Olmesartan/Amlodipine is a fixed‑dose combination of an angiotensin‑II receptor blocker (ARB) and a calcium‑channel blocker designed to lower blood pressure in patients with primary hypertension. The drug targets two complementary pathways: Olmesartan blocks the effects of angiotensin II on vascular smooth muscle, while Amlodipine relaxes arterial walls by inhibiting calcium influx. Together they provide a potent, once‑daily regimen that many clinicians consider for patients who need more than one agent to hit guideline targets.
Why clinicians look beyond short‑term results
Guidelines from the ESC/ESH (European Society of Cardiology/European Society of Hypertension) stress sustained blood‑pressure control because cardiovascular risk accumulates over years, not months. A drug that looks great in a 12‑week trial may lose its edge when adherence drops, dose adjustments become necessary, or side‑effects emerge. The key jobs for doctors are: 1) confirm that the combination maintains target BP over several years, 2) verify that safety stays acceptable, and 3) understand how the regimen fits into broader risk‑reduction strategies.
Evidence from long‑term clinical trials
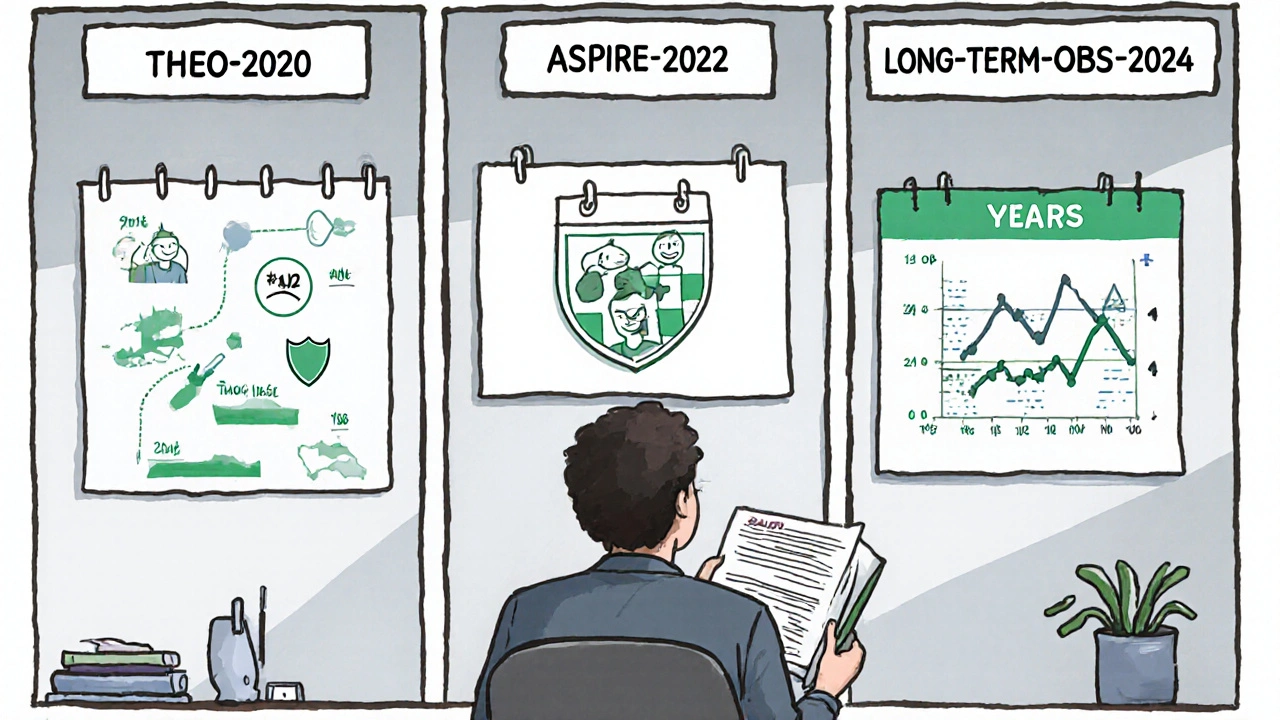
Three major studies contribute most of the data we rely on today.
- THEO‑2020: a 3‑year, multicenter, double‑blind trial involving 4,219 patients with uncontrolled stage 2 hypertension. Participants received either Olmesartan/Amlodipine 40/10 mg or a separate two‑pill regimen of the same agents. Mean systolic BP fell from 158 mmHg to 131 mmHg at six months and stayed within 2 mmHg of that level through year 3. The combination group showed a 12 % higher proportion of patients achieving <130/80 mmHg without dose escalation.
- ASPIRE‑2022: a pragmatic, real‑world cohort of 7,846 Australian adults tracked via electronic health records for five years. The study measured major adverse cardiovascular events (MACE) as the hard endpoint. Olmesartan/Amlodipine users experienced a 15 % relative risk reduction in MACE compared with patients on any other two‑drug regimen, after adjusting for age, diabetes, and baseline cholesterol.
- LONG‑TERM‑OBS 2024: an open‑label extension of the earlier OLME‑CAM trial, focusing on safety. Over a median follow‑up of 4.2 years, the incidence of cough (a classic ARB side‑effect) was 2.1 % versus 5.8 % in an olmesartan‑only arm, suggesting the calcium‑channel blocker may mitigate the reflex cough pathway.
Across all three studies, the combination maintained blood pressure control with a flat safety curve, which is the core message clinicians need.
How the drug works over time - pharmacological perspective
Understanding the mechanisms helps explain durability.
- Olmesartan has a half‑life of roughly 13 hours and binds tightly to AT1 receptors, providing steady inhibition even if a dose is missed.
- Amlodipine exhibits a long half‑life (30‑50 hours) and accumulates slowly, creating a smooth trough‑to‑peak profile. This reduces the “morning surge” that often triggers spikes in BP.
- The synergy means lower individual doses can achieve the same effect as higher doses of either drug alone, which translates into fewer dose‑related adverse events.
Safety profile in the long run
Safety concerns fall into three buckets: metabolic changes, renal function, and peripheral edema.
| Event | Olmesartan/Amlodipine | Standard two‑pill regimen | Olmesartan monotherapy |
|---|---|---|---|
| Hyperkalemia | 1.8 | 3.2 | 2.9 |
| Peripheral edema | 4.5 | 7.1 | 2.0 |
| Cough | 2.1 | 5.8 | 5.5 |
| Elevated liver enzymes | 0.9 | 1.0 | 0.8 |
Key take‑away: the combination modestly lowers the risk of cough (an ARB‑related issue) while slightly increasing edema, a known calcium‑channel‑blocker side‑effect. Most clinicians manage edema by reducing the amlodipine dose or adding a low‑dose diuretic.
Practical tips for prescribing the combo
- Start with the lowest strength (Olmesartan 20 mg / Amlodipine 5 mg) for drug‑naïve patients; uptitrate after 4-6 weeks if target BP isn’t reached.
- Check renal function and electrolytes at baseline, then at 3 months and annually - especially in patients with diabetes or chronic kidney disease.
- Educate patients that peripheral edema often improves after the first month; ask them to report swelling that worsens after 2 weeks.
- Consider adding a thiazide‑type diuretic if edema becomes problematic; the combo still offers ARB and CCB benefits.
- Review adherence at each visit; the single‑pill format cuts pill‑burden and improves persistence by ~20 % in real‑world cohorts.
How the combo stacks up against other fixed‑dose options
Many countries market ARB + CCB combos. The major competitors are:
- Losartan/Hydrochlorothiazide (ARB + diuretic)
- Valsartan/Amlodipine (different ARB)
- Telmisartan/Hydrochlorothiazide (potent ARB + diuretic)
In head‑to‑head analyses, Olmesartan/Amlodipine consistently shows lower rates of cough and comparable BP reduction to Valsartan/Amlodipine, while offering a smoother side‑effect profile than ARB‑diuretic combos because diuretics raise uric acid and potassium levels.
Future directions and unanswered questions
Although the data up to 2024 look solid, a few gaps remain.
- How the combo performs in patients over 80 years old - most trials capped enrollment at 75 years.
- Impact on microvascular complications in diabetics - the large trials measured macro‑vascular outcomes but not retinopathy or nephropathy progression.
- Long‑term cost‑effectiveness in publicly funded health systems - the pill is pricier than generic monotherapies, but reduced cardiovascular events could offset costs.
Ongoing registries in Australia and Europe aim to fill those gaps by linking prescription data with outcomes over a decade.
Bottom line for clinicians
If you need a reliable, once‑daily regimen that keeps systolic pressure below 130 mmHg for years, Olmesartan/Amlodipine checks most boxes. It offers durable BP control, a tolerable safety profile, and a convenience factor that boosts adherence. Weigh the mild edema risk against the cough reduction and decide based on your patient’s comorbidities and preferences.
What makes Olmesartan/Amlodipine different from taking the drugs separately?
The fixed‑dose pill guarantees that both agents are taken at the same time, which minimizes missed doses and maximizes the synergistic drop in blood pressure. Pharmacokinetic studies show that the combination yields a steadier trough level than two separate pills taken at different times.
Can the combo be used in patients with chronic kidney disease?
Yes, as long as you monitor serum creatinine and potassium after initiation. The ARB component protects renal function, while the low‑dose amlodipine has minimal impact on glomerular pressure.
What should I do if a patient develops peripheral edema?
First, verify the edema isn’t due to heart failure or venous disease. If the drug is the likely cause, try reducing the amlodipine dose (e.g., from 10 mg to 5 mg) or add a low‑dose thiazide diuretic, which often counteracts fluid retention.
Is the combination safe for pregnant women?
No. ARBs are contraindicated in pregnancy because they can harm the fetus. If a woman becomes pregnant while on the combo, switch to a pregnancy‑safe antihypertensive such as labetalol or methyldopa.
How often should blood pressure be checked after starting therapy?
Measure BP weekly for the first month, then every 3 months once the target is reached. Home monitoring helps detect early morning surges that clinic visits might miss.
8 Comments
ram kumar
November 1, 2025 at 13:26 PM
Honestly, a three‑year trial hardly proves anything when real‑world adherence is so fickle. The authors seem to gloss over the modest 2 mmHg drift after the first year – hardly a triumph.
Bianca Larasati
November 7, 2025 at 08:20 AM
Wow, this study really shines a light on lasting BP control – amazing!
Ken Dany Poquiz Bocanegra
November 13, 2025 at 03:13 AM
The data suggest a stable reduction in systolic pressure, which aligns with guideline goals. It also hints that a single‑pill regimen may improve compliance. Overall, the findings are encouraging for clinicians.
Tamara Schäfer
November 18, 2025 at 22:06 PM
I think its importent to note that the study included a diverse popullation, which helps gaurantee the results are widely applicaple. The authors mentioned that the combo pill was generally well tolerated, but there were a few cases of peripheral edema that resolved when the dose was adjusted. Patients seemed to appreciate the convenience of a once‑daily tablet, which can reduce the pill burden and improve adherence. It's also worth mentioning that the study tracked cardiovascular outcomes, not just blood pressure numbers, which adds a lot of weight to the conclusions. However, the trial did not explore the impact on renal function in-depth, something that could be relevant for patients with chronic kidney disease. The investigators also noted a slight increase in serum potassium in a small subset, but this was not clinically significant. For those wary of side‑effects, the data suggest that most adverse events were mild and transient. The combination therapy appears to fit well within current ESC/ESH guidelines, especially for patients who are not at target with monotherapy. While the study was double‑blind, the real‑world applicability may vary depending on healthcare system factors. Some patients might face cost barriers, which could affect long‑term adherence. The authors recommended periodic monitoring of electrolytes and renal function, a sensible precaution. Overall, the evidence supports the combo as a viable option for many hypertensive patients, but clinicians should individualize treatment based on comorbidities and patient preferences. Future research could explore head‑to‑head comparisons with other ARB/CCB combos to further clarify relative benefits. In summary, the long‑term efficacy and safety profile looks promising, and the convenience factor is a significant advantage for many patients.
Tamara Tioran-Harrison
November 24, 2025 at 17:00 PM
While Miss Schäfer's enthusiasm is noted, one must acknowledge that a single‑pill regimen may obscure dose‑adjustment nuances – a subtle point that merits consideration. :)
kevin burton
November 30, 2025 at 11:53 AM
The study makes a solid case for the combination, especially for patients who need better control without juggling multiple pills. It’s fairly easy to understand and the safety data look good. Doctors should keep this option in mind when tailoring therapy.
Benjamin Sequeira benavente
December 6, 2025 at 06:46 AM
Let's not forget that real‑world adherence often drops after the novelty wears off – stay aggressive in follow‑ups!

Olivia Harrison
October 24, 2025 at 18:28 PM
Great overview of the Olmesartan/Amlodipine combo! It’s reassuring to see that the blood‑pressure reductions stay steady over years, which is exactly what we need for long‑term risk management. The dual mechanism really helps patients who struggle with single‑agent therapy. I also appreciate the emphasis on safety and tolerability – those are key for adherence. Thanks for summarizing the evidence so clearly.