Bipolar Disorder Treatment: Medications, Risks, and What Actually Works
When it comes to bipolar disorder treatment, a long-term approach using medication to control extreme mood swings between mania and depression. Also known as manic depression, it’s not something you fix with willpower or therapy alone—most people need a stable mix of drugs to keep their brain chemistry in balance. The cornerstone of this treatment is mood stabilizers, medications designed to prevent highs and lows without causing sedation or emotional blunting. Lithium, valproate, and carbamazepine are the most common, but they’re not interchangeable. Each has its own risks, side effects, and interactions that can turn a safe plan into a medical emergency.
Take lithium, a simple salt that’s been used for decades to calm manic episodes and prevent depression. Also known as lithium carbonate, it’s effective—but it’s also one of the most dangerous drugs if your kidneys or sodium levels shift even slightly. That’s why common meds like NSAIDs (ibuprofen, naproxen) or diuretics (water pills) can spike lithium levels and cause toxicity. Symptoms? Tremors, confusion, vomiting, even seizures. You don’t need to avoid these drugs entirely, but you need to know the signs and get your blood tested regularly. The same goes for valproate and carbamazepine—they interact with birth control, antibiotics, and even grapefruit juice. One wrong combo can send you to the ER.
Antipsychotics like quetiapine or olanzapine are often added to mood stabilizers, especially during acute episodes. They help with agitation, hallucinations, or sleep issues, but they come with weight gain, drowsiness, and metabolic changes. Many people stop taking them because of side effects, not because they don’t work. The key isn’t finding the perfect drug—it’s finding the right combination that keeps you stable without wrecking your quality of life. That’s why tracking your symptoms, blood levels, and side effects matters more than any prescription alone.
You’ll find posts here that break down exactly how lithium interacts with everyday drugs, why some mood stabilizers are riskier than others, and what to do if your current treatment stops working. These aren’t theoretical guides—they’re based on real cases, real risks, and real patient experiences. Whether you’re newly diagnosed, struggling with side effects, or just trying to understand why your doctor changed your meds, this collection gives you the facts you need to ask better questions and stay safe.
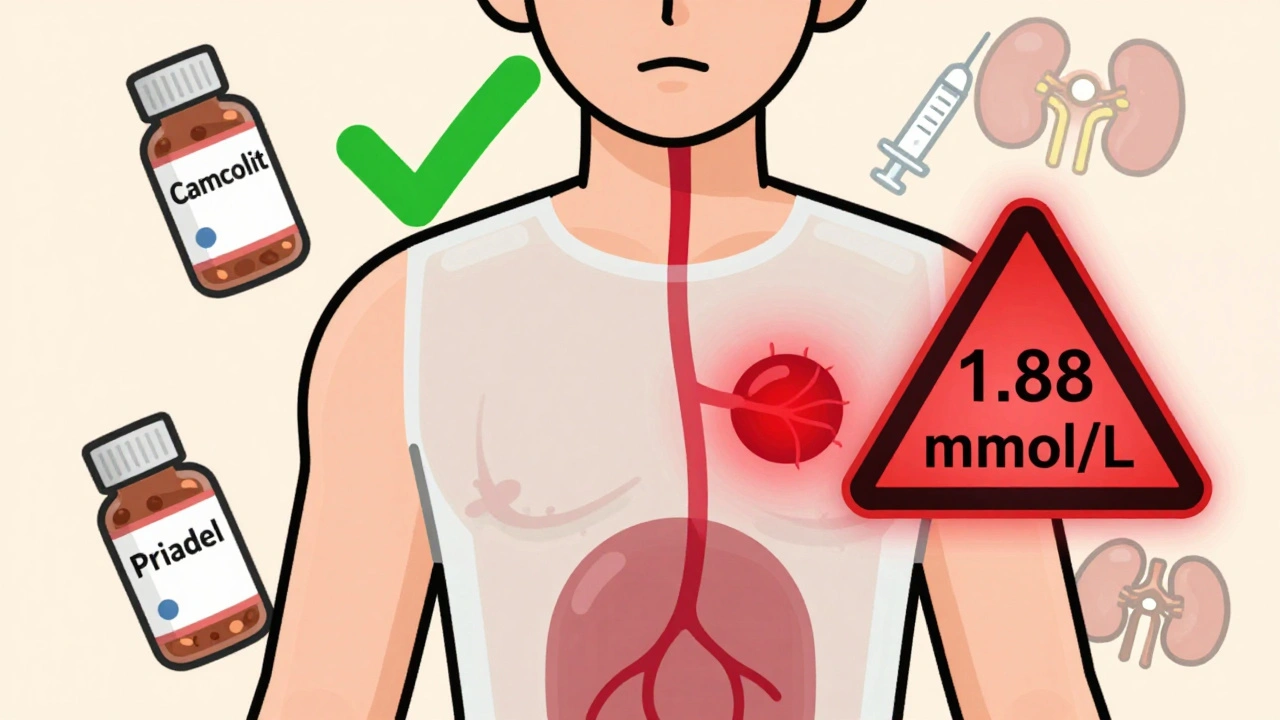
Lithium Carbonate Generics: What You Need to Know About Serum Levels
Lithium carbonate generics require careful serum level monitoring due to their narrow therapeutic range. Small differences between brands can affect blood levels, increasing risk of toxicity or treatment failure. Learn how to stay safe with proper testing and dosing.
View More




