Muscle spasms: quick relief, common causes, and what actually works
A muscle spasm is a sudden, involuntary contraction of one or more muscles. They can be mildly annoying or so painful they stop you in your tracks. Most often they come from simple, fixable things — dehydration, overuse, or low electrolytes — but sometimes they point to a deeper problem. Here’s a straight, practical guide to easing spasms now and preventing them later.
Fast home fixes that help right away
If a spasm hits, try these steps first. Gently stretch the tight muscle and hold the stretch for 15–30 seconds. Apply heat (warm towel or heating pad) to loosen the muscle, or cold if the area is sore or swollen. Massage along the muscle to increase blood flow. Drink water or an electrolyte drink — especially after sweating. Over-the-counter pain relievers like ibuprofen or acetaminophen can ease pain but won’t stop the spasm itself.
Simple foods can help restore minerals fast: a banana or orange for potassium, yogurt or milk for calcium, and nuts or seeds for magnesium. Some people find a short course of oral magnesium helps recurring nighttime leg cramps, but check with your doctor first if you take other meds or have kidney issues.
Why spasms happen — the usual suspects
These are the common causes you should check before worrying. Dehydration and low electrolytes (potassium, magnesium, calcium) are top reasons. Muscle overuse from a new workout, standing long hours, or holding an awkward position often triggers cramps. Poor circulation or a pinched nerve in the spine can cause spasms and sharp pain. Certain meds — statins, diuretics, some asthma drugs — may increase cramp risk.
Less common causes include thyroid problems, diabetes, or neurological issues. If spasms come with weakness, numbness, or loss of coordination, treat it as more than a cramp and get medical attention.
For frequent or severe spasms, your doctor may order blood tests (electrolytes, kidney function, thyroid), an EMG to check nerve function, or imaging if they suspect a disc problem.
If you need prescription muscle relaxants, options like cyclobenzaprine or tizanidine can help short-term. Benzodiazepines sometimes work but carry sedation risk. Use prescriptions only under a doctor’s guidance. If you buy meds online, pick a licensed pharmacy that requires a prescription and shows contact info and credentials.
Prevention is mostly common sense: stay hydrated, warm up before activity, stretch regularly (especially calves and hamstrings), improve posture, and balance electrolytes through food. If workouts trigger cramps, reduce intensity, add rest days, and gradually build strength.
If spasms are constant, getting worse, or come with weakness, fever, breathing trouble, or sudden swelling, seek immediate care. For ongoing but non-urgent issues, book a primary care visit — bring notes on when spasms happen, what helps, and any meds you take. That makes diagnosis faster and smarter.
Small changes usually fix most muscle spasms. Try the quick steps here, keep an eye on patterns, and ask a clinician when something feels off. That’ll get you moving again without needless worry.
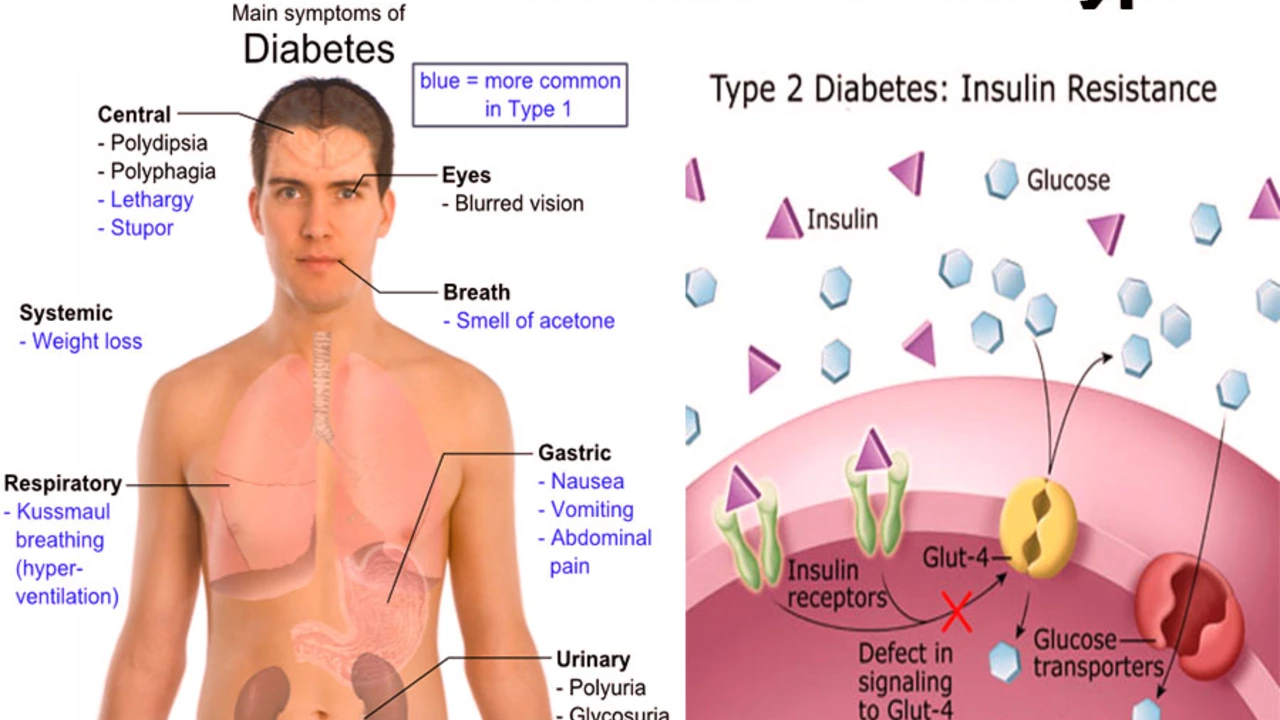
The connection between muscle spasms and diabetes
After delving into the topic, it's clear there's a notable connection between muscle spasms and diabetes. Muscle spasms, often experienced as a sudden, painful contraction, are frequently reported by individuals with diabetes. This connection can be attributed to the fluctuations in blood sugar levels that disrupt the balance of electrolytes in the body, leading to muscle cramps. Additionally, nerve damage caused by long-term diabetes, a condition known as diabetic neuropathy, can also trigger these spasms. So, it's pretty important for diabetics to manage their blood sugar levels effectively to avoid such discomfort.
View More




