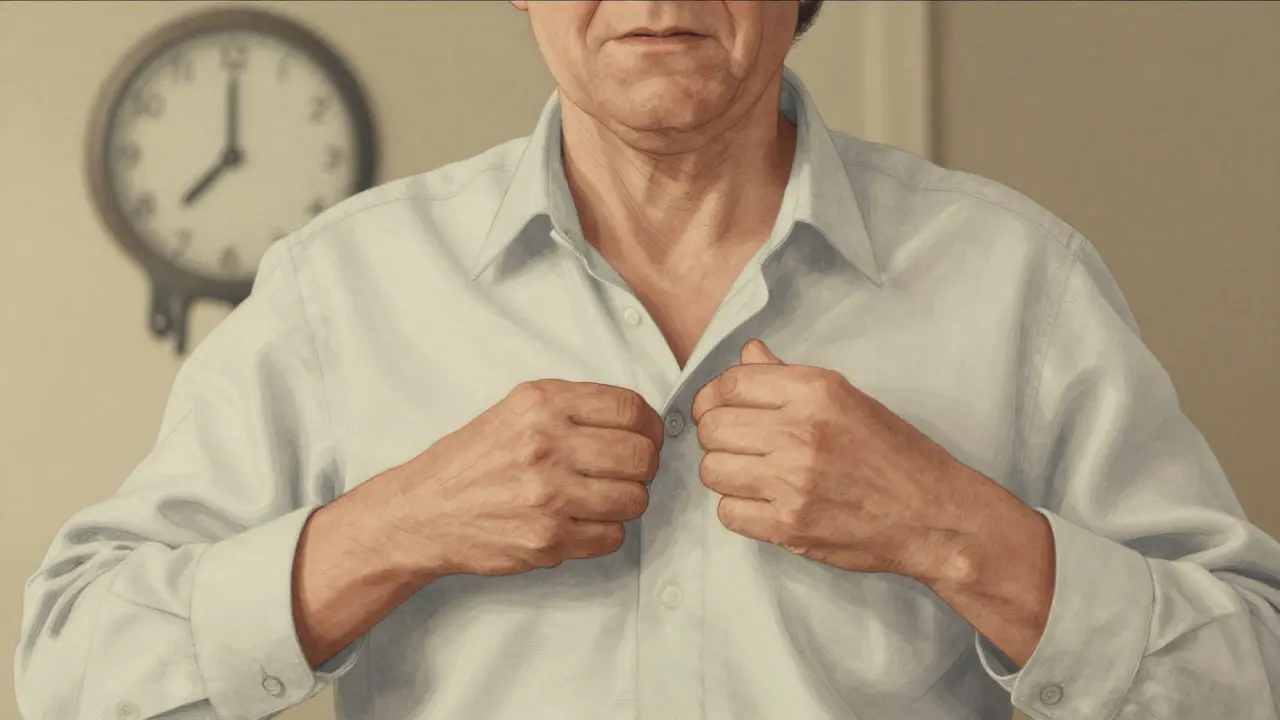
Living with Parkinson’s disease means learning to navigate a body that no longer moves the way it used to. It’s not just about shaking hands or slow steps-it’s about the quiet, daily battles: struggling to button a shirt, forgetting how to turn over in bed, or realizing your voice has gotten so soft that your family has to lean in just to hear you. This isn’t a sudden change. It’s a slow, steady shift that creeps in over years, reshaping everything from how you walk to how you connect with the people around you.
What Are the Core Motor Symptoms?
Doctors don’t diagnose Parkinson’s based on one symptom. They look for a pattern. The four cardinal signs are bradykinesia, rigidity, tremor, and postural instability. Of these, bradykinesia-slowness of movement-is the one you can’t miss. If you have Parkinson’s, this symptom is always there. Even if your hands don’t shake, even if your muscles don’t feel stiff, if your movements have slowed down, it’s a red flag.
Tremor is what most people picture: a rhythmic shaking, often starting in one hand, like rolling a pill between thumb and finger. About 70% of people notice this first. But here’s the twist: 20-30% of patients never develop a tremor at all. That’s why relying on shaking alone can delay diagnosis. Rigidity feels like your muscles are stuck in concrete. Some describe it as a jerky resistance-like a cogwheel turning-while others feel constant stiffness, like a lead pipe. About 85% of people have the cogwheel type.
Postural instability shows up later, usually after five to ten years. It’s not just feeling unsteady. It’s the sudden, terrifying moment when you reach for something and your body doesn’t respond fast enough. You lurch forward. You stumble. That’s why falls are so common-nearly 7 out of 10 people with Parkinson’s fall at least once a year.
How Medications Work-and Where They Fall Short
The goal of treatment is simple: replace the dopamine your brain is losing. Levodopa, first used in 1967, is still the most effective drug. It crosses into the brain and turns into dopamine. For most people, it works wonders in the beginning. Around 70-80% see big improvements in movement, stiffness, and tremor.
But here’s the catch: after five years, about half of people start having problems. Their medication stops working as smoothly. One minute they’re moving fine, the next they’re frozen. This is called “on-off” fluctuation. Or worse, they develop dyskinesias-uncontrollable, dance-like movements. These aren’t side effects you can ignore. They can be as disabling as the original symptoms.
That’s why doctors often start younger patients on dopamine agonists like pramipexole or ropinirole. These mimic dopamine without turning into it. They’re not as powerful as levodopa, but they delay the onset of motor complications. About half of early-stage patients get good control with them. But they come with their own risks: nausea, dizziness, and sometimes sudden sleep attacks or compulsive behaviors like gambling or shopping.
After ten years, about 30% of people become candidates for deep brain stimulation (DBS). This isn’t a cure. It’s a reset button for your brain’s movement circuits. A surgeon implants electrodes into specific areas of the brain and connects them to a pacemaker-like device in your chest. It doesn’t stop the disease-but it can smooth out the wild swings in movement caused by long-term medication use.

How Daily Life Changes-And What You Can Do
Small tasks become huge. Dressing takes 2.3 times longer. Buttoning a shirt? Three times longer. Your handwriting shrinks into tiny, cramped letters-micrographia. You notice it when you sign a check or write a note. You didn’t mean to do it. Your hand just did it on its own.
Walking changes too. Your arms don’t swing anymore. That’s not just a quirk-it’s a balance problem. Without that natural counterweight, your body loses stability. Step length drops by 25-35%. Walking speed slows by 30-40%. You start shuffling. You hesitate before stepping off a curb. You don’t realize how much you rely on arm swing until it’s gone.
Speech gets quieter. Voice volume drops by 5-10 decibels. In a noisy room, you’re effectively silent. People ask you to repeat yourself. You stop trying. You withdraw. About 89% of people develop a soft voice, and 74% get slurred speech. Swallowing becomes harder. Food sticks. You choke. Drooling becomes common because you’re not swallowing as often. Around 50-80% deal with it.
Turning over in bed? That’s a struggle for 65% of people within five years of diagnosis. Getting up from a chair? You need to push off with your arms. Standing up takes two tries. Your body remembers how to move-but your brain can’t send the signal fast enough.
Non-Medical Support Makes a Real Difference
Medication can’t fix everything. That’s where physical therapy, speech therapy, and exercise come in. A 12-week program of targeted movement therapy can improve walking speed by 15-20% and cut fall risk by 30%. It’s not about lifting weights. It’s about retraining your body to move with rhythm and balance. Tai chi, dance, and even boxing classes have shown real benefits for people with Parkinson’s.
Speech therapy helps with volume and clarity. Techniques like the Lee Silverman Voice Treatment (LSVT) can boost voice strength by up to 10 decibels-enough to be heard across a room. Occupational therapy can restructure your home: installing grab bars, using adaptive utensils, switching to slip-on shoes. These aren’t luxuries. They’re lifelines.
And then there’s the emotional side. Depression affects up to 50% of people with Parkinson’s. Anxiety, sleep problems, fatigue-they all pile up. Sexual dysfunction affects half of male patients. These aren’t talked about enough. But they matter. They’re part of the disease, too.

What to Expect as the Disease Progresses
Parkinson’s doesn’t move at the same pace for everyone. Some decline slowly over 20 years. Others see faster changes. The Hoehn and Yahr scale breaks it into five stages:
- Stage 1: Symptoms on one side only-maybe a slight tremor or stiffness.
- Stage 2: Symptoms on both sides, but balance still okay.
- Stage 3: Loss of balance. Falls become common. Slowness increases.
- Stage 4: Severe symptoms. You can still stand or walk, but you need help.
- Stage 5: Wheelchair-bound or bedridden. You need full-time care.
Most people reach Stage 3 within five to seven years. Stage 5 can take a decade or more. But it’s not just about the scale. It’s about what you lose: independence, spontaneity, control.
What’s Not Being Told
No medication today stops Parkinson’s from progressing. All we have are tools to manage symptoms. Researchers are testing drugs that target alpha-synuclein, the protein that clumps in the brains of people with Parkinson’s. But so far, nothing has worked in large trials. That means your treatment plan today is your best defense-not a cure, but a shield.
And here’s the truth: Parkinson’s isn’t just a movement disorder. It’s a life-altering condition that touches every part of your existence. The tremor gets attention. The stiffness gets studied. But the silence? The isolation? The frustration of watching your own body betray you? Those are the real battles. And they’re the ones no pill can fix.
Is tremor always the first sign of Parkinson’s?
No. While tremor is the most common symptom at diagnosis-seen in about 70% of cases-it’s absent in 20-30% of people. Bradykinesia, or slowness of movement, is always present and is the most reliable early sign. Some people first notice stiffness, trouble getting out of a chair, or a loss of facial expression before any shaking occurs.
Can you live a normal life with Parkinson’s?
Yes, but "normal" changes. With the right combination of medication, therapy, and lifestyle adjustments, many people maintain independence for 10-20 years after diagnosis. You may need to adapt how you do things-using voice-to-text instead of typing, wearing Velcro shoes instead of laces, sitting down to dress-but you can still travel, work, socialize, and enjoy life. The key is early intervention and staying active.
Why does levodopa stop working over time?
Levodopa doesn’t stop working-it’s the brain’s response to long-term use that changes. As Parkinson’s progresses, dopamine-producing cells continue to die. The brain also becomes less able to store and release dopamine smoothly. This leads to "on-off" fluctuations, where the medication’s effect wears off too quickly, and dyskinesias, where too much dopamine causes uncontrolled movements. Adjusting doses, switching formulations, or adding other drugs can help manage this.
Are there alternatives to medication for managing symptoms?
Absolutely. Exercise is one of the most powerful tools. Studies show that regular physical activity-especially balance training, strength work, and rhythmic movement like dance or tai chi-can slow functional decline. Speech therapy helps with voice and swallowing. Occupational therapy makes daily tasks easier. And support groups reduce isolation. These aren’t supplements-they’re essential parts of care.
Does Parkinson’s shorten life expectancy?
Most people with Parkinson’s live as long as those without it. The disease itself isn’t fatal. But complications can be. Difficulty swallowing leads to aspiration pneumonia, which causes about 70% of Parkinson’s-related deaths. Falls, infections, and poor nutrition also contribute. Managing these risks-through swallowing therapy, fall prevention, and good nutrition-is just as important as taking your medication.
13 Comments
Karianne Jackson
February 8, 2026 at 21:02 PM
My grandma had this. She stopped talking. Just sat there. I didn’t get it until she tried to button her shirt and cried. That’s it. That’s Parkinson’s.
Brandon Osborne
February 9, 2026 at 06:26 AM
Ugh. I’ve heard this exact story 12 times. You think dopamine replacement is magic? It’s not. It’s a band-aid on a ruptured artery. And don’t even get me started on DBS. Surgeons make it sound like a Tesla upgrade, but half the people I know end up with worse dyskinesias or speech that sounds like a robot on helium.
And don’t even get me started on ‘exercise helps.’ Like, yeah, dancing is cute. But when your legs are literally frozen in place and you can’t lift your foot off the ground, no amount of tai chi is gonna fix that. The system is broken. The drugs are outdated. We need real science, not feel-good blogs.
Chelsea Cook
February 10, 2026 at 08:31 AM
LOL ‘exercise helps’? Yeah, because nothing says ‘hope’ like being told to do yoga when you can’t stand up without using your arms like crutches. Real helpful, guys. 😏
But seriously-LSVT worked for my dad. He went from whispering to yelling ‘I’M FINE!’ at the grocery store. So yeah, some things actually work. Just not the ones the pharma companies want you to hear about.
Brett Pouser
February 12, 2026 at 00:40 AM
Just came back from Brazil where they’ve got these community-based rehab hubs-no fancy machines, just people helping each other move. One guy, 78, taught himself to walk again using a broomstick and a wall. No meds. No DBS. Just community. Maybe we’re over-medicalizing this too much? Not saying skip treatment, but maybe we’re missing the human piece.
Ken Cooper
February 12, 2026 at 02:35 AM
hey so i read this whole thing and i just wanna say… bradykinesia is the real villain here. like, tremor? yeah, it’s scary. but the fact that your brain just… forgets… how to move? that’s the nightmare. i had a friend who could still talk fine but couldn’t lift his spoon. for 3 months. he just stared at it. like it was alien. no one talks about that. it’s not about shaking. it’s about your own body becoming a stranger.
Monica Warnick
February 13, 2026 at 02:23 AM
Oh honey. You think you’ve seen suffering? Try being the one who has to watch the person you love forget how to smile. Not because they don’t want to. Because their face doesn’t listen anymore. That’s Parkinson’s. Not the tremor. Not the stiffness. The silence. The stillness. The way they look at you like you’re a ghost. And you’re the one who’s supposed to hold it all together.
I didn’t cry when she stopped walking. I cried when she stopped recognizing her own reflection.
Sam Dickison
February 13, 2026 at 23:52 PM
Levodopa doesn’t stop working-it’s the brain’s dopamine storage system that’s collapsing. Think of it like a leaky bucket. You keep pouring in water (levodopa), but the bucket’s got holes (dying neurons). The solution isn’t more water-it’s patching the holes. That’s why dopamine agonists help early. They’re slower, gentler refills. But once the bucket’s full of holes? DBS is the only thing that can bypass the system. Not a cure. A workaround. And honestly? It’s pretty damn brilliant.
Tatiana Barbosa
February 14, 2026 at 23:44 PM
Just want to say-non-medical support isn’t optional. It’s the backbone. My sister started doing dance therapy after her diagnosis. Not because she wanted to. Because her neurologist said ‘if you don’t move, you’ll lose it all.’ She hated it. Now? She teaches it. She says it’s the only time she feels like herself. Not the patient. Not the wife. Just… her.
And yes, depression is part of it. Not a reaction. A symptom. Like tremor. We treat the tremor. Why not the sadness? Why not the shame? Why not the grief?
Also-yes, 50% of men have sexual dysfunction. We need to talk about this. It’s not embarrassing. It’s neurochemical.
John McDonald
February 15, 2026 at 13:58 PM
Just want to say thank you for writing this. My dad’s at stage 4. He still walks, barely. But he can’t button his shirt. I used to do it for him. Now I just hand him the shirt and say ‘you got this.’ He cries. I cry. Then he does it. Slow. Messy. But he does it. That’s the win. Not the meds. Not the surgery. Just… showing up. Even when your body says no.
Joseph Charles Colin
February 17, 2026 at 04:19 AM
On the pharmacodynamics: the pulsatile dopamine delivery from oral levodopa is the root cause of LID (levodopa-induced dyskinesias). The brain’s striatal neurons develop supersensitivity due to erratic receptor stimulation. That’s why continuous dopaminergic stimulation (CDS) via pumps or extended-release formulations shows promise. DBS modulates the basal ganglia-thalamocortical circuit to override pathological oscillations. It’s not magic-it’s neuroengineering. But it’s the closest thing we have to a reset.
John Sonnenberg
February 19, 2026 at 01:39 AM
And yet… we still have no disease-modifying therapy. No one’s talking about alpha-synuclein. No one’s talking about the fact that we’ve been chasing dopamine for 50 years, and the disease keeps creeping forward. We’re managing symptoms like it’s a car with a flat tire and we’re just rotating the wheels. We need to fix the road. Not just the tire.
Tom Forwood
February 21, 2026 at 01:24 AM
my dad’s been on dbS for 3 years. he’s back to gardening. he’s back to laughing. he’s back to being my dad. it didn’t fix everything. but it gave him back the moments that mattered. not a cure. but a gift. and that’s more than most get.






Marie Fontaine
February 7, 2026 at 13:21 PM
Just wanted to say this post hit different. I’ve been watching my mom go through this for 8 years, and honestly? The part about turning over in bed got me. She doesn’t even talk about it anymore. Just stares at the ceiling like it’s a puzzle. No one talks about how exhausting it is to just exist in your own body anymore.
Also, LSVT voice therapy? Life-changing. We started it last year. Her voice isn’t loud, but now she can yell at the dog from across the room. Small wins.
Also also-yes to boxing classes. She hates it, but she shows up. That’s the win.
Love you all doing this work.