Medicaid Prior Authorization: What It Is, Why It Matters, and How to Navigate It
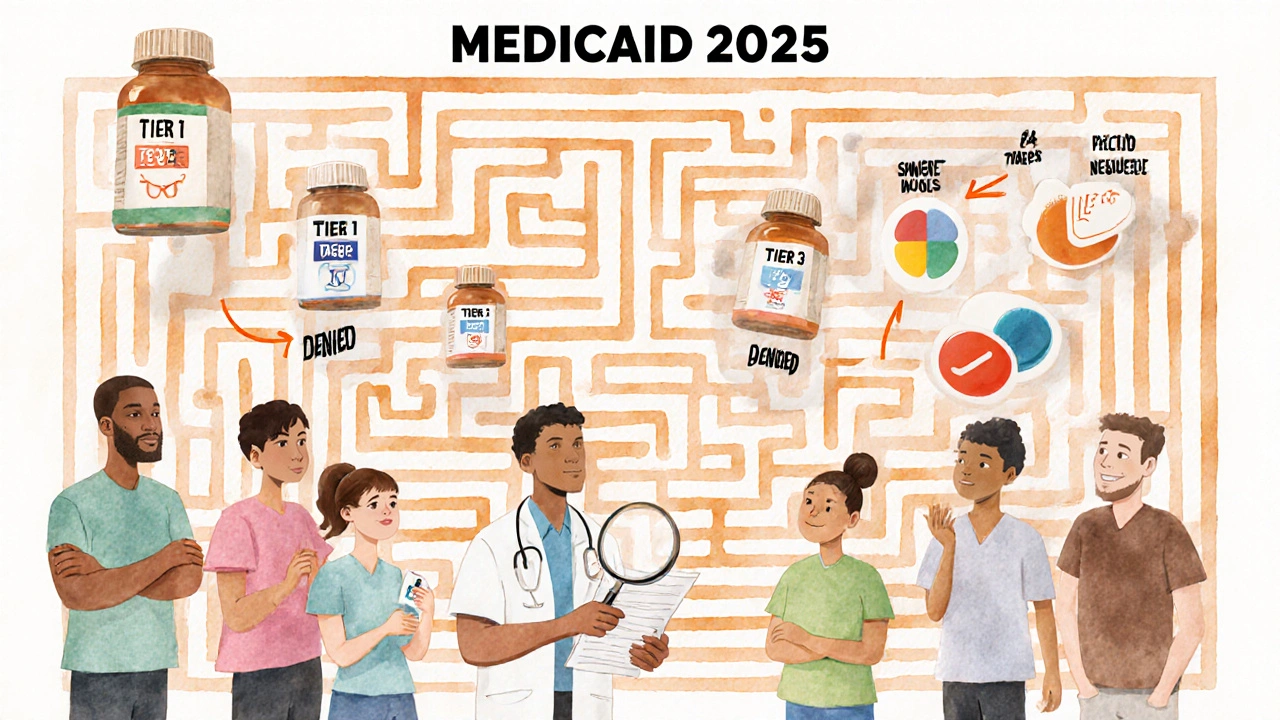
When you need a prescription covered by Medicaid prior authorization, a process where Medicaid requires approval before covering certain medications. Also known as pre-approval, it’s a gatekeeping step meant to control costs and ensure safe use—but for many, it’s a frustrating roadblock. You’re not alone if you’ve waited days or weeks for a simple drug to be approved. This isn’t about bureaucracy for bureaucracy’s sake. It’s about balancing affordability, safety, and access—especially for people managing chronic conditions like diabetes, epilepsy, or autoimmune diseases.
Medicaid prior authorization isn’t random. It targets drugs that are expensive, have safer alternatives, or carry high risk if misused. Think of it like this: if your doctor prescribes a brand-name drug when a generic works just as well, Medicaid will ask for proof that the cheaper option won’t work first. Or if you’re on a blood thinner like warfarin or apixaban, they may require documentation of lab tests before renewing the script. It’s not just about the drug—it’s about the prescription coverage, the rules that determine whether a medication is paid for by your plan. And it’s tied directly to Medicaid drug approval, the system that decides which drugs are covered under state-specific formularies. Each state runs its own rules, so what’s approved in Texas might be denied in New York—even for the same condition.
People with chronic illnesses often face the most hurdles. Someone on Medicaid prior authorization for a drug like omalizumab for chronic hives or acamprosate for alcohol dependence might need multiple forms, lab results, and even a letter from their doctor. It’s not just paperwork—it’s time lost, stress built up, and sometimes, treatment delayed. But there’s a way through. Know your rights. Ask your pharmacy to track the status. Keep copies of every form. And if your doctor says it’s medically necessary, push back. Many approvals happen only after an appeal. The system isn’t perfect, but it’s not unbeatable either.
Behind every approval denial is a story: a senior missing their blood pressure med because the form was lost, a parent waiting for their child’s seizure drug, or someone with liver disease stuck on an ineffective treatment because the better one needs pre-approval. These aren’t abstract policy issues—they’re daily realities. The posts below cover real cases where people fought for their meds, navigated drug interactions while waiting, or found alternatives when approval was denied. You’ll find guides on how to talk to your doctor about prior auth, what to do when a drug is pulled from the formulary, and how to spot when a denial is actually illegal under federal rules. This isn’t just about paperwork. It’s about getting the right medicine, on time, without the headache.
Medicaid Coverage for Prescription Medications: What’s Included in 2025
Medicaid covers most prescription drugs, but coverage varies by state. Learn how formularies, step therapy, prior authorization, and Extra Help affect your out-of-pocket costs in 2025.
View More




