Torsades de Pointes: Causes, Risks, and Medications That Trigger It
When your heart’s electrical system gets disrupted, it can spiral into a life-threatening rhythm called torsades de pointes, a specific type of irregular heartbeat that appears as a twisting pattern on an ECG and can lead to sudden cardiac arrest. Also known as polymorphic ventricular tachycardia, it doesn’t come out of nowhere—it’s often tied to something you’re already taking, like a common antibiotic, antidepressant, or heart medication. This isn’t just a rare glitch. It’s a real, measurable risk tied to how your body handles certain drugs, especially if you already have a condition called long QT syndrome, a heart condition where the electrical recharge phase of the heartbeat takes too long, making the heart vulnerable to dangerous rhythms.
Torsades de pointes doesn’t care if you’re young or old—it just needs the right mix of triggers. Some people are born with a genetic form of long QT, but most cases are acquired from medications. Drugs like quinidine, erythromycin, citalopram, and even some anti-nausea pills can stretch out the QT interval on your ECG. That stretch might seem harmless, but in the wrong body, it’s like holding a rubber band too long—it snaps. And when it does, your heart stops pumping blood properly. You might feel dizzy, faint, or have no warning at all. The risk goes up if you’re female, have low potassium or magnesium, take more than one QT-prolonging drug, or have kidney or liver problems. These aren’t just medical terms—they’re real-world factors that affect millions.
What’s surprising is how often this is missed. Doctors don’t always check your QT interval before prescribing, and patients rarely know to ask. But the connection between meds and torsades is well-documented. For example, studies show that citalopram, a common antidepressant can cause dangerous QT prolongation at doses above 40mg. Same with levetiracetam, an epilepsy drug—rare, but possible. Even candesartan, a blood pressure pill, has been linked in isolated cases. The point isn’t to scare you—it’s to make you aware. If you’re on any medication for heart rhythm, depression, infection, or nausea, you deserve to know if it could be quietly affecting your heart’s timing.
Below, you’ll find real-world comparisons of medications that carry this risk, what alternatives exist, and how to spot the warning signs before it’s too late. No fluff. Just clear, practical info from people who’ve seen this happen—and how to avoid it.
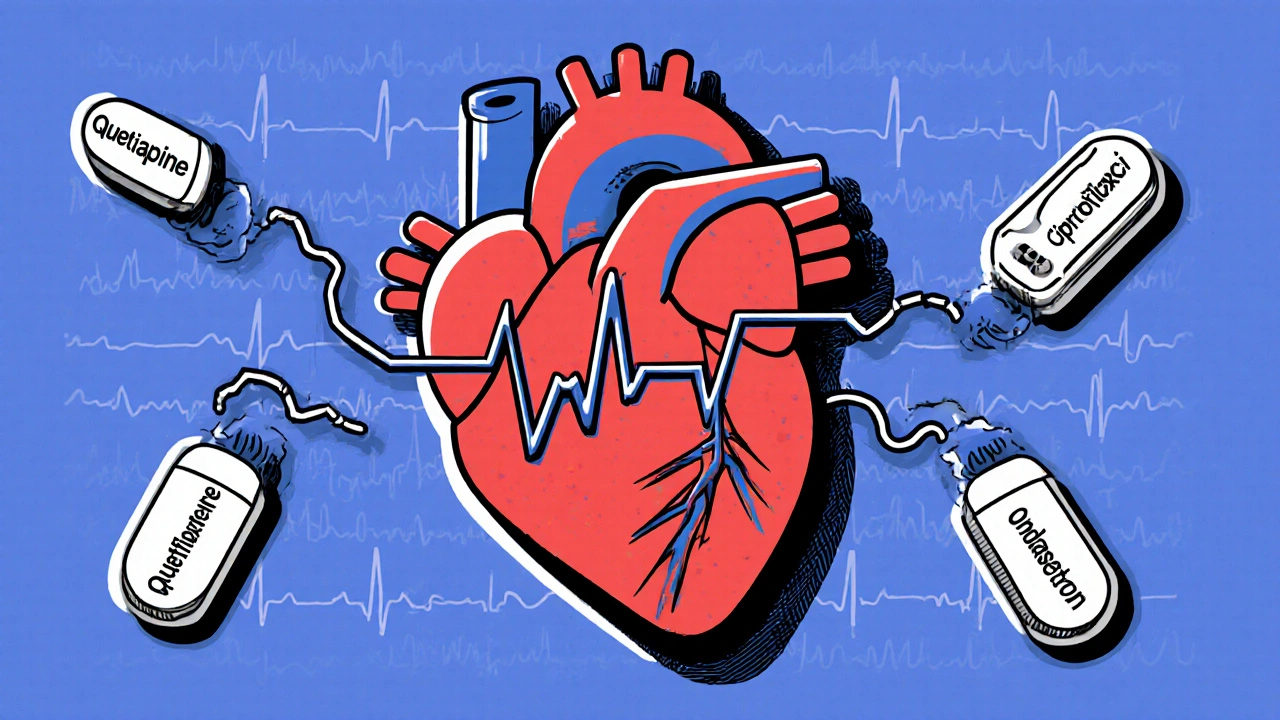
Antipsychotics and QT-Prolonging Drugs: What You Need to Know About Heart Risks
Combining antipsychotics with other QT-prolonging drugs can dangerously extend the heart's electrical cycle, raising the risk of life-threatening arrhythmias. Learn which meds are safest, who's most at risk, and how to prevent cardiac events.
View More