Medicaid Prescription Coverage: What’s Covered, Who Qualifies, and How to Save on Medications
When you rely on Medicaid prescription coverage, a state-run health program that helps low-income individuals pay for medical care, including medications. Also known as state Medicaid drug benefits, it’s one of the biggest sources of affordable prescriptions in the U.S., covering over 80 million people. But knowing what’s included — and what isn’t — can mean the difference between taking your meds and skipping them because you can’t afford them.
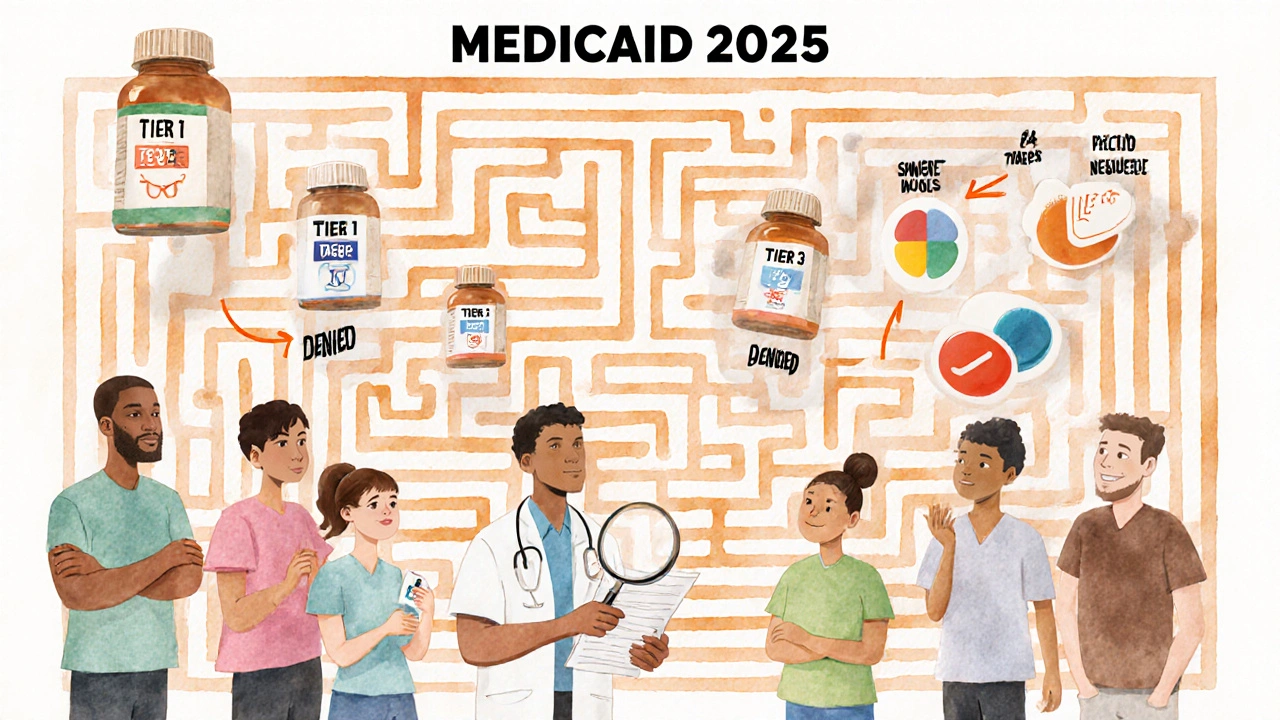
Not every drug is covered the same way. Medicaid plans have lists called formularies, official lists of approved medications that the program will pay for. Also known as drug lists, these vary by state and even by plan type. Some states require you to try cheaper generics first before approving brand-name drugs — a process called step therapy. Others limit how much of a drug you can get each month. And while most plans cover common meds like blood pressure pills, insulin, and antibiotics, some exclude certain psychiatric drugs, weight loss pills, or even popular generics if they’re deemed non-essential.
What you pay out of pocket also depends on your income. Many enrollees pay nothing. Others pay small copays — usually $1 to $5 for generics and up to $10 for brand names. But here’s the catch: some states don’t cover certain narrow therapeutic index drugs, medications where even tiny dosage changes can cause serious harm, like warfarin or lithium. Also known as NTI drugs, these often require special approval because they’re risky if not dosed exactly right. If you’re on one of these, your doctor may need to file paperwork just to get it approved — even if it’s the only thing that works for you.
And while Medicaid helps with generic drugs — which make up 90% of all prescriptions filled — it doesn’t always cover the cheapest version. Sometimes it picks a specific brand of generic, and if you want a different one, you might pay more. That’s why checking your plan’s formulary before filling a new prescription is critical. You can usually find it online through your state’s Medicaid site or by calling your pharmacy.
Medicaid also works with other programs. If you’re on Medicare too, you might qualify for Extra Help — a federal program that reduces out-of-pocket costs for Part D drugs. And if you’re not on Medicaid but still struggling to pay, some states offer patient assistance programs, free or low-cost drug programs run by manufacturers for people who can’t afford their meds. Also known as PAPs, these can cover everything from insulin to cancer drugs. You don’t need to be on Medicaid to qualify for these — just have a low income and a prescription.
What you’ll find in the posts below are real, practical guides on how Medicaid interacts with the drugs you actually take. From how anticoagulants like apixaban are covered to why some states restrict access to certain beta blockers like metoprolol, these articles cut through the confusion. You’ll see how the Hatch-Waxman Amendments made generics the norm — and why that matters when you’re on a fixed income. You’ll learn how to spot when a drug you need isn’t on your formulary, what to do next, and how to get help without waiting weeks.
This isn’t about theory. It’s about making sure you get the meds you need without breaking the bank — and knowing exactly where to look when things don’t go as planned.
Medicaid Coverage for Prescription Medications: What’s Included in 2025
Medicaid covers most prescription drugs, but coverage varies by state. Learn how formularies, step therapy, prior authorization, and Extra Help affect your out-of-pocket costs in 2025.
View More




