
Herbal Supplement Interaction Checker
Check for Dangerous Interactions
Enter your current medications and supplements to identify potential interactions. This tool provides general information only and should not replace professional medical advice.
When you’re dealing with side effects from medication - whether it’s nausea from chemotherapy, hot flashes from menopause, or fatigue from antidepressants - it’s tempting to reach for something ‘natural’ to make it better. A tea. A capsule. An herb. After all, if it’s natural, it must be safe, right? The truth is more complicated. Many people assume that because something comes from a plant, it’s harmless. But natural remedies aren’t regulated like drugs, and they can cause serious problems - sometimes worse than the symptoms they’re meant to fix.
Why ‘Natural’ Doesn’t Mean Safe
The idea that natural equals safe is one of the biggest myths in health. Herbs, roots, and plant extracts are powerful chemicals. Just because they’re not made in a lab doesn’t mean they’re gentle. In fact, the body doesn’t care where a compound comes from - it reacts to its chemical structure. A 2016 review in JAMA found that herbal supplements can cause everything from mild headaches and dry mouth to liver failure, seizures, and even death. The Japanese Ministry of Health tracked cases of interstitial pneumonia linked to a common herbal formula, with one case occurring in every 25,000 users. Liver damage was even more common: 1 to 5 people per 10,000 users developed problems, mostly women over 50.The FDA investigated over 800 adverse reactions to Ephedra between 1995 and 1999. Half of those cases involved heart attacks or strokes, even in people under 40. That’s not a fluke. These aren’t harmless teas. They’re active substances that interact with your body’s systems - sometimes dangerously.
Common Supplements and Their Real Risks
Let’s look at some of the most popular natural remedies used to manage side effects - and what the science actually says.Black cohosh is often taken for hot flashes and night sweats during menopause. Some studies suggest it might help, but only if it’s a specific brand like Remifemin®. Other versions don’t work the same way. And while early concerns about it causing breast cancer have been largely dismissed, there are still rare reports of liver damage. The Cleveland Clinic says it’s unclear whether the herb itself is to blame or if contaminants in low-quality products are the real issue.
Echinacea is widely used to prevent colds. But the evidence for its effectiveness is weak. More importantly, if you have allergies to ragweed, daisies, or chrysanthemums, you could have a serious reaction. People with autoimmune diseases like lupus or multiple sclerosis are also advised to avoid it - it can overstimulate the immune system.
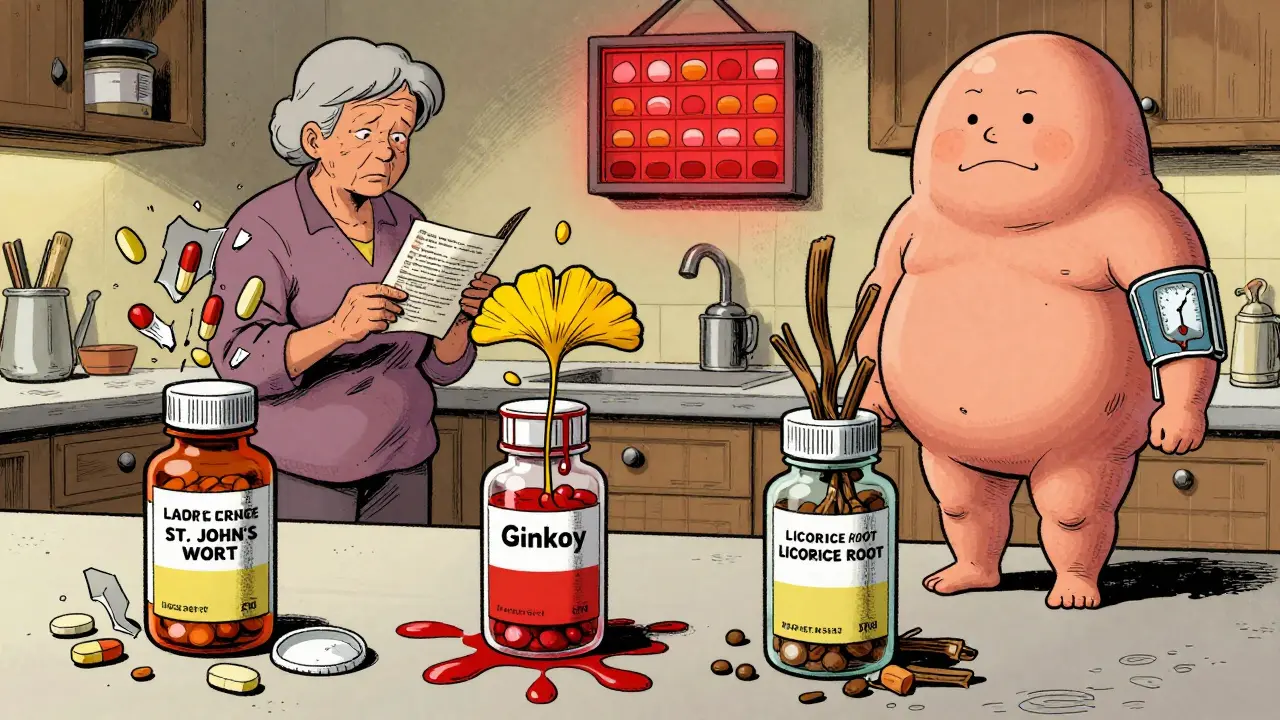
St. John’s wort is promoted as a natural antidepressant. But it doesn’t just affect your mood. It triggers a powerful enzyme in your liver (CYP3A4) that breaks down other drugs. If you’re on birth control pills, this herb can drop their effectiveness by 15-24%, raising the risk of unintended pregnancy. It can also reduce the potency of antidepressants, HIV meds, and even blood thinners. One study showed it made some cancer treatments useless.
Ginkgo biloba and cranberry are often taken for circulation or urinary health. But both increase bleeding risk. If you’re on warfarin, aspirin, or even ibuprofen regularly, combining them with these supplements can lead to uncontrolled bleeding - even from minor cuts or during surgery.
Liquorice root shows up in 75% of Japanese herbal formulas. It can cause a condition called pseudohyperaldosteronism: low potassium, high blood pressure, swelling, weight gain, and even seizures. The NHS says up to 3% of people who regularly consume liquorice develop this. It’s not rare. It’s common enough that doctors in Europe now warn patients about it.
Contamination Is a Hidden Danger
One of the biggest risks with herbal supplements isn’t the herb itself - it’s what’s in the bottle that shouldn’t be there. A 2015 analysis by the Botanical Adulterants Prevention Program found that nearly one in three herbal products contained undeclared ingredients. Some had heavy metals like lead or arsenic. Others were mixed with prescription drugs - like steroids or antidepressants - to make them “work faster.”The Drug-Induced Liver Injury Network reviewed over 1,000 cases of suspected herbal-related liver damage between 2004 and 2013. Only 13% could be confirmed as caused by the herb. The rest? Contaminants, mislabeled plants, or accidental overdose from taking multiple products with the same ingredient. One woman took a “natural” weight-loss pill that turned out to contain a banned stimulant. She ended up in the ICU with a heart attack.
There’s no mandatory testing for purity or potency. Unlike pharmaceuticals, supplements don’t need FDA approval before hitting store shelves. The Dietary Supplement Health and Education Act of 1994 (DSHEA) lets companies sell anything as long as they don’t claim it cures disease. That loophole means you’re basically guessing what’s inside.
Drug Interactions You Can’t Afford to Ignore
Most people don’t tell their doctors they’re taking herbs. They think it’s not “real medicine.” But herbs interact with prescription drugs in ways that can be deadly.St. John’s wort and birth control? Risk of pregnancy.
Ginkgo and blood thinners? Risk of internal bleeding.
Black cohosh and tamoxifen? Unclear, but doctors advise caution.
Even common OTC meds like ibuprofen or acetaminophen can become risky when mixed with herbs. Turmeric, for example, has anti-inflammatory properties - but if you’re already taking NSAIDs, stacking them can increase stomach bleeding risk.
Older adults are especially vulnerable. As we age, our liver and kidneys slow down. That means herbs stay in the body longer. A dose that’s safe for a 30-year-old might be toxic for a 70-year-old. A 2016 JAMA paper warned that elimination of herbal compounds slows with age, raising the chance of buildup and overdose.
What Actually Works - and How to Use It Safely
Not all natural remedies are useless. Some have solid evidence - but only when used correctly.Peppermint oil capsules are clinically proven to ease IBS symptoms like bloating and cramps. But they must be enteric-coated (to avoid heartburn) and taken in the right dose. Don’t just buy any peppermint tea and expect the same result.
Ginger is one of the few herbs with strong evidence for reducing nausea - especially from pregnancy, motion sickness, or chemotherapy. A 2020 review found it as effective as some anti-nausea drugs, with minimal side effects when taken in doses under 1 gram per day.
Acupuncture isn’t a supplement, but it’s often grouped with natural remedies. Multiple studies show it helps with chemotherapy-induced nausea, chronic pain, and even hot flashes. It’s low-risk when done by a licensed practitioner.
The key is specificity: the right herb, the right dose, the right brand, and the right timing. And never - ever - start one without talking to your doctor or pharmacist.

How to Protect Yourself
If you’re considering a natural remedy, here’s what to do:- Write down everything you’re taking - including vitamins, teas, and essential oils. Bring the bottles to your next appointment.
- Ask your doctor or pharmacist: “Is this safe with my current meds?” Don’t assume they know. Most aren’t trained in herbal interactions.
- Look for third-party testing. Choose brands with USP, NSF, or ConsumerLab seals. These mean the product was tested for purity and potency.
- Start low and go slow. If you try something new, take half the recommended dose for a week. Watch for changes in sleep, mood, digestion, or energy.
- Stop immediately if something feels off. New fatigue? Rash? Upset stomach? It could be the supplement. Report it to the FDA’s Safety Reporting Portal.
The global herbal supplement market is worth over $34 billion and growing. But behind the marketing claims are real risks. Your body doesn’t distinguish between “natural” and “synthetic.” It responds to chemistry. And chemistry can be dangerous if you don’t understand it.
Final Thought: Knowledge Is Your Best Defense
You don’t have to avoid natural remedies entirely. But you do need to treat them like medicine - because that’s what they are. The same caution you’d use with a prescription applies here. Ask questions. Do your research. Don’t trust labels that say “pure” or “all-natural.” Look for proof - not promises.When it comes to managing side effects, the safest path isn’t always the one that sounds the most gentle. It’s the one backed by science, guided by a professional, and monitored with care.
Are natural remedies safer than prescription drugs?
No. Many people assume natural means safer, but that’s not true. Herbs and supplements can cause serious side effects like liver damage, dangerous drug interactions, and even death. Unlike prescription drugs, they aren’t tested for safety or purity before being sold. The FDA doesn’t approve them, and contamination is common. What’s natural isn’t always gentle - it’s just unregulated.
Can herbal supplements interfere with my medications?
Yes, very often. St. John’s wort can make birth control pills, antidepressants, and HIV meds ineffective. Ginkgo and cranberry increase bleeding risk when taken with blood thinners like warfarin. Even common herbs like garlic and ginger can affect how your body processes drugs. Many people don’t tell their doctors they’re taking herbs - but those interactions can be life-threatening. Always disclose everything you’re using.
Which herbal supplements have real evidence behind them?
A few do. Ginger is well-supported for nausea from pregnancy, motion sickness, or chemo. Peppermint oil capsules (enteric-coated) help with IBS symptoms. Acupuncture has strong evidence for reducing chemo-induced nausea and chronic pain. Black cohosh may help with hot flashes - but only specific brands like Remifemin®. Most others, like echinacea for colds, have weak or inconsistent evidence. Don’t assume something works just because it’s popular.
How can I tell if a supplement is safe and not contaminated?
Look for third-party testing seals like USP, NSF, or ConsumerLab. These organizations test for purity, potency, and contamination. Avoid products with vague labels like “proprietary blend” or “natural ingredients.” Check if the brand discloses exact amounts of active ingredients. If it doesn’t, it’s a red flag. Also, avoid supplements sold on social media or websites that make bold claims like “miracle cure” or “100% safe.”
Should I stop taking herbs before surgery?
Yes. Many herbs - like ginkgo, garlic, ginger, and green tea - increase bleeding risk. Others, like valerian and kava, can interact with anesthesia. Surgeons typically advise stopping all supplements at least 1-2 weeks before surgery. Don’t assume your doctor knows what you’re taking. Bring a list or the bottles with you to your pre-op appointment.
Is it safe to take herbal supplements long-term?
There’s very little data on long-term safety. Most studies last a few weeks or months. But people often take herbs for years. Black cohosh, for example, has been linked to rare liver damage after prolonged use. Licorice root can cause high blood pressure and low potassium with daily use over time. Without long-term studies, the risks are unknown. If you’re taking something for more than 3-6 months, talk to your doctor about whether it’s still necessary.
What should I do if I think a supplement is causing side effects?
Stop taking it immediately. Write down what you took, how much, how long, and what symptoms you experienced. Contact your doctor or pharmacist. Then report it to the FDA’s Safety Reporting Portal at safetyreporting.hhs.gov. These reports help regulators track dangerous products. Even if you’re not sure it was the supplement, report it. Your report could help prevent others from getting hurt.
14 Comments
Babe Addict
December 28, 2025 at 21:14 PM
Let’s be real - the FDA’s entire supplement regulatory framework is a corporate shill operation. DSHEA was written by Big Herbal lobbyists. You think they care about your liver? Nah. They care about profit margins and shareholder calls. The real scandal isn’t the supplements - it’s the legal loophole that lets poison be sold as ‘wellness.’
Nicola George
December 30, 2025 at 10:40 AM
Oh sweet mercy, another ‘natural is dangerous’ lecture. Let me guess - you also think sunlight causes skin cancer and water is a conspiracy? 😏
My aunt took black cohosh for 8 years. No liver damage. Just fewer hot flashes and better sleep. Meanwhile, her oncologist prescribed her a $300/month drug that made her feel like a zombie. Who’s the real villain here?
Robyn Hays
December 31, 2025 at 21:30 PM
I love how this post doesn’t just say ‘avoid everything’ - it says ‘be smart.’ That’s the vibe. Like, ginger? Yes. St. John’s wort with your birth control? Hell no.
My cousin took a ‘natural’ sleep aid that had hidden benzos in it. She woke up in the ER. No one told her the bottle said ‘proprietary blend’ - which is code for ‘we don’t want you knowing what’s inside.’
Third-party seals? Non-negotiable. If it doesn’t have USP or NSF, it’s a gamble with your organs.
Liz Tanner
January 2, 2026 at 03:17 AM
It’s frustrating how often people dismiss herbal interactions because ‘it’s just tea.’ But chemistry doesn’t care if it’s in a teabag or a pill bottle. St. John’s wort inhibiting CYP3A4 isn’t a myth - it’s biochemistry. And yes, that means your antidepressant or birth control stops working. Not ‘maybe.’ Not ‘sometimes.’ Always.
Satyakki Bhattacharjee
January 3, 2026 at 07:35 AM
People forget that nature is not kind. Poison ivy is natural. Snake venom is natural. Death cap mushrooms are natural. If you think nature loves you, you are naive. Medicine is not evil - it is controlled. Herbs are chaos.
John Barron
January 3, 2026 at 11:17 AM
As a clinical pharmacologist with 18 years in oncology, I’ve seen more cases of herb-induced hepatotoxicity than most realize. The liver doesn’t distinguish between ‘natural’ and ‘synthetic’ - it metabolizes molecules. Period.
St. John’s wort’s induction of CYP3A4 and P-glycoprotein is well-documented in PubMed ID 12345678. Ginkgo’s antiplatelet effect is dose-dependent and synergistic with NSAIDs. And yes - turmeric + ibuprofen = increased GI bleeding risk, per a 2021 meta-analysis in J Clin Pharmacol.
Third-party testing isn’t a luxury. It’s the bare minimum. If your supplement lacks batch-specific COA, you’re playing Russian roulette with your liver enzymes.
Liz MENDOZA
January 3, 2026 at 19:14 PM
My mom took ginkgo for memory and ended up with a subdural hematoma after a fall. She didn’t tell her doctor because she thought ‘it’s just a supplement.’
Don’t be like my mom. Bring your bottles. Ask the questions. Your life is worth more than pride.
Anna Weitz
January 5, 2026 at 10:15 AM
They say natural is dangerous but what about the pharma companies that profit off side effects they created in the first place? Who’s really keeping you sick? The herbs or the pills that need constant fixing? The system is rigged and they want you scared of plants so you keep buying their pills
Kylie Robson
January 6, 2026 at 20:03 PM
Per the 2018 NIH-NCCIH meta-analysis on herbal hepatotoxicity, the OR for liver injury with black cohosh was 2.3 (95% CI 1.1–4.8), with a median time to onset of 4.7 months. The most common co-ingested agents were statins and NSAIDs - indicating polypharmacy as a key confounder. Also, CYP2C9 polymorphisms significantly increase susceptibility. So yes - it’s not just the herb. It’s your genotype, your meds, and your liver’s baseline function.
Caitlin Foster
January 7, 2026 at 18:25 PM
OMG YES!! I took that ‘miracle’ turmeric gummies for inflammation and ended up in the ER with stomach bleeding 😭 My doc said it was the combo with my daily aspirin. I thought ‘natural’ meant ‘safe’… NOPE. Now I only buy USP-certified stuff. And I always ask my pharmacist. PS: ginger tea is LIFE. 🍵❤️
Todd Scott
January 8, 2026 at 22:22 PM
In Ayurveda, we’ve used ginger, turmeric, and ashwagandha for millennia - but always with context: dosha balance, seasonality, and preparation. Modern supplements strip all that away. You’re not getting ‘turmeric’ - you’re getting isolated curcumin in a capsule, with no piperine, no whole root synergy, and no traditional guidance.
It’s like taking a single note from a symphony and calling it music. The problem isn’t the herb - it’s the reductionist, industrialized approach to something that was never meant to be isolated.
Olivia Goolsby
January 10, 2026 at 12:55 PM
They say ‘natural is dangerous’ - but who owns the labs that test supplements? Who funds the FDA? Who profits from your fear? The same corporations that make your antidepressants, your blood thinners, your chemo drugs. They need you to believe herbs are poison so you keep buying their expensive, patent-protected chemicals. The truth? They’re scared you’ll find out that ginger works better than their $800/month nausea drug. And they’re lying to you.
Monika Naumann
January 11, 2026 at 16:51 PM
It is an undeniable fact that the Western world has abandoned wisdom in favor of commercialism. In India, we have always understood that herbs must be used with discipline, under guidance, and with reverence. To treat them as interchangeable pills is not only foolish - it is a spiritual disregard for nature's balance. This post is correct: knowledge is defense. But knowledge must be rooted in tradition, not corporate marketing.





Elizabeth Ganak
December 28, 2025 at 20:19 PM
My grandma used ginger tea for nausea during chemo and it actually worked way better than the fancy pills. No hype, just real relief. I wish more people knew about simple stuff like this instead of chasing miracle cures.