When a mole changes shape, color, or starts bleeding, most people panic. But panic won’t save you. What will? Knowing the difference between a harmless spot and something dangerous-and acting fast. Melanoma, the deadliest form of skin cancer, doesn’t wait. If caught early, the 5-year survival rate is over 99%. If it spreads? That number drops to just 32.1%. The gap isn’t luck. It’s detection. And treatment.
What Makes Melanoma So Dangerous?
Melanoma starts in melanocytes, the cells that give your skin its color. Unlike basal or squamous cell cancers, which grow slowly and rarely spread, melanoma can move fast. It can go from a tiny spot to a life-threatening tumor in months. That’s why it accounts for only 1.8% of all skin cancers but causes most skin cancer deaths.
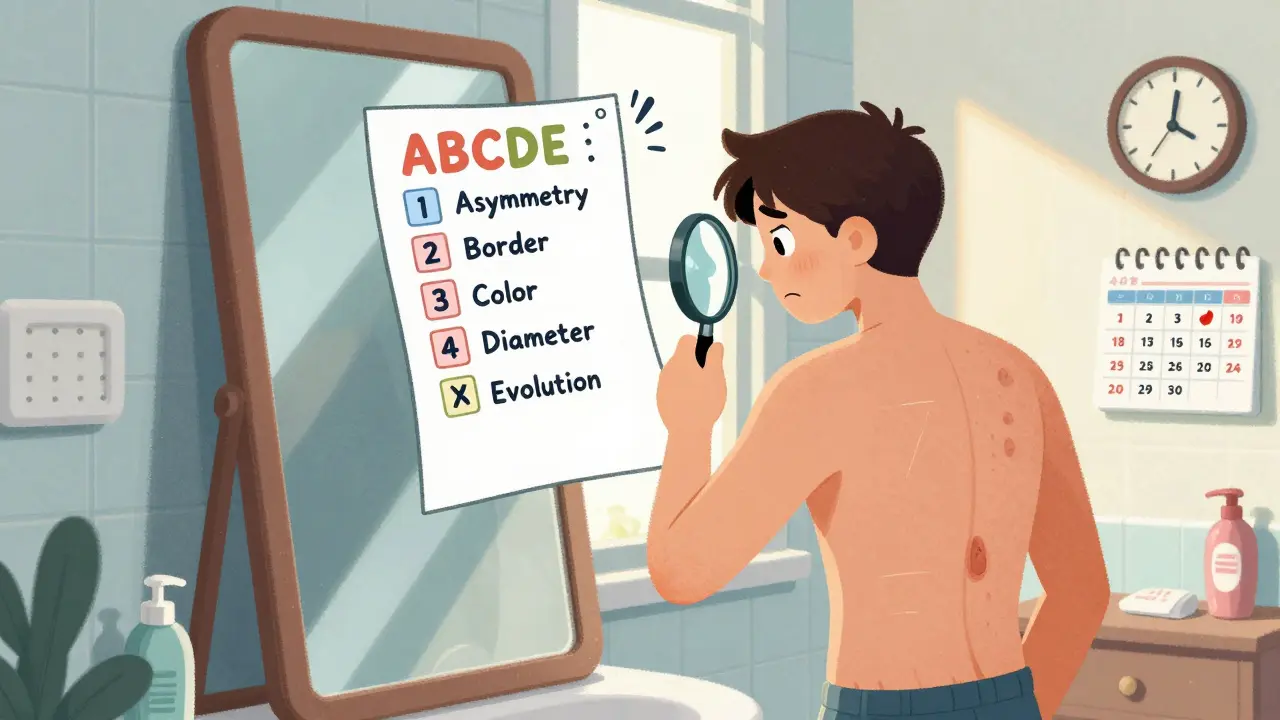
It’s not just about sunburns. Genetics, family history, and even certain moles play a role. A mole that’s asymmetrical, has uneven borders, varies in color, is larger than a pencil eraser, or changes over time? That’s the ABCDE rule-and it’s your first line of defense. But here’s the problem: most people don’t check themselves regularly. And even doctors miss up to 40% of melanomas during routine exams.
Early Detection: Beyond the Naked Eye
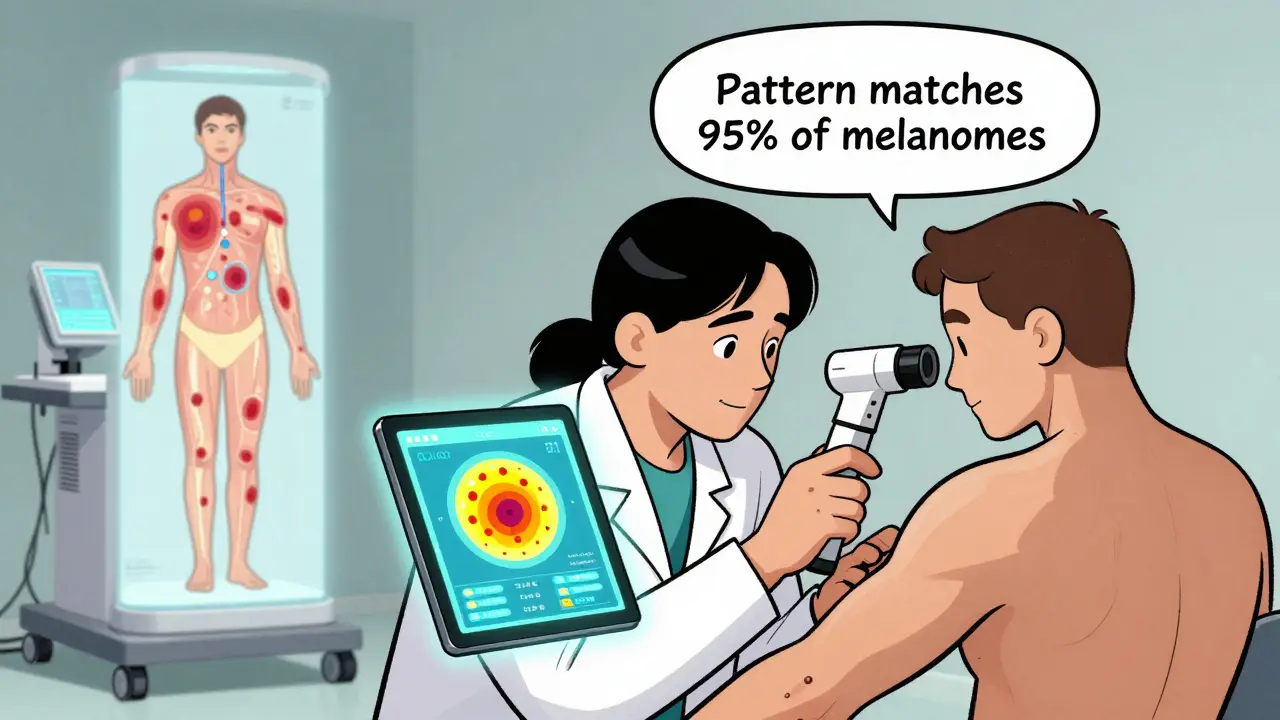
For decades, the only tool was a dermatologist’s eyes. Then came dermoscopy-a handheld magnifier that shows skin layers you can’t see normally. It helped. But not enough. Now, AI is stepping in.
At Northeastern University, researchers built SegFusion, a system that combines image segmentation and classification. It doesn’t just look at a mole. It isolates it, analyzes its edges, texture, and depth, then compares it to thousands of confirmed cases. Accuracy? 99%. Sensitivity? 95%. That means it catches nearly all real melanomas. And it’s not alone.
The iToBoS project, funded by the EU, uses a full-body scanner that takes six minutes to map every inch of your skin. It flags every suspicious spot, then uses explainable AI to show doctors why it flagged it. No black box. No guesswork. Just clear reasoning.
Then there’s DermaSensor, an FDA-approved device that shines near-infrared light on a mole. It measures how the light scatters-cancerous tissue reacts differently. Used by primary care doctors, it raised diagnostic confidence by 87%. But here’s the catch: its specificity is low. Only 26-40%. That means it flags a lot of harmless moles as dangerous. More biopsies. More stress. More cost.
And it’s not perfect for everyone. Studies show AI tools perform 12-15% worse on darker skin tones. Why? Because most training data came from lighter skin. This isn’t a glitch. It’s a gap. And it’s dangerous.
Wearables and At-Home Screening
What if you could check your skin every day without stepping into a clinic?
At Wake Forest, Dr. Mohammad J. Moghimi’s team developed a battery-free, wireless patch you stick on a mole. It measures electrical differences between healthy and cancerous tissue. In a small trial with 10 volunteers, it spotted clear differences. The patch is comfortable. It’s non-invasive. And it could one day let you monitor high-risk moles at home.
Early testers called it “comfortable.” But they also asked for better electrodes. The team is now testing conductive hydrogel to improve signal quality. Larger trials are coming. If it works, it could turn skin checks into a daily habit-like brushing your teeth.
Why AI Isn’t the Magic Bullet
AI tools are powerful. But they’re not replacements. They’re assistants. And they have limits.
First, they need clean, consistent images. Real-world photos? Uneven lighting. Bad angles. Moles on the back, scalp, or between toes? Many AI systems can’t see those. Clinical trials use ideal images. Real life doesn’t.
Second, false positives are a problem. DermaSensor’s low specificity means many people get unnecessary biopsies. That’s not just painful-it’s expensive. And it creates anxiety.
Third, integration is slow. Dermatology clinics report 15-20 hours of training just to use one AI system. Electronic health records don’t talk to these tools. Doctors have to copy-paste results manually. That’s not efficiency. That’s friction.
And then there’s regulation. The FDA takes 18-24 months to clear an AI diagnostic tool. Europe is faster-42 devices are CE-marked as of 2025. The U.S. has only 17. That gap slows access.
Immunotherapy: Turning the Body Into a Weapon
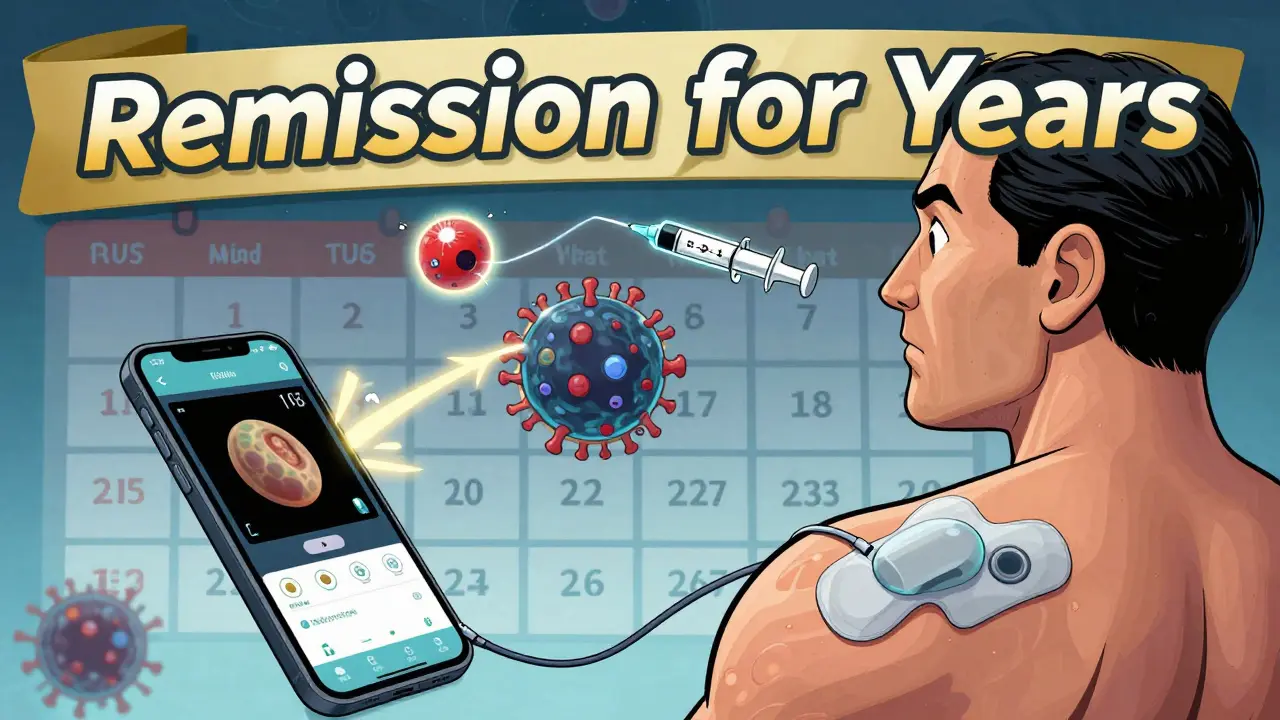
Once melanoma spreads, surgery and radiation often aren’t enough. That’s where immunotherapy changed everything.
In 2011, the FDA approved ipilimumab, the first drug to show it could extend life in metastatic melanoma. It worked by blocking CTLA-4, a protein that puts the brakes on immune cells. Suddenly, the body could fight back.
Then came PD-1 inhibitors-pembrolizumab, nivolumab. They work differently. They remove another brake. Now, the standard is combination therapy: anti-PD-1 + anti-CTLA-4. Together, they double response rates compared to single drugs.
And it’s getting better. Regeneron’s new combo-fianlimab (a LAG-3 blocker) plus a PD-1 drug-is showing even stronger results in early trials. IMA203, a cell therapy targeting PRAME proteins, achieved a 56% complete response rate in a Phase 1b trial. That means tumors vanished in more than half the patients.
These aren’t just drugs. They’re reprogramming the immune system. Some patients stay in remission for years. A few, maybe decades. That was unthinkable 15 years ago.
The Human Side: Overdiagnosis and Fear
But there’s a dark side to early detection.
Some melanomas grow so slowly they’d never harm you. Detecting them doesn’t save life-it just adds stress. A 2025 study in Taylor & Francis warned that screening might cause more harm than good by overdiagnosing harmless lesions. Unnecessary biopsies. Scar tissue. Anxiety. All for a cancer that might never have mattered.
Patients on Reddit are split. 62% love AI tools. 38% worry about privacy. Full-body scanners? They feel like surveillance. And they’re right to ask: Who owns this data? Could insurers use it?
Doctors are caught in the middle. They want to catch cancer early. But they don’t want to turn healthy people into patients.
What’s Next?
The future isn’t one tool. It’s a system.
Imagine this: You wear a patch that monitors your moles daily. Your phone app alerts you if something changes. You visit your doctor. They use a handheld scanner that reads the patch data and combines it with a dermoscopy image. The AI cross-checks it with your genetic risk profile and family history. It flags a spot. The system explains why. You get a biopsy. If it’s melanoma, you start immunotherapy within days.
That’s not sci-fi. It’s coming. By 2030, Deloitte predicts 89% of clinics will use AI-assisted detection. Mayo Clinic and Cleveland Clinic are already there. They’ve cut unnecessary biopsies by nearly a third.
The goal isn’t perfect detection. It’s smart detection. Early enough to save lives. Accurate enough to avoid harm. And personalized enough to match your risk.
What You Can Do Today
You don’t need AI to save your life. You need awareness.
- Check your skin monthly. Use a mirror. Look for moles that change.
- Know your ABCDEs: Asymmetry, Border, Color, Diameter, Evolution.
- See a dermatologist yearly if you have many moles, fair skin, or a family history.
- Don’t ignore new spots after age 40.
- Wear sunscreen daily. UV damage adds up.
If you’re high-risk, ask your doctor about AI tools or wearable monitors. They’re not everywhere yet-but they’re getting closer.
Melanoma doesn’t care if you’re busy, scared, or skeptical. But you can care for yourself. And that’s the most powerful treatment of all.
Can melanoma be cured if caught early?
Yes. When melanoma is caught before it spreads beyond the skin, the 5-year survival rate is over 99%. Early-stage melanoma is usually removed with a simple outpatient procedure. No chemotherapy. No radiation. Just surgery-and a high chance of full recovery.
How accurate are AI tools for detecting melanoma?
Top AI systems like SegFusion and DenseNet-201 achieve 94-99% accuracy on controlled image datasets. But real-world performance drops slightly due to lighting, skin tone, and image quality. Most FDA-cleared tools have sensitivity above 90% but specificity between 26-87%. That means they’re great at finding melanomas but sometimes flag harmless moles too.
Is immunotherapy better than chemotherapy for melanoma?
For advanced melanoma, yes. Chemotherapy rarely works well against melanoma. Immunotherapy, on the other hand, trains the immune system to attack cancer cells. It’s more effective, longer-lasting, and often has fewer side effects than chemo. Combination immunotherapy (like PD-1 + CTLA-4 blockers) is now the first-line standard for metastatic disease.
Do I need a biopsy if an AI tool flags a mole?
Yes. No AI tool, no matter how accurate, can replace a biopsy. AI can raise suspicion-but only a pathologist examining tissue under a microscope can confirm melanoma. AI is a triage tool, not a diagnosis tool. Always follow up with a dermatologist.
Are these new detection tools covered by insurance?
Most standard skin exams and biopsies are covered. But newer tools like DermaSensor or wearable patches are still emerging. Coverage varies by insurer and state. Some Medicare Advantage plans and private insurers are starting to cover AI-assisted screenings, especially if ordered by a dermatologist. Check with your provider before using new tech.
Can people with darker skin get melanoma?
Yes. While melanoma is less common in darker skin tones, it’s often diagnosed later-and more deadly. It tends to appear on palms, soles, under nails, or in the mouth. AI tools trained mostly on light skin may miss these. Everyone should check all areas of their skin, not just sun-exposed ones. Don’t assume you’re immune.
How long does immunotherapy last?
Treatment usually lasts 1-2 years, depending on response and side effects. But the effects can last much longer. Some patients remain in remission for over a decade. Unlike chemo, immunotherapy doesn’t kill cancer cells directly-it helps your body keep fighting them long after treatment ends.
11 Comments
Joni O
January 19, 2026 at 02:33 AM
i just started using a little app that reminds me to check my moles every sunday. it’s kinda dumb but it works 😅 i used to forget until i saw a friend’s post about melanoma and now i’m scared but also proactive. my dermatologist said i’m doing great. pls do this. your skin remembers everything.
Robert Davis
January 19, 2026 at 21:28 PM
Let’s be real-AI isn’t saving lives. It’s just making doctors richer. DermaSensor flags half your moles as cancer. You end up with scars you didn’t need, bills you didn’t ask for, and anxiety you didn’t sign up for. And don’t get me started on the training data being 90% white skin. My cousin with dark skin got told his melanoma was a ‘freckle’ for two years. AI doesn’t fix bias. It automates it.
And immunotherapy? Sure, it works for some. But the side effects? Autoimmune hell. I know a guy who lost his thyroid, his kidneys, and his sanity on it. People act like it’s magic. It’s not. It’s a gamble with your body.
Ryan Otto
January 20, 2026 at 11:57 AM
It is not merely a medical issue-it is a systemic orchestration of pharmaceutical and technological hegemony. The FDA’s 18–24 month approval window? A deliberate bottleneck to preserve market exclusivity. The EU’s 42 CE-marked devices? A regulatory farce designed to export liability. And the wearable patches? Surveillance capitalism disguised as prevention. Your biometric data is being harvested, monetized, and sold to insurers before you even blink. This is not healthcare. It is bio-surveillance under the guise of salvation.
Selina Warren
January 22, 2026 at 09:45 AM
What if the real cure isn’t in the algorithm or the drug-but in the way we stop treating our bodies like machines to be fixed? We’re scared of moles because we’ve been taught to fear our own skin. We don’t live in it. We inspect it. We judge it. We panic at every freckle. Maybe we need to stop trying to control every cell and start listening to the whole person. Healing isn’t just a biopsy. It’s peace.
Jay Clarke
January 23, 2026 at 13:39 PM
AI is the new placebo. You press a button, it says ‘probably fine,’ and you feel better. Meanwhile, real doctors are getting lazy. Why think when an app can do it? And don’t even get me started on the ‘daily patch’ nonsense-next they’ll be selling us melanoma-tracking smart underwear. 🤡
Praseetha Pn
January 24, 2026 at 09:49 AM
Y’all are missing the BIG PICTURE. These AI tools? They’re not for you. They’re for the rich. The poor? Still getting told ‘it’s just a rash’ by overworked docs who can’t even afford the software. And the data? Oh honey, your skin scan is already on some dark web forum. I saw a leak last year-12 million dermatology images, labeled with names, addresses, even Socials. This isn’t medicine. It’s a data goldmine. And you’re the cow.
Dayanara Villafuerte
January 26, 2026 at 02:19 AM
My abuela used to say, ‘If it itches, check it. If it changes, run.’ 🙏 No AI needed. Just eyes, a mirror, and a little courage. Also, sunscreen isn’t optional-it’s your daily armor. SPF 50, every. single. day. Even when it’s cloudy. Even when you’re inside. I’m 42, no melanoma, and I owe it to my mom’s stubbornness. You got this 💪🌞
Stacey Marsengill
January 26, 2026 at 17:06 PM
I used to think I was immune because I’m brown. Then I got a melanoma on my sole. No sun exposure. No family history. Just… there. And the doctor laughed. Said it was ‘plantar wart.’ Took six months to get a biopsy. Six months. Now I’m in remission. But I’ll never trust a ‘normal’ exam again. If you’re not getting a full-body scan yearly, you’re gambling with your life.
Danny Gray
January 26, 2026 at 19:43 PM
Is it possible that the obsession with early detection is just another form of modern martyrdom? We turn our bodies into crime scenes, scanning every freckle like it’s evidence in a trial we didn’t consent to. What if some cancers aren’t meant to be found? What if the body knows better than the algorithm? We chase survival so hard we forget how to live-with imperfection, with uncertainty, with the quiet dignity of not knowing.
Eric Gebeke
January 27, 2026 at 00:43 AM
Wow. Just… wow. All this tech and we still can’t fix the fact that people won’t wear sunscreen. You don’t need AI. You need discipline. You need to stop being lazy. I’ve been using SPF 70 every morning since I was 18. No melanoma. No biopsies. No drama. Just responsibility. If you’re reading this and you haven’t applied sunscreen today-you’re part of the problem.

Jake Moore
January 17, 2026 at 23:55 PM
Just had my annual skin check last week-dermatologist used a dermoscope and flagged a mole I’d been ignoring since college. Turned out to be Stage 1. No chemo, no radiation, just a quick excision. I’m alive because I listened. Don’t wait for a scare. Check yourself. Monthly. Use a mirror. Take pics. Track changes. It’s that simple.