Medicaid Formulary: What Drugs Are Covered and How It Affects Your Prescriptions
When you’re on Medicaid formulary, the official list of prescription drugs approved for coverage under your state’s Medicaid program. Also known as a drug list, it tells you exactly which medications your plan will pay for—and which ones won’t. This isn’t just a paperwork detail. It directly impacts whether you can fill your blood pressure pill, your antidepressant, or your insulin without paying hundreds out of pocket.
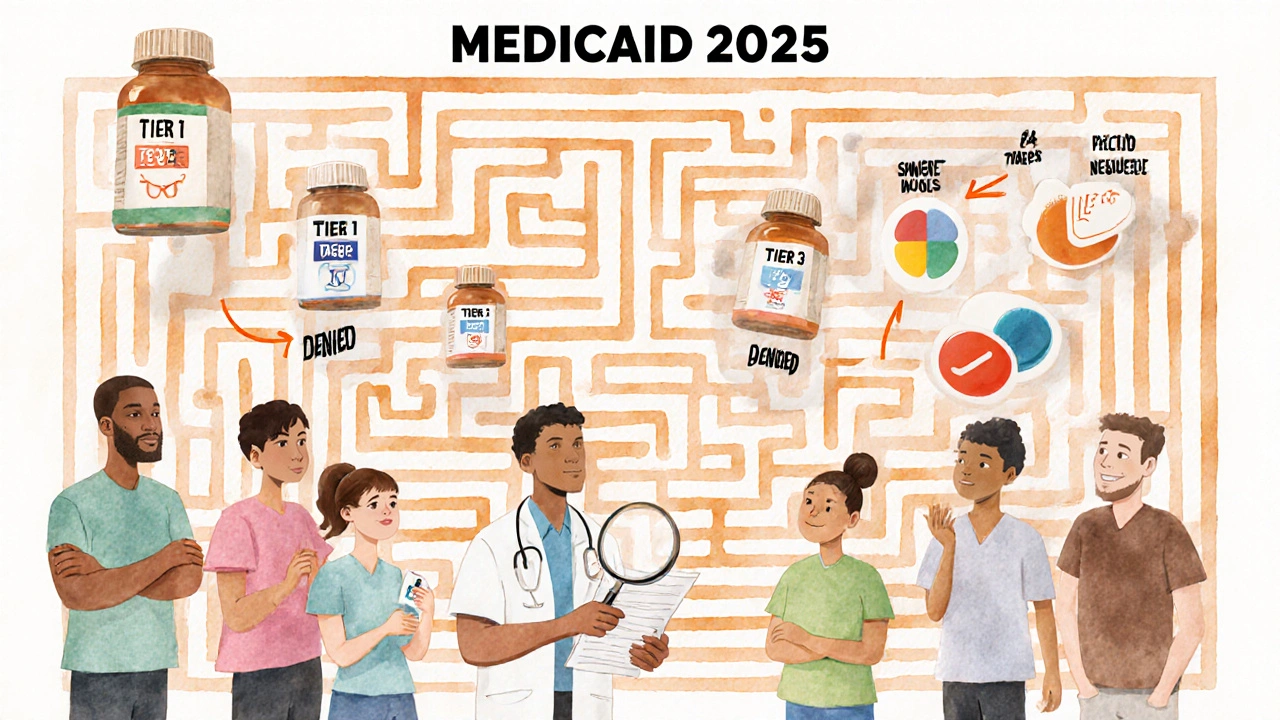
Each state runs its own Medicaid program, so the Medicaid formulary varies. Some states cover brand-name drugs only after you try cheaper generics first. Others block certain high-cost meds unless your doctor proves you’ve tried everything else. That’s where formulary restrictions, like prior authorization or step therapy, come in. You might need your doctor to call in a request just to get a drug approved. It’s not a glitch—it’s a system designed to control costs, but it often slows down care.
Many of the drugs listed in the posts below—like metoprolol, apixaban, Acamprosate, and Pravachol—are commonly included in Medicaid formularies because they’re proven, affordable, and widely used. But even these can be restricted. For example, some states require you to fail on atenolol before approving metoprolol. Others limit apixaban to patients with specific kidney function levels. And if you’re on a drug like promethazine, you might find it’s been replaced by safer alternatives like ondansetron on your formulary.
Knowing your formulary isn’t about memorizing lists. It’s about asking the right questions: Does my pharmacy accept my Medicaid plan? Is there a generic version? Do I need prior approval? What if I can’t afford the copay? The posts here cover real-world issues like drug interactions, side effects, and alternatives—exactly the kind of info you need when your formulary changes or denies a drug. You’ll find guides on how to navigate these systems, compare similar meds, and advocate for yourself without waiting weeks for approval.
Behind every denied prescription is a patient stuck between cost, access, and health. The Medicaid formulary isn’t perfect—but understanding it gives you power. These posts don’t just explain drugs. They show you how to get them, when to push back, and what to do when your plan says no.
Medicaid Coverage for Prescription Medications: What’s Included in 2025
Medicaid covers most prescription drugs, but coverage varies by state. Learn how formularies, step therapy, prior authorization, and Extra Help affect your out-of-pocket costs in 2025.
View More




