Healthcare Worker Crisis: Why Staff Shortages Are Putting Medications and Lives at Risk
When the healthcare worker crisis, a severe shortage of nurses, doctors, and support staff that’s overwhelming hospitals and clinics across the country. Also known as staffing shortage, it’s not just a backlog of appointments—it’s a direct threat to how safely medications are given, monitored, and managed. Every time a nurse is responsible for twice as many patients as recommended, every time a pharmacist works double shifts without a break, and every time a doctor skips a follow-up because they’re juggling 30 more patients than they should, the risk of a medication error goes up. This isn’t hypothetical. Studies from the Institute of Medicine show that over 1.5 million Americans are injured each year by preventable medication mistakes—and a huge chunk of those happen because staff are stretched too thin.
The nurse shortage, a critical gap in frontline care where over 200,000 nursing positions remain unfilled in the U.S. alone doesn’t just mean longer wait times. It means someone taking lithium for bipolar disorder might not get their blood levels checked on time, increasing the chance of lithium toxicity. It means a diabetic patient with hypoglycemia symptoms gets missed because the nurse can’t check every room. It means a patient on anticoagulants might not get their dose adjusted after a kidney test because the pharmacy tech is covering for three absent colleagues. The physician burnout, the emotional and physical exhaustion affecting nearly half of all doctors, leading to decision fatigue and higher error rates makes this worse. When you’re mentally drained, you’re more likely to overlook a dangerous drug interaction—like mixing NSAIDs with lithium, or adding a QT-prolonging drug to an antipsychotic regimen.
The healthcare system strain, the cumulative pressure from aging populations, chronic disease spikes, and underfunded infrastructure isn’t going away. And it’s not just about hiring more people—it’s about fixing the systems that make the job unbearable. When pharmacists are forced to choose between verifying 50 prescriptions or spending 10 minutes counseling a patient on how to use an epinephrine auto-injector, someone loses. When a clinic runs out of staff and starts dispensing expired medications out of desperation, safety goes out the window. This crisis touches every post in this collection: from DMARDs for autoimmune disease to antidepressants and anticholinergics that can harm memory if not monitored closely. The people who keep you safe—nurses, pharmacists, technicians—are drowning. And when they’re overwhelmed, your meds become riskier.
What you’ll find below isn’t just a list of articles. It’s a map of how the healthcare worker crisis is quietly changing how medicines work—or fail to work—in real life. From dosing mistakes to missed side effects, these posts show you what’s really happening behind the scenes. And more importantly, what you can do to protect yourself when the system is falling apart.
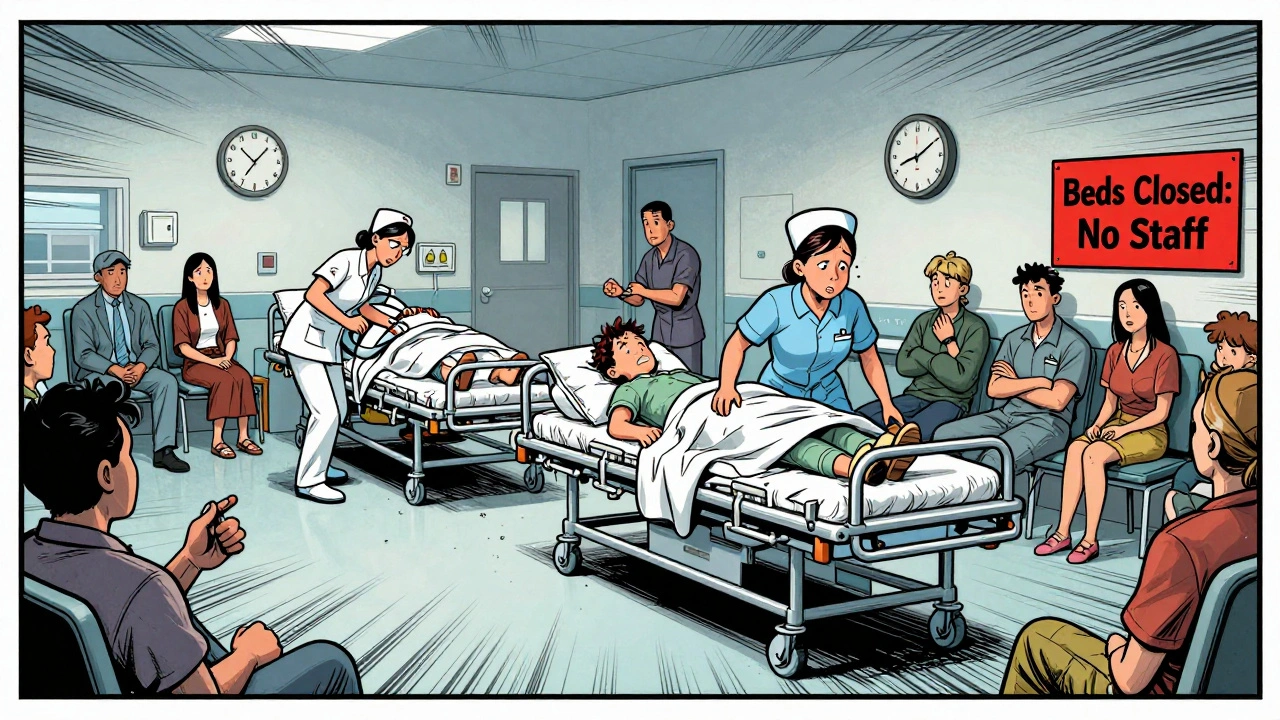
Healthcare System Shortages: How Hospital and Clinic Staffing Crises Are Hurting Patient Care
Healthcare staffing shortages are forcing hospitals to close beds, extend wait times, and risk patient safety. With nurses retiring and schools unable to replace them, the system is reaching a breaking point.
View More