
When a vertebra in your spine cracks under pressure - often from osteoporosis, a fall, or cancer - the pain can be crushing. Standing, sitting, even breathing becomes unbearable. For many older adults, this isn’t just discomfort; it’s a life-altering event. That’s where kyphoplasty and vertebroplasty come in. These aren’t big open surgeries. They’re quick, minimally invasive procedures that can turn your pain from an 8 out of 10 down to a 2 in just hours. And most people walk out the same day.
What Exactly Are Kyphoplasty and Vertebroplasty?
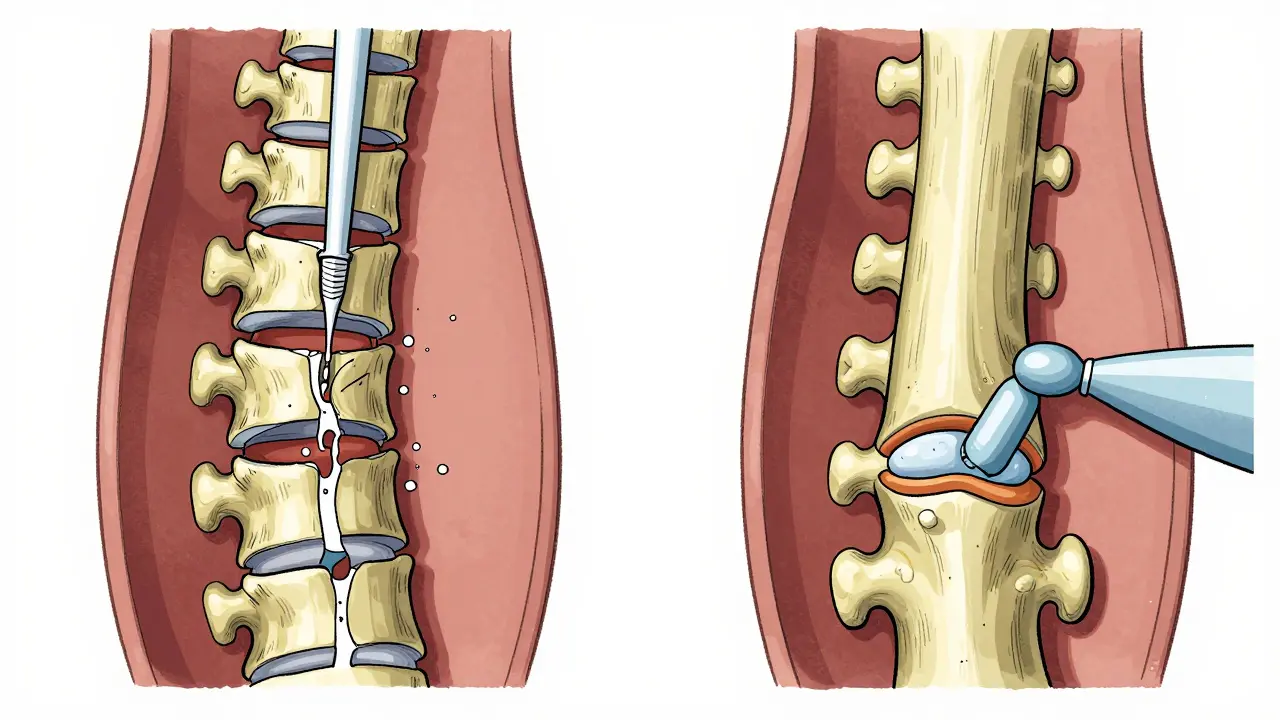
Both procedures fix broken vertebrae by injecting medical-grade bone cement into the damaged bone. Think of it like filling a cracked concrete block with strong epoxy. The cement hardens quickly, locking the fracture in place and stopping the pain. But here’s the key difference: vertebroplasty injects the cement directly into the fracture. Kyphoplasty first uses a tiny balloon to lift the collapsed bone back up before filling it.
Vertebroplasty started in France in the 1980s. Doctors noticed that injecting cement into a painful, broken spine bone made the pain vanish. It was simple, fast, and worked. Kyphoplasty came later - in the late 1990s - as an upgrade. Instead of just stuffing cement in, surgeons began inflating a small balloon inside the broken bone to restore its height before adding the cement. This wasn’t just about pain relief; it was about fixing the hunched back that often comes with these fractures.
How the Procedures Work - Side by Side
Both start the same way. You lie face down. A small needle is guided through your skin into the fractured vertebra using real-time X-ray imaging. Local anesthesia numbs the area, and you’re given light sedation so you’re relaxed but awake.
In vertebroplasty, the cement - polymethylmethacrylate (PMMA) - is pushed directly into the fracture under pressure. It flows through the spongy bone inside the vertebra, filling cracks and gaps. The whole thing takes 30 to 60 minutes. You’re usually home the same day.
In kyphoplasty, after the needle is in place, a balloon is threaded in and carefully inflated. It’s like gently propping up a collapsed box. The balloon lifts the broken bone back toward its original shape. Once the height is restored, the balloon is popped and removed. Then, the cement is injected into the space the balloon created. This cavity helps control where the cement goes, reducing the chance it leaks out.
Both use the same cement. Both use the same kind of X-ray guidance. Both cost a lot less than traditional spinal fusion surgery, which requires weeks of recovery and hospital stays.
Which One Is Better? Pain Relief, Height Restoration, and Risk
Here’s what most patients care about: will it stop the pain? Will I stand straighter? Is it safe?
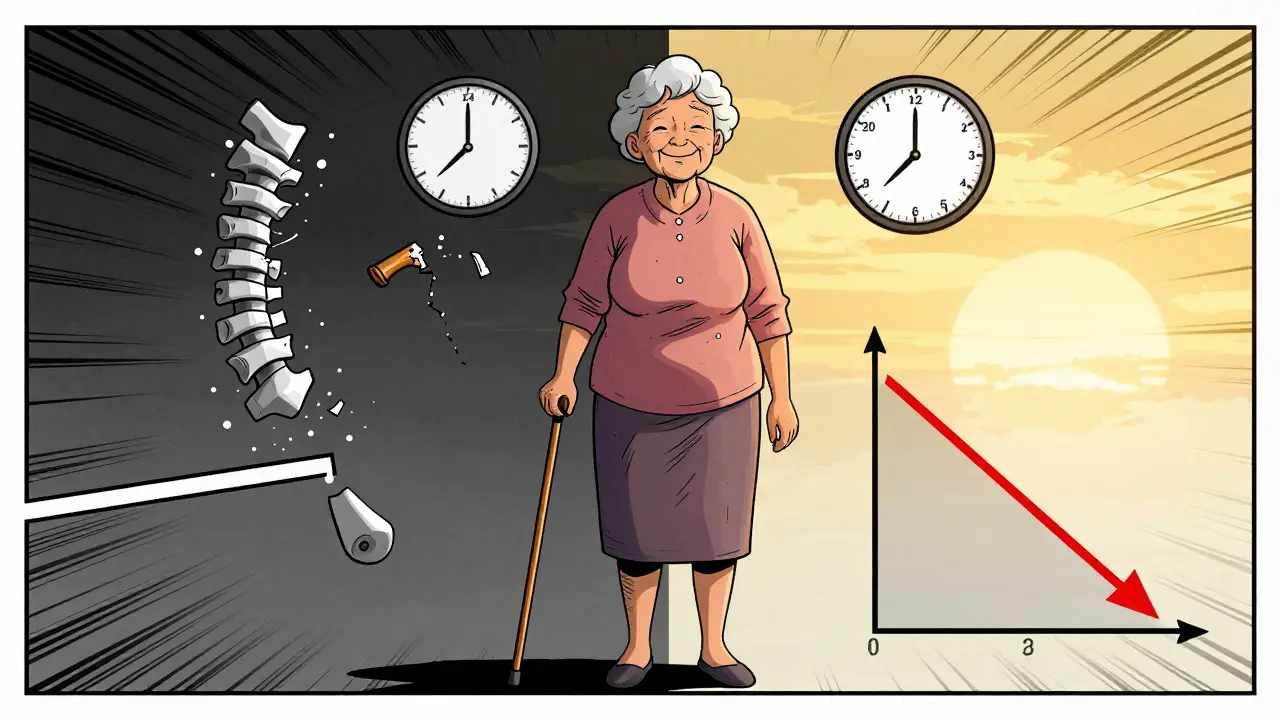
Pain relief is nearly identical between both. Studies show 85-90% of patients report immediate, dramatic pain reduction after either procedure. Before treatment, average pain scores are around 8.2 out of 10. Within 24 hours, they drop to 1.5. That’s not a small improvement - it’s life-changing.
Height restoration is where kyphoplasty shines. On average, it restores 40-60% of lost vertebral height. Vertebroplasty? Almost none. But here’s the catch: that restored height doesn’t last forever. Studies show about 30% of the height gained from kyphoplasty is lost within a few years as the bone settles. Still, for many, even temporary straightening means better posture, less pressure on other spine bones, and improved breathing.
Risk of cement leakage is the biggest safety concern. In vertebroplasty, cement leaks out of the bone in 27-68% of cases. Most leaks cause no problems, but if it hits a nerve or the spinal cord, it can be serious. Kyphoplasty reduces this risk to 9-33% because the balloon creates a controlled space for the cement. Symptomatic complications - like a cement clot blocking a lung artery - happen in about 1.1% of vertebroplasty cases and 0.6% of kyphoplasty cases.
Cost, Insurance, and Who Gets Which Procedure
Kyphoplasty costs 20-30% more than vertebroplasty. In the U.S., Medicare pays about $3,850 for kyphoplasty and $2,950 for vertebroplasty. That price difference matters - especially in systems where hospitals and doctors are paid by the procedure.
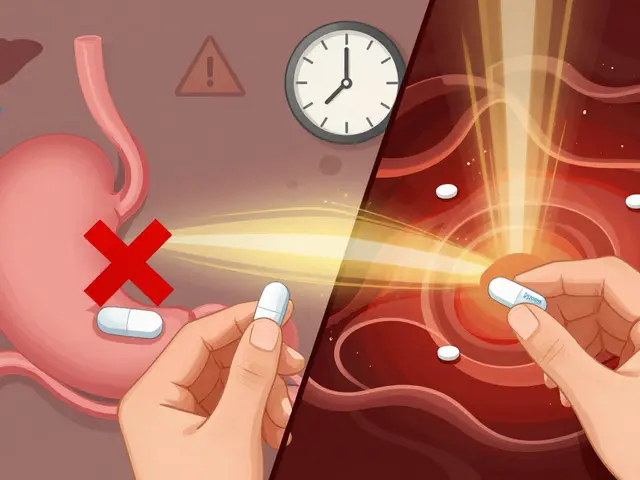
Insurance - including Medicare - covers both if you’ve tried conservative care first: at least 4-6 weeks of pain meds, physical therapy, or a back brace. Approval rates are above 95% when the paperwork is clear.
So who gets which? Doctors pick based on the fracture:
- If your spine is badly collapsed - more than 30% height loss, or you have a noticeable hunch - kyphoplasty is usually preferred.
- If the fracture is stable, not severely deformed, and you just need pain relief, vertebroplasty is often enough.
- For older patients with very weak bones, kyphoplasty’s lower leakage risk makes it the safer choice.
Real Patient Experiences
On patient forums, stories are powerful. One woman in her 70s, who couldn’t get out of bed after a fall, had kyphoplasty and said, “I went from 9/10 pain to 2/10 within hours. I cried because I could finally breathe.”
Another man had vertebroplasty. His pain dropped from constant 7/10 to occasional 3/10. But he still had his hunched posture. “It helped me live,” he wrote, “but I’m still bent over.”
Most people go home the same day. 92% return to normal activities within 72 hours. About 75% stop using opioid painkillers within a week.
But it’s not magic. About 10-15% of patients still have pain afterward. And in 5-10% of cases, another vertebra breaks within a year. That’s not because the procedure failed - it’s because osteoporosis is still active. The cement fixed one bone, but the disease didn’t go away.
What Happens After the Procedure?
You’ll be monitored for 4-6 hours after the procedure. You might feel sore at the needle site, but that fades in a day or two. You’re told to avoid heavy lifting or twisting for 24 hours. After that, you can walk, drive, and gradually return to daily life.
But here’s the critical part: you still need to treat the root cause - osteoporosis. If you don’t, you’re at high risk for another fracture. Your doctor will likely start you on calcium, vitamin D, and medications like bisphosphonates or denosumab. Physical therapy to strengthen your back and core muscles is also essential.
What’s New in 2026?
The field is evolving. New cement formulas - like calcium phosphate - are being used because they bond better with natural bone and generate less heat during hardening. In March 2023, Medtronic got FDA approval for an updated kyphoplasty balloon system that’s easier to control.
A major 2023 study in The Lancet found that if you do either procedure within two weeks of the fracture, you reduce your risk of dying within a year by nearly 30%. That’s huge. It means these aren’t just pain treatments - they’re life-saving interventions.
Right now, kyphoplasty makes up about 65% of all vertebral fracture procedures in the U.S. But analysts predict that number will rise to 75% by 2028. Why? Because even though it costs more, it’s safer, and patients prefer it. The market for these procedures is growing fast - expected to hit $2.17 billion by 2029 - mostly because the population is aging. One in four women over 50 will get a spinal fracture. By 2035, that number could jump 50%.
Final Thoughts: Choosing the Right Path
There’s no single “best” procedure. Both kyphoplasty and vertebroplasty are proven, effective, and safe for the right patients. If your spine is severely collapsed and you want to stand taller, kyphoplasty gives you the best shot. If your fracture is stable and you just need the pain to stop, vertebroplasty is just as effective - and cheaper.
The real win isn’t the tool. It’s the outcome: getting back your life. No more lying down because you can’t stand. No more fear of a fall. No more painkillers that make you foggy. These procedures don’t cure osteoporosis, but they give you the strength to fight it.
If you or someone you love is suffering from a spinal fracture, ask your doctor: Is this fracture recent? Is there height loss? What’s my risk of cement leakage? What’s the plan for my bones after this? The answer might be simpler than you think - and the relief could be faster than you imagine.
8 Comments
Jay Clarke
January 19, 2026 at 03:05 AM
Let me tell you something - I had vertebroplasty last year. Pain went from 'I can’t breathe' to 'I can finally hug my grandkids' in 2 hours. No balloon, no fancy tech, just cement and a miracle. People act like kyphoplasty is some kind of luxury spa treatment. Nah. It’s just a more expensive version of the same thing. The body doesn’t care if the cement went in with a balloon or a syringe. It just wants the pain to stop. 🙏
Eric Gebeke
January 19, 2026 at 09:41 AM
Of course the medical-industrial complex loves kyphoplasty - it’s 30% more expensive. You think the balloon is about patient care? Nah. It’s about profit margins. Hospitals get paid more, surgeons get bonuses, and you? You’re just a walking insurance claim. And don’t even get me started on how they push this on elderly patients who don’t know any better. It’s predatory. They don’t fix osteoporosis - they just slap a Band-Aid on it and bill you $4K. 🤑
Ryan Otto
January 20, 2026 at 02:53 AM
Interesting how the narrative conveniently ignores the geopolitical angle. The U.S. leads in these procedures because it’s the only country where healthcare is structured as a profit-driven auction. In Canada, they wait. In Germany, they use physical therapy first. Here? We inject cement like it’s a fast-food combo. And yet, we’re the 'healthcare superpower'? More like a medical carnival. The real tragedy isn’t the fracture - it’s the system that monetizes suffering. 🌍💸
Robert Cassidy
January 21, 2026 at 11:43 AM
Look, I get it - you want to stand tall again. But here’s the truth nobody tells you: after these procedures, your spine is still a ticking time bomb. Osteoporosis doesn’t care if you’ve got cement in there. You’re still weak. You’re still brittle. And guess what? The next fracture? It’s gonna be worse. They don’t fix the disease. They just patch the symptom. And then they charge you for the patch. This isn’t medicine - it’s damage control for a broken system. 🤬
Dayanara Villafuerte
January 22, 2026 at 15:26 PM
OMG I had kyphoplasty last year and I’m basically a new person 😭 I went from crawling to dancing at my daughter’s wedding! The balloon thing? Total game-changer. I could finally breathe without feeling like a caved-in taco 🌮✨ Also, my ortho said the new calcium phosphate cement is like magic - bonds to bone like Velcro. And yes, I’m still on my bisphosphonates. Don’t skip the meds, people. This ain’t a one-and-done fix. 💪❤️
Andrew Qu
January 22, 2026 at 19:00 PM
For anyone considering this - don’t rush. Get a second opinion. Make sure your fracture is recent (under 2 weeks) if you want the best results. And please, please - talk to a bone specialist about osteoporosis meds. These procedures are amazing, but they’re not a cure. I’ve seen too many patients come back with another fracture because they thought the cement 'fixed everything.' It doesn’t. You still have to fight the disease. Stay strong. You got this. 💪
Jodi Harding
January 24, 2026 at 11:59 AM
They both work. Cement fixes pain. Balloon fixes posture. Pick your priority. 🤷♀️





Pat Dean
January 18, 2026 at 01:27 AM
This whole 'minimally invasive' crap is just Big Pharma’s way of keeping seniors hooked on procedures instead of fixing the real problem: their shitty diets and lack of movement. You think cement in your spine is the answer? Try eating real food and lifting weights before you let some surgeon pump plastic into your bones. I’ve seen 80-year-olds do pull-ups - you’re telling me we need this nonsense? 🤡