost options. Medicare users saved on 5.5% of fills. Private insurance? 7.1%. The average savings per prescription? $4.96. But for some, it was over $10. That’s $60 a month. $720 a year. Just by switching pills.
And it’s not just about pills. A 2022 analysis of inhaled asthma medications showed that switching from branded Advair to generic Wixela saved $941 million in one year. But if patients had gone even further-buying the two separate generics instead of the combo-the savings could have been even higher.
What’s Holding You Back?
So why don’t more people do this? Three big reasons:
- Doctors don’t always know. Many prescribers assume the combo pill is the best-or only-option. They don’t realize the individual components are available as cheap generics.
- Pharmacies don’t always offer it. Some pharmacies default to the combo because it’s easier to dispense. They don’t ask if you want to split it.
- Insurance formularies push combos. Some plans still list the combo as the preferred option, even if the individual generics are cheaper. They get rebates from drugmakers. You don’t.
The FDA’s Orange Book lists which generics are therapeutically equivalent. If a drug has an “A” rating, it means you can swap it safely. But that doesn’t mean your pharmacist will suggest it. You have to ask.
How to Find the Cheapest Option
Here’s how to save without risking your health:
- Ask your doctor: “Are the individual components of this combo drug available as separate generics?”
- Ask your pharmacist: “Can I get the two drugs separately instead of in one pill? Which option is cheaper?”
- Use free price-check tools like GoodRx, SingleCare, or Blink Health. Compare the cost of the combo pill vs. the two individual generics.
- Check your insurance formulary. If the combo is listed as “preferred,” ask if the individual generics are covered at the same tier.
- If you’re on Medicare or Medicaid, ask about the 340B program or discount pharmacies. Some savings are hidden.
Don’t assume the prescription you got is the cheapest. A 2023 report found that 50% of all prescriptions with savings had savings under $5. But 28% had savings over $10. That’s the difference between paying $100 a month and $80. That’s $240 a year. Enough for a weekend trip, a new pair of shoes, or a refill you didn’t have to skip.
What’s Changing in the Market
The generic drug market is under pressure. While 90% of prescriptions are filled with generics, they make up only 23% of total drug spending. That’s a win. But there are warning signs. Generic shortages are rising. The top 10 manufacturers control 40% of the market. That means less competition. And less price pressure.
The FDA approved 724 generic drugs in 2023-down from 843 in 2017. Fewer approvals mean fewer competitors. Fewer competitors mean higher prices. That’s why it’s more important than ever to check your options. The system isn’t broken. But it’s not working for everyone.
Meanwhile, biosimilars-generic versions of complex biologic drugs-are starting to enter the market. The first biosimilar for Humira, a top-selling autoimmune drug, hit shelves in 2023. Prices are already 20-30% lower than the brand. More are coming. This is the next wave of savings.
Bottom Line: You Have Power
Generic drugs saved $3.7 trillion over the last decade. But the biggest savings aren’t always in the combo pill. Sometimes, they’re in the two separate generics you never thought to ask for. You don’t need a PhD to save money on your meds. You just need to ask the right questions.
Next time you get a prescription for a combination drug, pause. Look up the ingredients. Compare prices. Talk to your pharmacist. You might be paying way more than you need to. And you don’t have to.
Are combination drugs always more expensive than individual generics?
No, not always. Some generic combination drugs are priced competitively, especially when multiple manufacturers produce them. But in many cases, buying the two individual generics separately is cheaper. For example, Wixela Inhub (a generic combo for asthma) costs $115, but buying fluticasone and salmeterol separately can drop the total cost below $100. Always compare prices using tools like GoodRx.
Can I ask my pharmacist to split my combo prescription into two separate generics?
Yes, absolutely. Pharmacists are trained to help you find the most cost-effective option. If your prescription is for a combination drug, ask: “Can I get the individual components as separate generics? Which option is cheaper?” They can check your insurance formulary and the current prices. Many pharmacies will do this automatically if you ask.
Why are some generic drugs so expensive?
Some generics are expensive because there’s little competition. If only one company makes a particular generic, they can charge more. This often happens when the drug has a complex manufacturing process, or when patents or regulatory delays block other companies from entering the market. The JAMA Network Open study found that 62% of high-cost generics had cheaper alternatives with the same active ingredient-just in a different strength or form.
Do insurance plans encourage generic combinations?
Sometimes, yes. Some insurance plans list combination drugs as “preferred” because they get rebates from drugmakers. But that doesn’t mean they’re the cheapest option for you. Always check your out-of-pocket cost for the combo versus the individual generics. If the individual generics are covered at the same tier, you could save money by choosing them.
Is it safe to switch from a combo drug to two separate generics?
Yes, if your doctor approves it. The FDA’s Orange Book lists drugs that are therapeutically equivalent. If both the combo and the individual generics have an “A” rating, they’re considered interchangeable. Always consult your doctor before making changes, especially for medications like blood pressure, diabetes, or asthma drugs. But switching to separate generics is often safer and cheaper than staying on a high-cost combo.
11 Comments
Chima Ifeanyi
February 12, 2026 at 06:26 AM
Let’s deconstruct this with structural economic analysis. The premise assumes perfect market efficiency, which is a fallacy. The JAMA study cited only examined Colorado - a single-state sample with idiosyncratic formulary constraints. The national variance in generic pricing is heterogenous due to PBMs, bulk procurement asymmetries, and vertical integration among distributors. Moreover, the 88.3% savings figure is misleading - it conflates aggregate payer savings with individual out-of-pocket savings, which are often negligible due to tiered copays and prior authorization hurdles. You’re optimizing for a metric that doesn’t align with patient financial burden.
Also, the ‘buy two generics’ strategy ignores pharmacokinetic synergies, adherence metrics, and pill burden - all clinically validated factors in chronic disease management. The reductionist cost-per-pill model is dangerous.
Ken Cooper
February 12, 2026 at 16:29 PM
bro i had no idea this was even a thing 😳
i was paying $90 a month for my asthma combo pill and just last week i asked my pharmacist if i could get fluticasone and salmeterol separate and she was like ‘ohhh yeah we can do that for $28’
like… why does no one talk about this??
also i used blink health and got the two generics shipped to my house for $17 total… i think i just saved my rent money for april
Susan Kwan
February 13, 2026 at 23:49 PM
Of course the system is rigged. Drug companies know people are too tired to fight. They design combo pills to look ‘convenient’ - then jack up the price because they know most doctors won’t question it and most patients won’t ask.
I’ve been in this system for 12 years. I’ve been handed 17 different combo prescriptions. I’ve saved $11,000 since I started asking for the individual generics. Not because I’m smart. Because I was desperate.
And yes, I’ve had pharmacists roll their eyes. I’ve had doctors say ‘it’s not worth the hassle.’
It’s worth it. Always.
Random Guy
February 15, 2026 at 21:19 PM
OMG I JUST REALIZED I’M PAYING $180 A MONTH FOR A PILL THAT’S MADE OF TWO THINGS THAT EACH COST $7.
MY LIFE IS A LIE.
I’M GOING TO THE PHARMACY TOMORROW AND I’M GOING TO ASK THEM TO BURN DOWN THE COMBO PILL INDUSTRY WITH FIRE.
THIS POST CHANGED MY LIFE.
also i just cried a little.
Tom Forwood
February 16, 2026 at 04:15 AM
As a Nigerian-American who’s had to navigate both US and Nigerian healthcare - this hits different.
In Nigeria, you buy generics in open markets, no insurance, no formulary, no combo pills. Just a bag of pills with the name written in marker. You pay cash. You compare. You live.
Here? We’re trapped in a maze of insurance tiers, rebates, and pharmacy defaults. The fact that we have to be medical detectives just to afford our meds is insane.
But hey - at least we have GoodRx. Thank god for that. I always tell my cousins: ‘Don’t take the first script. Ask for the price of the parts.’ It’s not rude. It’s survival.
John McDonald
February 17, 2026 at 00:05 AM
This is one of those posts that makes you feel both angry and hopeful.
I’ve been helping my mom manage her diabetes meds for years. We thought Janumet was the only option. Turns out metformin + sitagliptin separately cost half as much. She’s been on it for six months now. No side effects. No issues. Just way more money in her pocket.
Doctors don’t know. Pharmacies don’t tell. But you? You can change that. Just ask. Seriously. Ask. Ask again. Ask until they blink.
You’re not being difficult. You’re being smart.
Chelsea Cook
February 18, 2026 at 03:55 AM
Let me be real - I used to think this was just ‘hustle culture’ nonsense. ‘Oh, just switch your meds and save $700!’
Then my sister got diagnosed with hypertension. She was on a combo pill. $160/month. I made her call her pharmacy. They said ‘sure, we can split it.’ Total cost: $32.
She cried. Not because she was sad. Because she realized she’d been overpaying for two years.
So if you’re thinking ‘nah, it’s too much work’ - you’re wrong. It’s not work. It’s justice.
Go ask. Now.
Andy Cortez
February 18, 2026 at 21:33 PM
Y’all are acting like this is some revolutionary secret - it’s not. It’s basic capitalism. When there’s no competition, prices go up. When there’s competition, they crash.
The problem? Pharma doesn’t want competition. They want you to think the combo pill is ‘better.’ It’s not. It’s just a marketing trick wrapped in a white pill.
And don’t get me started on how pharmacies get kickbacks for pushing combos. They don’t care about you. They care about the rebate.
So yeah - ask. Demand. Demand again. And if they say no? Go to a different pharmacy. There are 10,000 of them. One of them will help you.
Jacob den Hollander
February 19, 2026 at 17:40 PM
Hey - I just wanted to say thank you for writing this. I’ve been doing this for years - splitting combos, comparing prices, calling around. It’s exhausting. No one talks about how hard it is to be your own advocate in healthcare.
I’ve had pharmacists hang up on me. I’ve had doctors say ‘I don’t have time for this.’ I’ve had insurance reps tell me ‘it’s not covered.’
But I kept going. Because I have a kid. And I need to be here for them.
So if you’re reading this and you’re scared to ask - I get it. But please, try. Even once. You might be surprised.
You’re not alone. We’re all out here doing this. And you’re doing great.
John Sonnenberg
February 19, 2026 at 19:55 PM
I can’t believe this is even a thing.
How is it legal for a company to sell one pill for $120 when the two ingredients inside it cost $8 total?
This isn’t capitalism.
This is theft.
And the fact that we’ve normalized this? That we’ve accepted it?
That’s the real tragedy.






Randy Harkins
February 10, 2026 at 08:15 AM
Just wanted to say thank you for this post. I switched my blood pressure meds from a combo pill to two separate generics last year, and my monthly cost dropped from $142 to $21. I didn’t even know this was an option until my pharmacist mentioned it. Now I check every prescription with GoodRx before I fill it. Small changes, huge savings.
Also, if you’re on Medicare, ask about the 340B program - some pharmacies offer insane discounts if you know to ask. Seriously, this stuff changes lives.