Gut health: practical steps to feel better fast
Gut problems can wreck your day—bloating, loose stools, constipation, or that nagging stomach ache. You don’t need a medical degree to make real improvements. Small, specific changes to food, meds, and habits usually give the fastest wins. Below are clear, useful actions you can try today.
First, understand fiber. Not all fiber does the same job. Soluble fiber (oats, bananas, apples, psyllium) soaks up excess fluid and can help with diarrhea and recovery after gastroenteritis. Insoluble fiber (whole grains, nuts, raw vegetables) adds bulk and speeds transit, which helps with constipation but can irritate an already inflamed gut. If you’re recovering from stomach flu, start with small amounts of soluble fiber and avoid large portions of raw vegetables until things settle.
Everyday habits that help
Hydration matters. Drink plain water rather than sugary drinks. When you have diarrhea, sip oral rehydration solution or lightly salted water with a bit of sugar to replace lost salts. Move gently—short walks help digestion and reduce bloating. Eat regular meals and avoid large, late-night dinners that can trigger reflux or slow digestion.
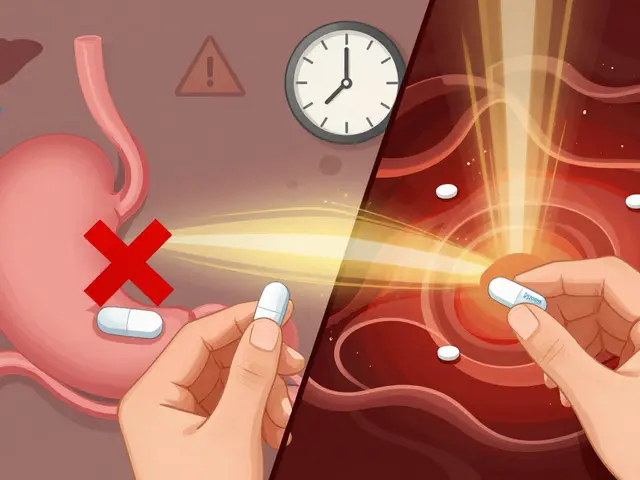
Use probiotics wisely. Foods like yogurt, kefir, and fermented vegetables can help restore balance after antibiotics or a stomach bug. If you try a supplement, look for Lactobacillus rhamnosus GG or Saccharomyces boulardii—both have good evidence for helping with diarrhea. If you’re taking antibiotics, take probiotics at least two hours apart from the antibiotic dose so the helpful bacteria have a chance to survive.
Watch how your meds affect your gut. Some medicines irritate the stomach or change bowel habits. For example, rifampin and other antibiotics can cause nausea and diarrhea—taking them with food often cuts down on nausea. If a prescription is giving you stomach pain, tell your doctor rather than stopping it on your own. They can suggest timing changes, protective foods, or switches to a gentler option.
When to act and when to see a doctor
If symptoms are mild and short, try the steps above for 48–72 hours. See a clinician sooner if you have high fever, bloody stool, severe dehydration (very little urine, dizziness), weight loss, or ongoing severe pain. For long-term issues like chronic constipation or repeated bloating, get a targeted plan—tests and simple med changes can make a big difference.
Use these practical tips as a starting point: adjust fiber type and amount, stay hydrated, try proven probiotics, and watch how medicines affect your gut. If home steps don’t help, get medical advice—quick fixes work best when they’re the right fix for your problem.
Related reads:
• Effective Fiber Use for Gastroenteritis Recovery and Prevention — how to pick and use fiber during recovery.
• Rifampin and Stomach Issues: Tips for Managing Gastrointestinal Side Effects — practical fixes if meds upset your stomach.

The Connection Between Gut Health and Vaginal Infections
In my latest research, I have discovered a fascinating connection between gut health and vaginal infections. It turns out that a balanced gut microbiome is essential for maintaining a healthy vaginal ecosystem. When our gut bacteria are thrown off balance, it can lead to an overgrowth of harmful bacteria and yeast, which may cause vaginal infections like bacterial vaginosis or yeast infections. So, taking care of our gut health through a balanced diet and possibly probiotics is crucial in preventing these uncomfortable infections. I will definitely be paying more attention to my gut health to ensure my overall well-being.
View More