Thyroid treatment: what works and how to stay safe
If your doctor told you your thyroid needs treatment, you probably want clear, useful steps — not medical jargon. This page explains common treatments for low and high thyroid function, how meds work, simple dosing rules, monitoring, and safety tips you can actually use.
Common medicines and how they behave
For hypothyroidism (low thyroid) the standard drug is levothyroxine. It replaces the missing hormone and usually fixes fatigue, weight gain, and slow thinking. The usual full replacement dose is about 1.6 mcg per kg of body weight per day. Older adults or people with heart disease start much lower (12.5–25 mcg) and go up slowly.
Liothyronine (T3) is faster acting and is sometimes added when symptoms persist despite normal tests, but it’s used carefully because it can cause heart palpitations and bone loss if overdone.
For hyperthyroidism (overactive thyroid) common options are antithyroid drugs like methimazole or propylthiouracil (PTU). Methimazole is usually preferred, while PTU is used in the first trimester of pregnancy or in thyroid storm. Other solutions include radioactive iodine or surgery when drugs aren’t enough or aren’t tolerated.
Practical dosing, testing, and safety tips
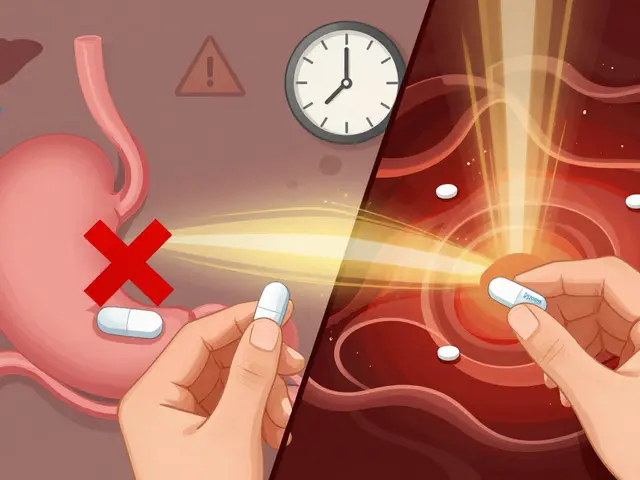
Take levothyroxine on an empty stomach — 30–60 minutes before breakfast or at bedtime 3–4 hours after your last meal. Avoid calcium, iron, and antacids within four hours of your dose; they reduce absorption. Soy and some high-fiber foods can interfere too.
Get your TSH checked about 6–8 weeks after starting or changing dose. Once stable, most people test every 6–12 months or sooner if symptoms change. If you’re pregnant, notify your doctor: many people need about a 30% increase in levothyroxine early in pregnancy.
Watch for signs of too much or too little hormone. Overreplacement can cause tremor, racing heart, anxiety, and long-term bone thinning. Underreplacement looks like fatigue, cold sensitivity, weight gain, and constipation. If you notice these, talk to your provider — don’t adjust doses yourself.
Be careful buying meds online. Use licensed pharmacies that require a prescription. If a site sells prescription thyroid medicine without asking for a prescription, it’s a red flag.
Supplements: don’t take iodine unless a doctor recommends it — too much iodine can worsen thyroid disease. Small studies show selenium may help certain autoimmune thyroid conditions, but talk to your clinician before starting supplements.
If symptoms are severe, you have chest pain, shortness of breath, or sudden changes in mood or thinking, seek medical care quickly. For routine care, an endocrinologist or a well-informed primary care doctor will guide safe, effective treatment tailored to your age, other health issues, and lifestyle.
Need more specific help with meds or monitoring? Ask your care team for a simple plan: target TSH range, when to test, and what to do if symptoms change. That keeps treatment safe and predictable.

Exploring Effective Alternatives to Synthroid for Thyroid Balance
Synthroid is a commonly prescribed medication for hypothyroidism, but it might not work for everyone. This article explores nine viable alternatives for thyroid management, each with its unique advantages and disadvantages. From natural desiccated options like Armour Thyroid to synthetic choices such as Cytomel, readers can find information helpful for navigating their treatment options. It also includes insights into various FDA-approved levothyroxine variations and naturals that provide both T4 and T3 hormones.
View More