When you’re managing bipolar disorder with lithium carbonate, it’s not just about taking a pill every day. The real challenge lies in keeping your blood levels just right-too low, and the medication won’t work. Too high, and you risk serious side effects. This is especially true with lithium carbonate generics, where small differences in how the drug is made can change how your body handles it.
Why Lithium Is Different From Other Medications
Lithium isn’t like most other drugs. It has a narrow therapeutic index, meaning the gap between a helpful dose and a dangerous one is tiny. For most people, the safe and effective range is between 0.6 and 1.2 mmol/L. At 1.5 mmol/L, you’re already in danger zone. Levels above 2.0 mmol/L can cause seizures, heart rhythm problems, or even coma. This isn’t just theory. In the 1981 study by Baastrup and Schou, patients on lithium had half the relapse rate compared to those on placebo. But that benefit only shows up when levels are steady and within range. That’s why checking your blood levels isn’t optional-it’s essential.Generics Aren’t Always Interchangeable
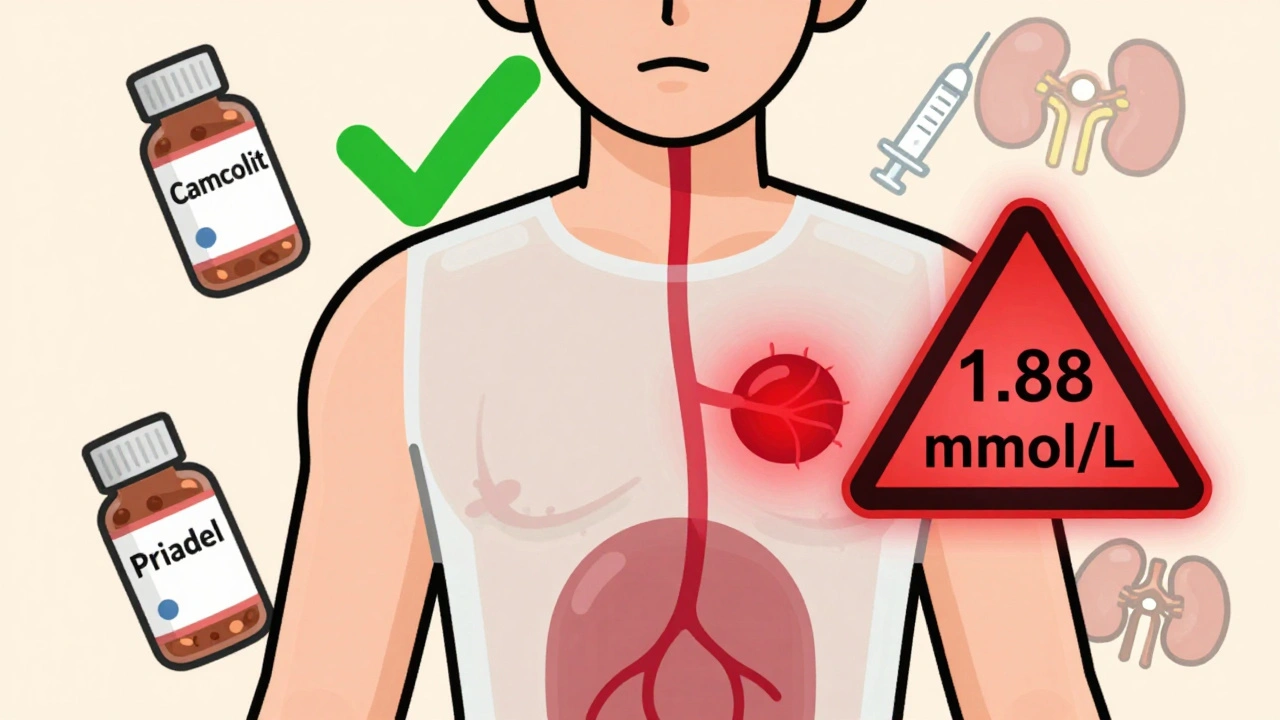
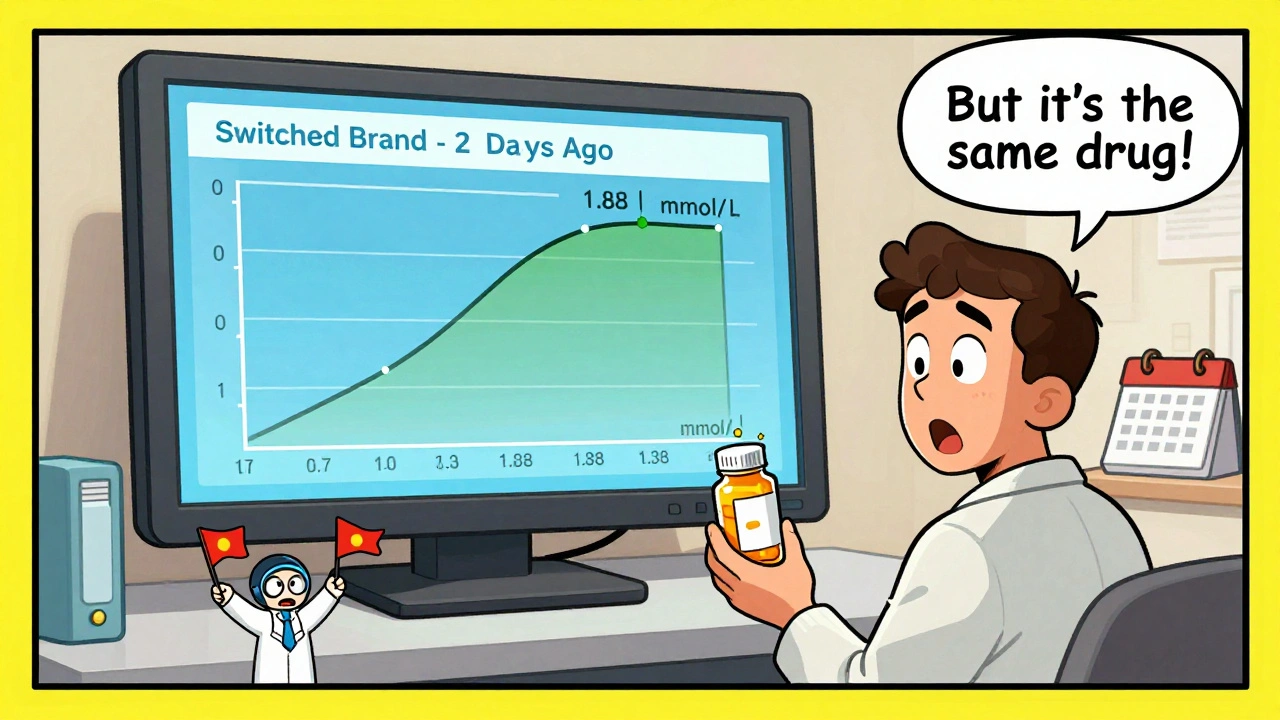
All generic lithium carbonate must prove they’re bioequivalent to the brand-name version. That means they should deliver the same amount of drug into your bloodstream over time. But bioequivalence doesn’t mean identical. Take Camcolit and Priadel-both are sustained-release forms. A 2024 study found that when patients switched from one to the other, their average serum levels jumped by 11%, even though the dose stayed the same. Some patients ended up with levels above 1.3 mmol/L, which is above the recommended range. Four patients in that study had levels over 1.3 mmol/L after switching brands. One hit 1.88 mmol/L-close to toxic. Why does this happen? It’s about how the drug is released. Immediate-release lithium hits peak levels in 1-2 hours. Sustained-release versions like Priadel or Camcolit take 4-5 hours. Even small differences in coating, particle size, or manufacturing can change absorption. One brand might release 20% more lithium in the first few hours than another. That’s enough to throw off your balance.When to Check Your Levels
You shouldn’t wait until you feel off. Regular monitoring is the only way to stay safe.- When you start lithium: Check every week until stable.
- After any dose change: Wait 5-7 days, then test.
- After switching brands: Test within 2 weeks.
- During stable maintenance: Every 3-6 months.
- If you get sick, dehydrated, or start a new medication: Test immediately.
Target Levels Change Based on Your Situation
There’s no one-size-fits-all number. Your target depends on what you’re treating and how old you are.- Acute mania: 0.8-1.0 mmol/L
- Maintenance (adults): 0.6-0.8 mmol/L
- Maintenance with sustained-release: 0.8-1.0 mmol/L
- Over 60: 0.4-0.6 mmol/L (some experts recommend even lower)
What Else Affects Your Lithium Levels
Lithium doesn’t live in a vacuum. Many things can shift your levels without you realizing it.- Dehydration: Sweating, diarrhea, or not drinking enough water can spike levels fast.
- NSAIDs: Ibuprofen, naproxen, and even aspirin can reduce kidney clearance of lithium.
- Diuretics: Water pills like hydrochlorothiazide are especially risky.
- Thyroid issues: Lithium causes hypothyroidism in up to 15% of users. Check TSH every 6 months.
- Renal function: Your creatinine and eGFR need checking every 3-6 months. The 2022 CANMAT guidelines now recommend cystatin C testing for better accuracy.
What to Do If You Switch Brands
If your pharmacy switches your lithium from one generic to another without telling you, don’t assume it’s safe. This happens more than you think. About 12.5% of lithium prescriptions are filled without brand specification. Here’s what you should do:- Ask your pharmacist: “Is this the same brand as before?”
- Call your prescriber immediately if you notice new side effects: tremors, nausea, confusion, frequent urination, or muscle weakness.
- Get a blood test within two weeks of the switch.
- Keep a log: Note your dose, brand name, and any symptoms.
Long-Term Monitoring Is Non-Negotiable
Lithium is one of the oldest and most effective mood stabilizers. It cuts suicide risk in half for people with bipolar disorder. But it’s not a set-it-and-forget-it drug. You need to stay involved. Track your kidney and thyroid numbers. Drink water. Avoid NSAIDs. Report changes in your mood or energy. Keep a list of all your meds. Ask questions. The good news? With careful management, lithium remains a first-line treatment for bipolar I disorder. Around 60% of long-term users still take it, even with newer options on the market. That’s because nothing else has its track record for preventing relapse.What’s Next for Lithium Therapy
Science is moving toward smarter dosing. The International Consortium on Lithium Genetics (ConLiGen) has found 30 genetic markers linked to how people process lithium. In the future, a simple blood test might tell your doctor exactly how much you need. Some clinics are already testing AI tools that pull data from your EHR-age, weight, creatinine, dose history-and suggest optimal doses. These aren’t mainstream yet, but they’re coming. Until then, the best tool you have is consistent monitoring. No matter what brand you’re on, your serum level is the only true measure of whether lithium is working safely for you.Can I switch between lithium generics without checking my blood levels?
No. Even though generics are required to be bioequivalent, small differences in how they release lithium can cause your blood levels to rise or drop. Studies show patients have had toxic levels after switching brands. Always get a serum lithium test within two weeks of any brand change.
What’s the safest lithium level for someone over 65?
For patients over 65, most experts recommend a target range of 0.4-0.6 mmol/L. Kidney function declines with age, and lithium is cleared mainly by the kidneys. Lower doses and tighter monitoring are essential to avoid toxicity. Some doctors may start even lower, at 0.3-0.5 mmol/L, depending on health status.
Why do I need to check my thyroid if I’m on lithium?
Lithium interferes with thyroid hormone production in 5-15% of users, leading to hypothyroidism. Symptoms like fatigue, weight gain, cold intolerance, or depression can be mistaken for bipolar symptoms. A simple TSH blood test every 6 months catches this early. If your thyroid is underactive, you can often manage it with levothyroxine while staying on lithium.
Can I take ibuprofen while on lithium?
Avoid ibuprofen, naproxen, and other NSAIDs if possible. They reduce how well your kidneys clear lithium, which can cause dangerous buildup. Use acetaminophen (paracetamol) for pain instead. If you must take an NSAID, get your lithium level checked within a week.
Is lithium still used today, or are there better options?
Lithium is still a first-line treatment for bipolar I disorder, especially for preventing mania and suicide. While newer drugs like lamotrigine or valproate are used, none have the same long-term evidence for preventing relapse. About 60% of people on long-term bipolar maintenance still take lithium. Its value lies in proven results-not popularity.
How often should I get my kidney function tested?
Every 3-6 months if you’re stable. Test serum creatinine and calculate eGFR. The latest guidelines (2022 CANMAT/ISBD) now recommend adding cystatin C, which is more accurate than creatinine alone for detecting early kidney changes. If your eGFR drops below 60 mL/min, your doctor may lower your dose.
What should I do if I miss a dose of lithium?
If you miss one dose, take it as soon as you remember-if it’s within a few hours of your usual time. Don’t double up. If you miss more than one dose, contact your doctor before restarting. Missing doses can destabilize your mood and make future dosing harder to predict. Consistency is key.
14 Comments
Inna Borovik
December 7, 2025 at 11:39 AM
It’s fascinating how people treat lithium like it’s just another antidepressant. The fact that you need blood tests every few months isn’t a bug-it’s a feature. This isn’t a drug you take because it feels good. It’s a precision instrument. And generics? They’re like swapping out engine parts in a jetliner because it’s cheaper. The math doesn’t lie: 11% increase in serum levels after a switch? That’s not bioequivalence-that’s negligence dressed up as cost-saving.
Jackie Petersen
December 8, 2025 at 01:08 AM
Why are we even talking about generics? The real problem is that Big Pharma doesn’t want you to know lithium is the OG mood stabilizer. They make billions off new antipsychotics that cost $1,200 a month. Lithium? It’s been around since the 1940s. It’s cheaper than your coffee habit. So of course they’re pushing you to switch brands-so you’ll eventually give up and take something that makes them money. Wake up, people.
Annie Gardiner
December 9, 2025 at 11:45 AM
What if… we’re all just chasing a number? Like, what if lithium doesn’t actually fix anything? What if it just makes us numb enough to stop screaming? I’ve been on it for years. My levels are ‘perfect.’ But I still cry in the shower. I still forget my kids’ birthdays. So… what’s the point? Are we just trying to make our suffering more predictable? Or are we just trying to make doctors feel like they’re doing something?
Rashmi Gupta
December 9, 2025 at 13:31 PM
I’m from India. We don’t even have access to branded lithium here. We get generics that come in packets with no labels. I once took a pill that looked like a candy. My cousin thought it was sugar. She didn’t know I was on lithium. She ate two. She’s fine now. But I still have nightmares. So yes-this matters. But here? Nobody cares. We just take what’s handed to us.
Andrew Frazier
December 10, 2025 at 20:04 PM
Umm… why are we letting foreigners make our meds? I mean, come on. Lithium is a mineral. It’s not rocket science. Why are we trusting Indian and Chinese factories to get the coating right? We got the tech here in the USA. We got the labs. We got the scientists. Let’s make our own damn lithium. No more brand switches. No more surprises. No more hospital trips. America first-meds first.
Kumar Shubhranshu
December 11, 2025 at 13:25 PM
Check levels every time you switch. Simple. Don't overthink. If you feel weird, get tested. No drama. No conspiracy. Just science. Your kidneys don't lie. Your blood doesn't lie. Trust the test. Not the pharmacy.
Mayur Panchamia
December 13, 2025 at 10:16 AM
Let me tell you something, folks-lithium isn’t just a drug, it’s a WARFARE TOOL. They’ve been using it since the Cold War to keep soldiers calm during missions. The Russians? They’ve got their own formula. The Chinese? They control 70% of the lithium mines. And now they’re slipping us generics with unknown coatings? This isn’t healthcare-it’s a slow-motion chemical coup. You think your tremors are side effects? Nah. That’s the enemy inside your bloodstream.
Saketh Sai Rachapudi
December 13, 2025 at 12:17 PM
why do people think its okay to switch brands? i mean like… if you had a heart pacemaker and they swapped it for a knockoff… would you be chill? no. you’d be screaming. lithium is just as vital. its not a phone charger. its your brain. and if you dont check your levels after a switch… you deserve what you get. i dont care if you’re ‘too busy.’ your life is on the line. get your blood drawn. or stop complaining when you end up in the er.
Akash Takyar
December 13, 2025 at 19:35 PM
Thank you for writing this. I’ve been on lithium for 18 years. I’ve had two hospitalizations because of brand switches I didn’t know about. I keep a binder: date, dose, brand, level, symptoms. It’s saved my life. If you’re on lithium, do this. Don’t wait for a crisis. Be your own advocate. You’re not a number. You’re not a cost-center. You’re someone who deserves to feel stable. And yes-it’s a lot of work. But you’re worth it.
Kenny Pakade
December 14, 2025 at 11:21 AM
Oh great. Another article telling me I can’t take ibuprofen. So what? I have a bad back. I take Advil. I’ve been doing it for 10 years. My levels are fine. You want me to switch to Tylenol? That’s worse for my liver. And now you’re telling me to test every time I take a pill? I’m not a lab rat. I’m a person. You’re turning a life-saving drug into a full-time job.
brenda olvera
December 16, 2025 at 02:25 AM
I’m from Mexico and I’ve been on lithium since I was 19. I moved to the US and my doctor here was shocked I was still on it. He said, ‘We don’t use that here anymore.’ But I feel better than I ever have. I’m a teacher. I raise two kids. I cook for my family. Lithium didn’t take away my emotions-it gave me the space to feel them without drowning. Don’t let anyone tell you it’s outdated. It’s a gift. Just don’t forget to drink water.
Myles White
December 17, 2025 at 09:36 AM
I’ve been thinking about this a lot lately. Lithium’s narrow therapeutic window is actually kind of beautiful in a way-it forces you to be present. You can’t just pop a pill and forget. You have to track your water intake, your kidney function, your thyroid, your sleep, your diet, your stress levels, your brand changes, your medication interactions… and honestly? That’s the real therapy. It’s not just the chemical. It’s the ritual. The discipline. The self-awareness. It turns you into a scientist of your own mind. And that’s something no new drug can replicate. We’re not just treating bipolar disorder-we’re cultivating a way of living.
olive ashley
December 18, 2025 at 10:43 AM
So you're telling me that after 20 years of taking lithium, I have to worry about whether my pharmacy switched me to a brand that releases lithium 20% faster? And I'm supposed to trust that my doctor is checking this? Please. My doctor doesn't even remember my name. I have to call three times to get a refill. And now I'm supposed to track my serum levels like a lab technician? No. I'm done. I'm switching to CBD gummies. At least they taste good.






Arjun Deva
December 7, 2025 at 07:12 AM
So let me get this straight… the government lets drug companies switch my lithium brand without telling me, and then I’m just supposed to trust that my brain won’t melt?!! I’ve been on this stuff for 12 years, and last year my pharmacy switched me to some generic I’d never heard of-next thing I know, I’m shaking like a leaf and vomiting in the bathroom at work… they didn’t even call me!!! This isn’t medicine-it’s Russian roulette with a prescription pad!!!