When you walk into a hospital or clinic and wait for hours just to see a doctor, it’s not just bad luck. It’s the result of a system breaking under the weight of its own shortages. Hospitals and clinics across the U.S. are struggling to keep doors open, staff beds, and deliver basic care-not because of a lack of patients, but because there aren’t enough healthcare workers to meet demand.
Why Hospitals Are Running on Empty
More than 193,000 nursing jobs open every year, and we’re not filling them. By 2030, the U.S. could be short over half a million registered nurses. That’s not a projection-it’s a countdown. The pandemic didn’t create this crisis. It exposed it. Nurses were already burning out before 2020. Now, nearly half of all nurses are over 50, and more than a third will retire in the next decade. Meanwhile, nursing schools can’t train enough new staff because there aren’t enough nursing professors to teach them. Over 8% of nursing faculty positions are empty right now.
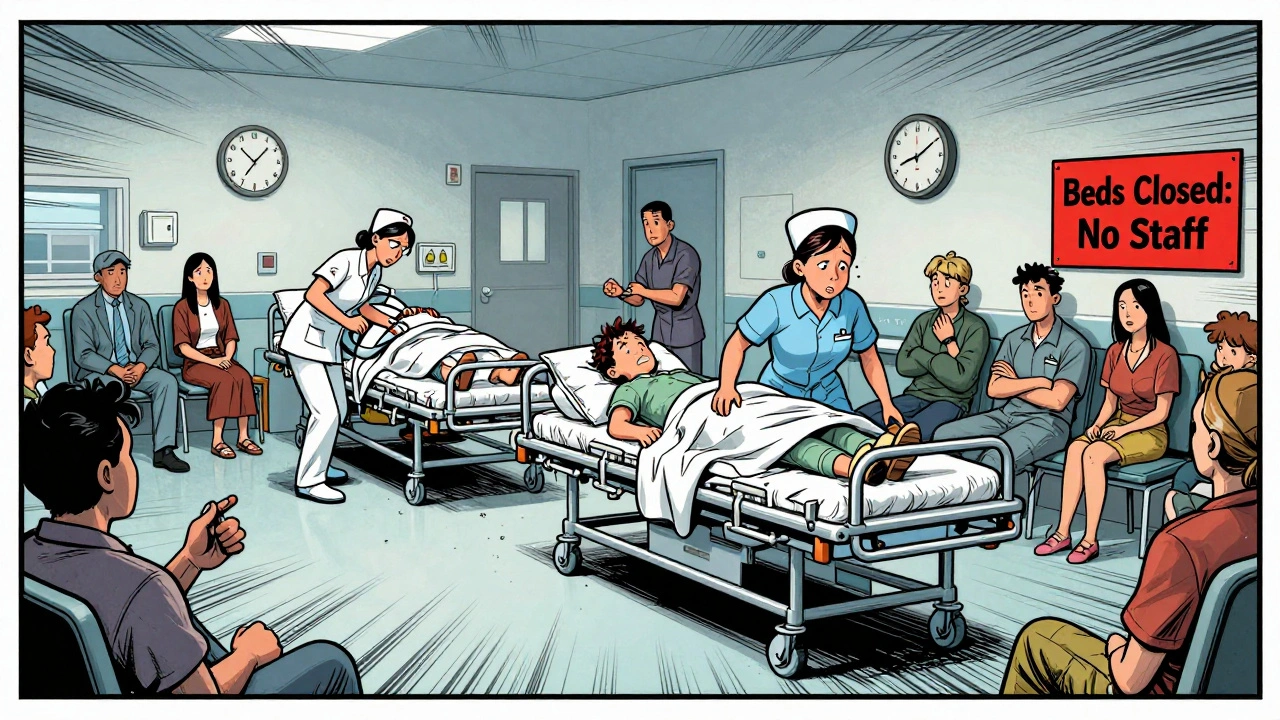
It’s not just nurses. Doctors are in short supply too. By 2036, the U.S. could face an 86,000-physician gap. Behavioral health providers? Even worse. Rural clinics are 37% more likely to have unfilled positions than urban ones. In places like Nevada and West Virginia, patients wait up to 72 hours in emergency rooms just to be seen. Some hospitals have had to close dozens of beds every week because they can’t staff them. One health system lost $4.2 million a month just from idle beds.
What Happens When There’s No One to Care
Staffing shortages don’t just mean longer waits. They mean deadlier care. Studies show that when a nurse is responsible for more than four patients, mortality rates jump by 7%. In emergency rooms, understaffing leads to 22% longer wait times. These aren’t abstract numbers-they’re lives at risk. Nurses on Reddit and LinkedIn are sharing stories of working 16-hour shifts with 3:1 patient ratios. One ICU nurse said she had two near-miss medication errors last month because she was stretched too thin.
It’s not just safety. It’s dignity. Patients are being discharged early because there’s no one to monitor them. Elderly patients in long-term care are going days without help bathing or turning in bed. Mental health patients wait weeks for an appointment, if they get one at all. In 2024, 12,400 behavioral health positions went unfilled nationwide-up 37% from the year before.
Who’s Getting Hit the Hardest
The shortage isn’t spread evenly. Rural hospitals are running at 67% staffing levels. Urban outpatient clinics? Around 79%. That gap means someone living in a small town has a much harder time getting care than someone in a city. Even within cities, it’s uneven. Magnet-designated hospitals-those with better working conditions-have 4.2 hours of professional development per nurse each month. Non-Magnet hospitals? Just 1.1 hours. That’s not just about morale. It’s about retention. Nurses at low-support hospitals are 63% more likely to quit.
Travel nurses are filling the gaps-but at a cost. They earn up to $185 an hour in high-demand areas like New York City ICUs. Meanwhile, permanent staff make $65 an hour. That pay gap creates tension. It also drives up hospital costs by 34%. Some hospitals now spend more on temporary staff than on their entire payroll a decade ago.
Why Solutions Keep Falling Short
Everyone talks about fixing this. But most fixes are temporary. Loan forgiveness programs in states like Massachusetts helped reduce shortages to 8% below the national average. But federal funding for nursing education? Just $247 million a year-when $1.2 billion is needed. The Biden administration recently added $500 million for training, but that only covers 18% of what’s required.
Technology is being pushed as the answer. AI tools can help with documentation, scheduling, and remote monitoring. One pilot program cut ER visits by 19%. But these tools take months to implement. Staff need 32 hours of training just to use them. And 68% of hospitals can’t get their electronic health records to talk to each other, making telehealth harder to roll out. Licensing rules across states delay cross-state staffing by over 100 days on average.
Some hospitals are trying redesigns. Mayo Clinic spent 18 months and $4.7 million to restructure care teams. It worked-nurse turnover dropped 31%. But most clinics can’t afford that kind of investment. Independent clinics? Only 37% have any kind of formal retention plan.

The Numbers Don’t Lie
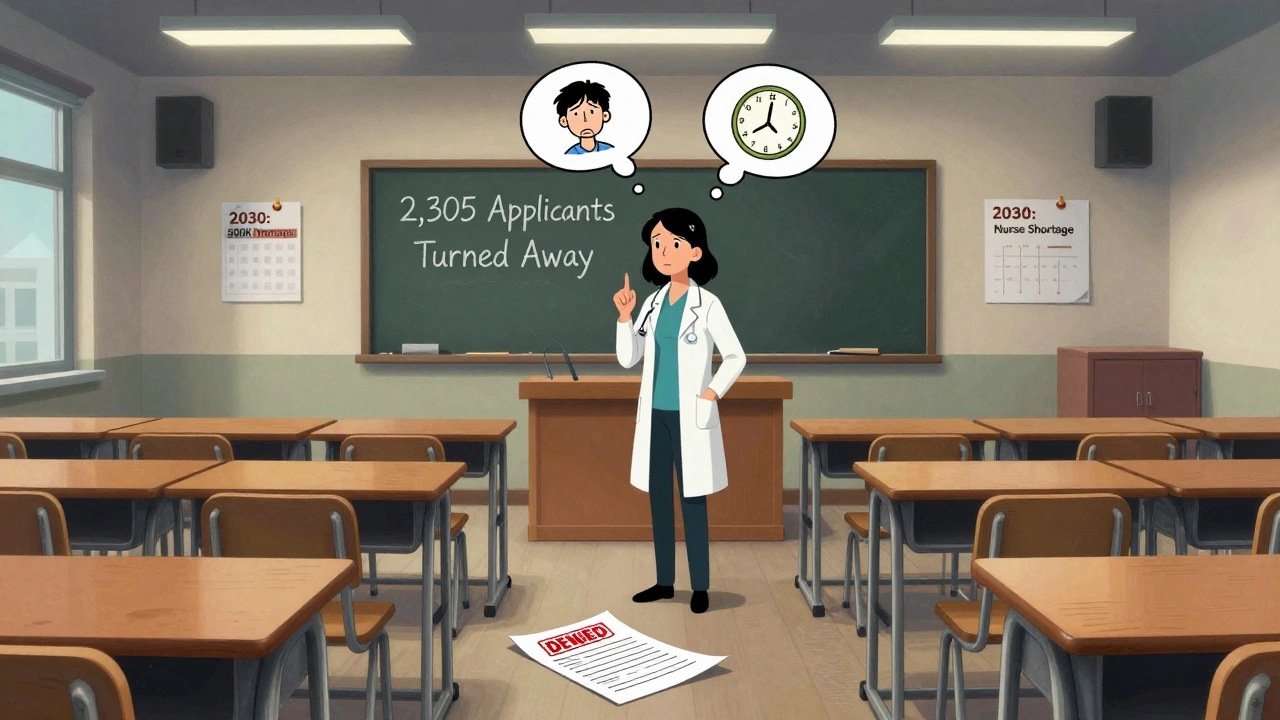
By 2030, 42 states will have nursing shortages. The U.S. population is aging fast. In 2023, there were 55.8 million Americans over 65. By 2050, that number will hit 82 million. But the number of working-age people supporting each senior is falling-from four to 2.9. That means fewer workers to care for more patients. And the pipeline isn’t keeping up. In 2023, nursing schools turned away 2,305 qualified applicants because they didn’t have enough teachers.
McKinsey says closing the global healthcare worker shortage could save 189 million years of life and add $1.1 trillion to the global economy. But right now, we’re treating symptoms, not the disease. Travel nurses, overtime, and AI tools aren’t solutions. They’re stopgaps.
What Needs to Change
We need to stop treating healthcare like a cost center and start treating it like infrastructure. That means:
- Investing $1.2 billion a year in nursing education-not $247 million.
- Removing state licensing barriers so nurses can move freely across state lines.
- Setting national nurse-to-patient ratios, like California’s 1:5 rule for medical-surgical units.
- Offering real retention programs: mental health support, predictable schedules, and career growth-not just bonuses.
- Using technology to reduce paperwork, not replace people.
Right now, hospitals are choosing between closing beds and overworking staff. Clinics are turning away patients because they can’t afford to hire. Patients are dying because care is delayed. This isn’t about politics or budgets. It’s about survival. If we don’t act now, the next time a crisis hits-whether it’s a pandemic, a heatwave, or a flu surge-we won’t just be overwhelmed. We’ll be unprepared.
Why are hospitals closing beds due to staffing shortages?
Hospitals close beds because they can’t safely staff them. Each bed requires a nurse, doctors, aides, and support staff. When there aren’t enough people to monitor patients, administer medications, or respond to emergencies, keeping beds open becomes a risk-not a service. Many hospitals now close 10-15 beds per week just to avoid putting patients and staff in danger.
Are travel nurses making the shortage worse?
They’re filling gaps, but they’re not solving the problem. Travel nurses make up 12% of hospital staffing, but they’re expensive-raising labor costs by 34%. Their high pay also creates resentment among permanent staff who earn far less. More importantly, they don’t stay long. Once the contract ends, the vacancy returns. They’re a band-aid, not a cure.
How do nurse-to-patient ratios affect patient outcomes?
Studies show that when a nurse cares for more than four patients, patient death rates rise by 7%. More patients means less time for monitoring, slower response to emergencies, and higher chances of medication errors. In states like California, where the ratio is capped at 1:5 for medical-surgical units, hospitals report lower infection rates and fewer patient complaints.
Why can’t we just hire more nurses?
We can’t hire more because we can’t train enough. Nursing schools have the space and funding to accept only so many students. But even when applicants are qualified, they’re turned away because there aren’t enough nursing professors. In 2023, over 2,300 qualified applicants were rejected for this reason. It’s a bottleneck at the source.
Is telehealth helping with staffing shortages?
In some cases, yes. Telehealth nurse triage has reduced ER visits by 19% in pilot programs. But it’s not a magic fix. It requires major tech investments, training, and interoperable systems-which 68% of hospitals still lack. Plus, telehealth can’t replace physical exams, emergency care, or bedside support. It helps with access, but not with the core staffing crisis.
What’s the long-term outlook for healthcare staffing?
Without major changes, the shortage will keep growing. The U.S. nursing shortage could last until 2035. The global shortage of healthcare workers is expected to peak at 15 million by 2027. The only way to reverse this is through serious investment in education, fair wages, better working conditions, and removing bureaucratic barriers. Otherwise, the system will keep getting slower, more dangerous, and less accessible.
14 Comments
Jennifer Patrician
December 7, 2025 at 13:11 PM
You think this is bad? Wait till the AI bots start replacing nurses entirely. They're already testing them in ER triage. No sleep. No union. No pay. Just cold algorithms deciding who lives.
aditya dixit
December 8, 2025 at 18:10 PM
The root issue isn't just numbers-it's the devaluation of care as a human act. When we treat healthcare like a supply chain, we forget that healing requires presence, not just procedure. The system rewards efficiency over empathy, and that's why it's collapsing.
Norene Fulwiler
December 9, 2025 at 23:14 PM
I worked as a med tech in rural Ohio. We had one RN for 18 patients on a good day. People died waiting for a bed that wasn't staffed. This isn't theory. This is my life.
William Chin
December 11, 2025 at 03:12 AM
It is imperative that we recognize the structural deficiencies within the current healthcare paradigm. The absence of standardized national protocols for staffing constitutes a fundamental failure of governance.
Deborah Jacobs
December 12, 2025 at 08:08 AM
I saw a nurse cry in the break room last week because she had to choose which of her five patients got the pain med first. She didn't say it out loud. But the way her hands shook... you could feel the whole system breaking inside her.
Lucy Kavanagh
December 13, 2025 at 15:04 PM
The NHS in the UK had this figured out. We didn't let corporations run hospitals. Now we're copying their mess. Why? Because someone in DC gets kickbacks from private equity firms buying up clinics. It's not incompetence. It's corruption.
Chris Brown
December 13, 2025 at 19:26 PM
This is what happens when you abandon moral responsibility in favor of fiscal pragmatism. The decline of American healthcare is not accidental. It is the logical endpoint of a society that no longer values life above profit.
Stephanie Fiero
December 15, 2025 at 01:51 AM
my friend works at a hospital and they just started using chatbots to answer patient questions. like... what if someone is having a heart attack and the bot says 'try drinking water'? this is not a joke. theyre cutting corners so hard its scary
Laura Saye
December 15, 2025 at 12:45 PM
The systemic underinvestment in human capital within the healthcare ecosystem reflects a broader ontological misalignment between commodification and care. The latent potential for resilience is present, yet it remains unactualized due to institutional inertia and epistemic neglect.
Michael Dioso
December 15, 2025 at 21:55 PM
You think travel nurses are the problem? Nah. The problem is you. You voted for politicians who cut funding for nursing schools and then complained when your grandma waited 12 hours for a bed. Fix your damn priorities.
Krishan Patel
December 17, 2025 at 17:15 PM
The solution is simple: abolish state licensing. Let nurses move freely. Let them earn fair wages. Let them teach without being exploited. The bureaucracy is the disease. Not the nurses. Not the patients. The system.
Carole Nkosi
December 18, 2025 at 00:34 AM
In South Africa we have no nurses. No meds. No hope. You think your crisis is bad? Look around. This isn't America's problem. It's the world's. And no one cares until it's their mom in the ER.
Ada Maklagina
December 18, 2025 at 22:48 PM
They close beds because they can't afford to keep the lights on if they don't have staff. It's not a choice. It's math.



sean whitfield
December 5, 2025 at 13:20 PM
They don't want you to know this but hospitals are being starved on purpose so you'll rely on private clinics. The real crisis? Profit margins. Nurses are just the collateral damage.